Abstract
Purpose of Review
Over the last 30 years, medical assistance in dying (MAiD) including euthanasia (EU) and physician-assisted death (or suicide, PAS) has become the center of a large debate, particularly when these practices have involved people with psychiatric illness, including resistant depression, schizophrenia, personality, or other severe psychiatric disorders. We performed a review utilizing several databases, and by including the most relevant studies in full journal articles investigating the problem of MAiD in patients with psychiatric disorders but not in physical terminal conditions (non-terminal, MAiD-NT).
Recent Findings
Literature has shown that a small percentage of people with psychiatric disorders died by MAiD-NT in comparison with patients with somatic diseases in terminal clinical conditions (e.g., cancer, AIDS). However, the problem in the field is complex and not solved yet as confirmed by the fact that only a few countries (e.g., the Netherlands, Belgium, Luxemburg) have legalized MAiD-NT for patients with psychiatric disorders, while most have maintained the practices accessible only to people with somatic disease in a terminal phase. Also, how to make objective the criterion of irremediability of a mental disorder; how to balance suicide prevention with assisted suicide; how to avoid the risk of progressively including in requests for MAiD-NT vulnerable segments of the population, such as minors, elderly, or people with dementia, in a productive-oriented society, are some of the critical points to be discussed.
Summary
The application of MAiD-NT in people with psychiatric disorders should be further explored to prevent end-of-life rights from contradicting the principles of recovery-oriented care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last 30 years, death with dignity has been a part of a large thematic discussion regarding hastening the patient’s death to put an end to their suffering, when no cure can be found such as patients in terminal stages of a somatic disease (e.g., advanced cancer, AIDS, amyotrophic lateral sclerosis). This topic, often subsumed under the rubric of medical assistance in dying (MAiD), namely, euthanasia (EU) and physician-assisted death (or physician-assisted suicide, PAS), has involved several areas of medicine, especially palliative medicine (Table 1 for definitions).
Gradually, starting from the Dutch experience dating almost 30 years back [1], these practices have been extended in some countries to people that are not terminally ill because of a somatic disease, but are affected by non-terminal conditions(MAiD-NT), including psychiatric disorders (e.g., depression, schizophrenia) or major neurocognitive disorders (e.g., dementia). The legislation in these jurisdictions is not identical, although some criteria are the same: the non-terminal condition should be refractory, resistant to treatment or untreatable, making the patients’ quality of life poor, and causing unbearable suffering (Table 2) [2•].
The aims of the present critical review are (i) to examine and discuss the most significant issues related to this area, including the complexity of the definition of clear-cut and stringent criteria for and the moral issues involved in MAiD-NT when comparing patients with physical or mental disorders; (ii) to summarize the most relevant data concerning the problem of MAiD-NT among patients with psychiatric disorders, attitudes, and views of health care professionals, patients and caregivers, and epidemiological data.
Methods
A search was made of the major databases over the last 10 years (Embase/Medline, PsycLIT, PsycINFO, the Cochrane Library) from January 2011 to June 2021, by including the most relevant studies in full journal articles investigating MAiD-NT in patients with psychiatric disorders. The literature search was performed with the search terms (euthanasia[title] OR “assisted suicide*”[title] OR “assisted dying”[title] OR “physician assistance in dying”[title]) AND (psych* OR mental) with appropriate filters (abstract, humans, English).
Results
The analysis of the literature allowed us to extrapolate data on several topics, namely, the moral debate about MAiD-NT in psychiatry, the opinions, and attitudes about MAiD-NT in psychiatric settings, the epidemiological findings on MAiD-NT cases among patients with psychiatric disorders, and the impact of MAiD-NT on physicians.
The Moral Debate About MAiD-NT in Psychiatry and Unsolved Problems
The moral debate in the case of MAiD-NT in psychiatry is motivated by the observation that many key aspects of these practices as applied in patients in a terminal phase of a somatic disorder are not pertinent in those with psychiatric disorders. For example, withdrawing/withholding treatment, even if not part of MAiD, does not apply to psychiatry where the intervention requires action and not omission. Action in fact relates to all the intentional activities (doing) that a physician may perform (such as in MAiD), while omission relates to the intentional decision to not act (not doing or stop doing). More specific moral issues in MAiD-NT are supporting death hastening practices for patients whose underlying condition invokes a desire to die when their desire to die can be reinforced by lack of support, opportunity, and access to resources that results from their marked marginalization.
When discussing opinions about MAiD-NT for people with mental illness, two opposite positions emerge as follows: those who are explicitly against those practices in patients with psychiatric disorders and those who support them as morally acceptable, with different arguments against and in favor of the practices (Table 3 and Supplement Table 1) [3••].
Regarding the first group who oppose the practices of MAiD-NT (and MAiD, in general), it is claimed that religious and secular traditions uphold the sanctity of human life and that physicians are called to act in accordance with the non-maleficence principle (Primum non nocere), avoiding by all means to damage their patients (Hippocratic oath). This group argues that medicine has to preserve human life and uphold suicide prevention. Since there is an important difference between passively “allowing to die” and actively “killing,” MAiD-NT is not morally justifiable. In this sense, medicine is defined by its devotion to a clearly stated purpose: healing and the conservation of health and life. Therefore, in the doctor-patient relationship stands the moral duty to preserve “the most intimate, most personal, and most humane uses of technology—the helping, caring, and curing of vulnerable, anxious, dependent, and trusting members of the human community” [4] (page 24).
As a further argument, its is said that all people have obligations (e.g., to their family and society in general), until their death. These obligations limit their rights. While patients may refuse treatment, they do not have the right to be killed, since this, in the reciprocity of the doctor-patient relationship, would mean that physicians have a duty to kill [5].
Another issue is determining an objective prognosis in mental illnesses versus physical illnesses. For example, whether a disorder is irremediable in a somatic disease (e.g., advanced stage of cancer) is quite clear, it is not so clear in mental disorders, since irremediability is difficult to be predicted in MAiD-NT [6••]. With respect to this, Gaind [7•] poses a series of questions “[..] would society consider a (any number)% chance of irremediability from advancing metastatic cancer to be the same as a (same number)% chance of irremediability of suffering from a clinical depression associated with significant loneliness and poverty?”; or also “Given the absence of any guidance regarding predicting irremediability, does this mean that it would be discriminatory to not provide MAiD to patients for mental illness, or that it would be discriminatory to provide such patients MAiD by exposing them to death based on unscientific determinations of unpredictable irremediability for which there are no standards?” (pp. 604–606). In this sense with regard to the issue of irremediablity, MAiD-NT practices lack evidence-based data and without those data, as in all the branches of medicine, it is a risk to apply the practices whatever their aims are [8].
Also, risks have been raised regarding the “slippery slope” phenomenon, meaning that the extension of MAiD from terminal illness to other conditions, may facilitate losing control of the practice. For example, economic pressures are a reality in most health systems, with the risk that providing MAiD is far more cost-effective than medical care to chronically ill patients [9] Furthermore, some of the people requesting MAiD-NT are likely to be a source of usable organs for transplantation. Strengthening the link between MAiD and organ donation could damage the trust in medical, professional and public health authorities [10]. Therefore, MAiD-NT is extremely dangerous, especially when extended to minors and people with psychiatric disorders, as well as in those whose cognitive impairments (e.g. dementia) make it difficult to assess decisional capacity [11, 12]. The risk is that society could have the right to get rid of people with problems that require considerable resources, hypocritically masking it as a humanitarian act to be performed for the patient’s own good [13,14,15,16].
In an opposite position are those who consider MAiD-NT morally permissible, thus endorsing the extension of those practices to patients with psychiatric disorders. Proponents of this view argue that the single individual (neither the society nor the family) is the owner of his/her own life (including death, as part of life process). Thus, as an autonomous, rational, and self-aware individual, his/her decisions, including those about time and circumstances of death, should be respected (e.g., [17, 18]). On this basis, giving everybody the right to have a good death through MAiD-NT should be acceptable as a universal principle, since prolonging an unacceptable or unbearable life, marked by agony and loss of dignity, is immoral. On these premises, prohibiting MAiD-NT limits the rights of personal liberty and prevents intervention aimed at solving loss of independence, sense of purpose and meaning, and functional capacities. These argumentations suggest that we need to understand that life is not always the best outcome, and death is not always the worst, as death can be a better alternative than living in the presence of suffering (utilitarian perspective). Also, if an action, such as MAiD-NT, promotes the best interest of everyone concerned and violates no one’s rights, then that action is morally acceptable (libertarian perspective). In this way, the Hippocratic Oath’s directive that “I will take care that they (the sick) suffer no hurt or damage” should be interpreted as the duty for physicians to help a person to avoid prolonged suffering, including ending the person’s life, as a form of care.
A further argument supporting MAiD-NT is to dissolve the distinction between deaths caused by actions and death caused by omissions or inaction. If no morally significant difference can be found between deaths caused by omissions or by actions, then, by extension, there are grounds for allowing for death caused by actions. In this sense, Rachels [19] argues that letting a person die is a type of action, demonstrated by the fact that we would consider a doctor blameworthy if he needlessly let a person die.
It is however true that some who consider MAiD acceptable for people in a terminal somatic condition face a series of challenges in people with mental illness as follows: the ethical distinction between helping a dying person die peacefully versus providing death to a non-dying person; the unpredictability of prognosis of non-terminal conditions such as most mental illnesses; the difficulty that MAiD-NT may put vulnerable or marginalized people at risk of seeking death as a relief from poverty, loneliness, or other psychosocial stressors [10, 20,21,22,23,24]. For example, Trachsel and Jox [25••] examined the criteria for MAiD-NT in Switzerland and considered the criteria put forward by the Swiss Academy of Medical Sciences, namely, intolerable suffering due to severe illness or functional limitations (and acknowledged as such by a physician), are not sufficient. The authors, instead, underline that suffering is a necessary but not sufficient condition and that decision-making capacity and refractoriness of suffering should also be included as key criteria. Moreover, they contend that suffering, as a subjective experience, can only be quantified by the patient and not be objectively compared across individuals. This means that “intolerable suffering” is different across individuals and that it should encompass perceived burdensomeness i.e. the perception that one is a burden or drain on significant others or a burden on society.
On the other side, although it is clear that MAiD-NT requires careful safeguards to be permitted in people with refractory mental illness, to exclude all individuals requesting MAiD-NT falsely implies that everyone in that category lacks capacity. In fact, apart from those who are legally declared incompetent, few patients with psychiatric disorders lack capacity (e.g., 4% of patients with a personality disorder, 80% of patients with acute psychosis due to schizophrenia, 30% of patients with major depression) [26••].
Opinions and Attitudes About MAiD-NT for People with Psychiatric Disorders
Linked with the moral debate are the opinions that physicians (or health care professionals) and patients and their caregivers have about MAiD-NT (Supplement Table 2 for details).
Opinions and Attitudes of the General Population
Data are available from studies examining general population opinions about MAiD-NT, with significant differences between countries where the practices are legalized and those where the practices are prohibited.
For example, in the Netherlands, half of the respondents (53%) of the general population supported the eligibility of psychiatric patients for MAiD-NT, with only 15% stating their opposition to this practice [27]. In contrast, among the US general population, one-third supported legalizing MAiD-NT for people with physical disability (e.g., cerebral palsy) and dementia or mental illness (e.g., depression) [28]. This percentage significantly decreased, however, when a series of scenarios were presented showing the possible request by patients in non-terminal state because of loss of support from health care system or poverty [29].
Opinions and Attitudes of People with Psychiatric Disorders
Studies specifically examining psychiatric patients’ opinions on MAiD-NT are lacking. Having resistant or refractory psychiatric disorders can cause unbearable suffering—which has been defined as “a profoundly personal experience of an actual or perceived impending threat to the integrity of life of the person, which has a significant duration and a central place in the person’s mind” [30]. However, to fully understand what unbearable mental suffering is for patients with psychiatric disorders, directly questioning those who perceived it is mandatory. Analysis of requests for MAiD-NT by 26 Belgian psychiatric patients indicated five main categories of suffering: medically related, intrapersonal, interpersonal, societal-related, and existential suffering [31]. A Dutch study showed that the most frequent reasons for MAiD-NT were irreversibility, loss of control, emptiness and emotional flooding, freezing, social distancing, narcissistic wounds, confusion, and self-estrangement [32]. A further study showed that patients with psychiatric disorders reported autonomy and self-determination, ending the suffering, recognition as being persons, and dignified end-of-life as the main reasons to request MAiD-NT [33].
Opinions and Attitudes of Relatives of Patients with Psychiatric Disorders
While there is literature about MAiD examining caregivers and family relatives of patients with terminal somatic illness [34], there are only very few studies on families of patients with psychiatric disorders. A qualitative Dutch study showed that although the relatives of psychiatric patients were understanding of their wish to die (e.g., compassion, respect for autonomy, fear that the patient will commit a gruesome suicide), they also hoped that they would make another choice [35].
Regarding the outcome, people bereaved by MAiD (but not MAiD-NT) generally had similar or lower scores on measures of disordered grief, mental health, and posttraumatic stress compared with those who died naturally [36]. However, a Swiss study [37] showed that among members or close friends who were present at an assisted suicide, 13% met the criteria for full Post Traumatic Stress Disorder (PTSD), 6.5% for subthreshold PTSD, and 4.9% for complicated grief, indicating a higher prevalence of psychiatric disorders than the general population. However, specific data on family reactions after MAiD-NT for a patient with psychiatric conditions are not available.
Opinions and Attitudes of Physicians
Regarding the opinions of physicians on MAiD-NT, there are also great variations. In countries where the practice is legalized, physicians of different specialties generally endorse MAiD-NT, with differences according to the medical specialty (Supplement Table 2 for details). In the Netherlands, 20% of medical specialists endorsed the practice, about half among general practitioners (main reasons: responsibility, self-determination, compassion, fairness, and preventing suicide) [27, 38]. Early and advanced stages of dementia are considered less conceivable conditions than patients with terminal somatic diseases [39]. However, a large survey of more than 2,000 physicians showed that while the majority would grant a request for MAiD in somatically ill patients, only about one-third found MAiD-NT conceivable, and one-quarter endorsed it for people just tired of living [40].
Regarding mental health care professionals, including psychiatrists and psychiatric nurses, a specific point is that these individuals are usually trained to address suicidal ideation and behavior, by emphasizing hopes and purpose for living and by treating as much as possible the underlying disorders. Therefore, they are particularly aware of the dilemma caused by MAiD-NT. However, in the cited Dutch study [41, 42], about 2/3 of the psychiatrists believed it is possible to establish whether a psychiatric patient’s suffering is unbearable. The majority (74.5%) felt MAiD-NT should remain legal for adult psychiatric patients, who are experiencing unbearable mental suffering, who are able to make a well-considered request, and whose situation is hopeless. Half of them agree that MAiD-NT is compatible with a psychiatric care relationship [43] in which it is possible to establish whether the desire to die is entangled with a psychiatric disorder [41]. Dutch psychiatric nurses are also supportive of patients with different mental disorders to make an informed decision about MAiD-NT [44] and the majority feel themselves able to address and discuss the issue with their patients [45]. Similar data were reported in Switzerland [46].
In Canada, only one-third support MAiD-NT for mental illnesses [47, 48], with low endorsement related to the risk of changing the psychiatrists’ commitment to their patients; having a personal faith; and having had patients who would have received MAiD-NT for mental illness but who recovered. Cultural factors may also play a role, as shown in Israel, where psychiatrists displayed more conservative views on MAiD-NT for mental disorders than physicians from other medical specialties [49].
Attitudes Versus Active Role
Opinions about the practices of MAiD-NT do not necessarily correspond to playing a direct role. In fact, despite the support of Belgian psychiatrists for MAiD-NT, only a minority (8.4%) would actually engage in performing it with their own patients, and even less would perform MAiD-NT for a colleague’s patient (4.5%) [43]. Furthermore, although about 80% psychiatrists in Belgium had to deal with at least one MAiD-NT request, only 5% were actually involved in the administration of lethal drugs or attended when another physician was performing the act for their own patient [50].
The first point here is to determine if the criteria for MAiD-NT for patients with psychiatric disorders are equivalent to patients with somatic terminal conditions, given that suicide ideation can be a symptom of mental disorders. This point speaks to the 2-track approach of the Dutch law, where mental health care professionals have to evaluate the possible MAiD request from their patients to grant the request itself, while at the same time, maintaining a recovery-oriented care and being committed to suicide prevention [51, 52].
A second point is the difference between irrational and rational suicidality, with one position suggesting that suicide is always an irrational act and the other supporting the view that patients who suffer from a severe mental disorder but maintain competence, such as severe depressive disorders or schizophrenia, can indeed have a rational wish to die [53,54,55, 56••, 57].
There are other motives regarding healthcare professional involvement or non-involvement in MAiD-NT, such as lack of criteria or difficulties in applying these criteria [50, 58] or the problem of suicide in those who had their request refused [59].
Studies on MAiD-NT Cases Among People with Psychiatric Disorders
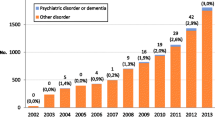
Analysis of the literature of the last years shows a constant increase of MAiD-NT cases and requests in the context of patients with psychiatric disorders (Supplement Table 3).
In Belgium, MAiD-NT due to psychiatric disorder have increased from 0.5% of all cases reported in the period 2002–2007 to 3.0% of all cases reported in 2011, [60] with a total number of psychiatric patients explicitly requesting it between 1,100 and 1,150 (2015–2016) and 60–70 patients effectively receiving it. The requests due to psychiatric disorders, mainly depression and personality disorders, in young patients, became the sixth most common indication. In most cases, patients were less than 70 years old (mean age 47 years) [61] and about half of patients had made suicide attempts before [62, 63], including while waiting for approval [61].
In the Netherlands, the number of MAiD-NT cases increased from 2011 (n = 2) to 2017 (n = 83) [64], for patients with mood or personality disorders, mainly women and aged between 50 and 70 years [62, 65].
In Canada, where the Supreme Court extended MAiD to other conditions beyond terminal illnesses (to “a person whose natural death is not reasonably foreseeable”) [66], mental illnesses are temporarily excluded from eligibility up until March 2023. In the meantime, the Minister of Justice and Health will provide guidelines for MAiD-NT. A series of cases of patients with psychiatric disorders who applied for MAiD-NT were denied it, although, based on their characteristics, would have been eligible for MAiD-NT in other countries (e.g. Belgium, Netherlands) [67, 68]. The number of patients with borderline personality disorders requesting MAiD-NT is also markedly increasing [69••].
The Impact of MAiD-NT in Mental Health Professionals
There is a dearth of research on how MAiD in general may impact physician health and well-being, but even less is known about MAiD-NT. The uncertainty of predicting irremediability, possible conflation of psychiatric suffering with illness suffering, and the challenges of differentiating patients seeking MAiD-NT from the suicidal patients will all likely impact health care professionals [70]. For example, there are data showing that advance request for MAiD-NT in cases of patients with dementia was complicated by ambiguous directives, patients being unaware of the procedure, and physicians’ difficulty in assessing “unbearable suffering.” [71]
For some disorders, such as borderline personality disorders, a physician intervening by MAiD-NT could encounter moral distress, since the criteria for the procedure might not take into consideration the common fluctuating suicidal ideation and behavior in these disorders, the contemporary forms of psychosocial rehabilitation treatment, and the individual’s potential for having a life worth living [68, 72].
Conclusion
The increasing number of countries endorsing and legalizing MAiD-NT for people with psychiatric disorders underscores the need to examine this phenomenon in more detail and from many different perspectives.
The first moral issue we have summarized indicates that criteria for MAiD-NT in people with intolerable suffering caused by non-terminal disease, such patients with psychiatric disorders (but also with neurological disorders refractory to any treatment, dementia, or even minors or people with existential suffering), are more problematic than the criteria for patients with somatic incurable diseases in an advanced or terminal phase. This is a moral dilemma that can cause significant conflict: on the one hand, it can be argued that professional roles, responsibilities, and personal expectations include the duty to preserve life, and that failure to do so by way of not having foreseen and prevented suicide can result in moral and legal culpability. On the other hand, there is the professional obligation to help and not abandon patients and the duty to relieve suffering, by helping them to die. There also needs to be a better definition and ways to assess unbearable suffering that patients’ experiencing psychiatric disorders, and further exploration of how this can be addressed in the therapeutic setting [73].
A second moral issue regards the “rationality” of a request to be helped in dying. Although physicians differentiate three types of death wishes among patients with psychiatric disorders (death wish related to psychopathology or impulsive suicidality; death wish consistent over time, or chronic suicidality, and rational death wishes) [74], more research should be carried out in this area.
A third issue we have addressed is the impact of MAiD-NT in physicians. In spite of the importance of this topic, it has been largely neglected with only a few studies examining the impact of MAiD on healthcare professionals in palliative care setting. Thirty to fifty percent of physicians expressed emotional burden or discomfort regarding participation, and adverse personal impact in 15–20% [75•]. The risk for health care professional to suffer and become psychologically vulnerable because of emotional exhaustion, detachment toward patients, poor professional accomplishment, moral distress, or even depression and risk of suicide should be considered when examining the implications of MAiD-NT [76].
In summary, although the literature has shown that a small percentage of people with psychiatric disorders died by MAiD-NT in comparison with patients with somatic terminal diseases, the problems it elicits are not solved yet. How to make objective criterion of irremediability of a mental disorder; how to balance suicide prevention with assisted suicide; how to avoid the risk of progressively including in MAiD-NT requests by vulnerable segments of the population, such as minors and elderly or people with dementia, in a productive-oriented society, are some of the critical points to be considered. As indicated from the beginning in the Dutch experience [77, 78], the application of MAiD-NT in people with mental disorders should be further explored, to prevent end-of-life rights from contradicting the principles of recovery-oriented care in psychiatry.
Change history
28 August 2022
Missing Open Access funding information has been added in the Funding Note.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Groenewoud JH, van der Maas PJ, van der Wal G, Hengeveld MW, Tholen AJ, Schudel WJ. van der Heide A Physician-assisted death in psychiatric practice in the Netherlands. N Engl J Med. 1997;336(25):1795–801. https://doi.org/10.1056/NEJM199706193362506.
• Sheehan K, Gaind KS, Downar J. Medical assistance in dying: special issues for patients with mental illness. Curr Opin Psychiatry, 2017;30(1):26–30. https://doi.org/10.1097/YCO.0000000000000298. This is a review underlying the scarce role of psychiatrist in MAiD for terminally patients, and their specific role in MAiD-NT.
•• Nicolini ME, Nicolini ME, Kim SYH, Churchill ME, Gastmans C. Should euthanasia and assisted suicide for psychiatric disorders be permitted? A systematic review of reasons Psychol Med. 2020;50:1241–1256. https://doi.org/10.1017/S0033291720001543. Review on the reasons for and against E/PAS in psychiatric patients. Debate on parity between mental and physical illnesses, concept of irremediability and the issue of suicide prevention in psychiatric disorders in relation to E/PAS.
Pellegrino ED. Medical ethics in an era of bioethics: resetting the medical profession’s compass. Theor Med Bioeth. 2012;33:21–4. https://doi.org/10.1007/s11017-012-9209-1.
Pellegrino ED. Patient and physician autonomy: conflicting rights and obligations in the physician-patient relationship. J Contemp Health Law Policy. 1994;10:47–68.
•• Van Veen SMP, Ruissen AM, Widdershoven GAM. Irremediable psychiatric suffering in the context of physician-assisted death: a scoping review of arguments Can J Psychiatry. 2020;65(9):593–603. https://doi.org/10.1177/0706743720923072. Ethical and clinical paper regarding the concept of irremediability in psychiatric disorders, with arguments concerning uncertainty of diagnosis and prognosis in these disorders, the nature of mental illness and relative treatments, as well as arguments concerning hope and treatment refusal.
• Gaind KS. What does “irremediability” in mental illness mean? Can J Psychiatry. 2020;65(9):604–6. https://doi.org/10.1177/0706743720928656. Critical discussion and arguments about the meaning of irremediability of psychiatric disorders.
Sinyor M, Schaffer A. The lack of adequate scientific evidence regarding physician-assisted death for people with psychiatric disorders is a danger to patients. Can J Psychiatry. 2020;65(9):607–9. https://doi.org/10.1177/0706743720928658.
Trachtenberg AJ, Manns B. Cost analysis of medical assistance in dying in Canada. CMAJ. 2017;189(3):E101–5. https://doi.org/10.1503/cmaj.160650.
Buturovic Z. Embracing slippery slope on physician-assisted suicide and euthanasia could have significant unintended consequences. J Med Ethics. 2020;medethics-2020–106089. https://doi.org/10.1136/medethics-2020-106089.
Kim SY, Mangino D, Nicolini M. Is this person with dementia (currently) competent to request euthanasia? A complicated and underexplored question. J Med Ethics. 2020;medethics-2020–106091. https://doi.org/10.1136/medethics-2020-106091.
Mondragón JD, Salame L, Kraus A, De Deyn PP. Clinical considerations in physician-assisted death for probable Alzheimer’s disease: decision-making capacity, anosognosia, and suffering. Dement Geriatr Cogn Dis Extra. 2019;9:217–26. https://doi.org/10.1159/00050018.
Cuman G, Gastmans C. Minors and euthanasia: a systematic review of argument-based ethics literature. Eur J Pediatr. 2017;176(7):837–47. https://doi.org/10.1007/s00431-017-2934-8.
Trejo-Gabriel-Galán JM. Euthanasia and assisted suicide in neurological diseases: a systematic review Neurologia (Engl Ed). 2021;S0213–4853(21)00090–6. https://doi.org/10.1016/j.nrl.2021.04.016.
Rajkumar RP. Physician-assisted suicide in dementia: paradoxes, pitfalls and the need for prudence Front Sociol. 2021;6:815233. https://doi.org/10.3389/fsoc.2021.815233.
Simpson AIF. Medical assistance in dying and mental health: a legal, ethical, and clinical analysis. Can J Psychiatry. 2018;63(2):80–84. https://doi.org/10.1177/0706743717746662.
Kamm F. A Right to Choose Death. Boston Rev. 1997;20–23. Last Accessed 07 June 2022. https://bostonreview.net/articles/fm-kamm-right-choose-death/.
Singer P. Practical Ethics. 3rd ed. Cambridge: Cambridge University Press; 2011.
Rachels J. Active and Passive Euthanasia in Singer P. Applied Ethics: Oxford, Oxford University Press; 1986. 32–4.
Mehlum L, Schmahl C, Berens A, Doering S, Hutsebaut J, Kaera A, Kramer U, Moran PA, Renneberg B, Ribaudi JS, Simonsen S, Swales M, Taubner S, di Giacomo E. Euthanasia and assisted suicide in patients with personality disorders: a review of current practice and challenges Borderline Personal Disord Emot Dysregul. 2020;7:15. https://doi.org/10.1186/s40479-020-00131-9.
Mangino DR, Bernhard T, Wakim P, Kim SY. Assessing public’s attitudes towards euthanasia and assisted suicide of persons with dementia based on their advance request: an experimental survey of US public. Am J Geriatr Psychiatry. 2020;S1064–7481(20):30431. https://doi.org/10.1016/j.jagp.2020.07.013.
Evenblij K, Pasman HRW, van der Heide A, van Delden JJM, Onwuteaka-Philipsen BD. Public and physicians; support for euthanasia in people suffering from psychiatric disorders: a cross-sectional survey study BMC Med Ethics. 2019;20(1):62. https://doi.org/10.1186/s12910-019-0404-8.
Van Den Noortgate N, Van Humbeeck L. Medical assistance in dying and older persons in Belgium: trends, emerging issues and challenges. Age Ageing. 2021 Jan 8;50(1):68-71. https://doi.org/10.1093/ageing/afaa116.
Council of Canadian Academies. The state of knowledge on medical assistance in dying where a mental disorder is the sole underlying medical condition. Ottawa (ON):The Expert Panel Working Group on MAID Where a Mental Disorder Is the Sole Underlying Medical Condition. 2018. https://cca-reports.ca/wp-content/uploads/2018/12/The-State-of-Knowledge-on-Medical-Assistance-in-Dying-Where-a-Mental-Disorder-is-the-Sole-Underlying-Medical-Condition.pdf.
•• Trachsel M, Jox RJ. Suffering is not enough: assisted dying for people with mental illness Bioethics. 2022. https://doi.org/10.1111/bioe.1300. This is a paper examining the criteria to be met for permitting MAiD, indicating that suffering is a necessary but insufficient condition for assisted dying, and that the criteria should also include decision-making capacity and refractoriness of suffering.
•• Dembo J, Schuklenk U, Reggler J. “For their own good”: a response to popular arguments against permitting medical assistance in dying (MAID) where mental illness is the sole underlying condition. Can J Psychiatry. 2018;63(7):451–456. https://doi.org/10.1177/0706743718766055. The paper examines several factors, such as prejudices, stigma, and paternalism persist in psychiatry. It is unjustifiable to exclude psychiatric patients from benefitting from a medical intervention that is designed to preserve autonomy and reduce suffering, without giving due consideration to individual variability, just because of the benevolent intent of making decisions in their best interests.
Evenblij K, Pasman HRW, Van Der Heide A, Van Delden JJM, Onwuteaka-Philipsen BD. Public and physicians’ support for euthanasia in people suffering from psychiatric disorders: a cross-sectional survey study. BMC Med Ethics. 2019b;20:1–10. https://doi.org/10.1186/s12910-019-0404-8.
Mangino DR, Bernhard T, Wakim P, Kim SY. Assessing public’s attitudes towards euthanasia and assisted suicide of persons with dementia based on their advance request: an experimental survey of US public. Am J Geriatr Psychiatry. 2021;29(4):384–94. https://doi.org/10.1016/j.jagp.2020.07.013.
Berens N, Wasserman D, Wakim P, Bernhard T, Kim SYH. Resource limitation and “forced irremediability” in physician-assisted deaths for nonterminal mental and physical conditions: a survey of the US public. J Acad Consult Liaison Psychiatry. 2022;S2667–2960(21):00204–14. https://doi.org/10.1016/j.jaclp.2021.12.010.
Dees M, Vernooij-Dassen M, Dekkers W, van Weel C. Unbearable suffering of patients with a request for euthanasia or physician-assisted suicide: an integrative review. Psychooncology. 2010;19. https://doi.org/10.1002/pon.1612.
Verhofstadt M, Thienpont L, Peters GJY. When unbearable suffering incites psychiatric patients to request euthanasia: qualitative study. Br J Psychiatry. 2017;211. https://doi.org/10.1192/bjp.bp.117.199331.
Lengvenyte A, Strumila R, Courtet P, Kim SYH, Olié E. “Nothing hurts less than being dead”: psychological pain in case descriptions of psychiatric euthanasia and assisted suicide from the Netherlands. Can J Psychiatry. 2020;65:612–620. https://doi.org/10.1177/0706743720931237.
Pronk R, Willems DL, van de Vathorst S. Feeling seen, being heard: perspectives of patients suffering from mental illness on the possibility of physician-assisted death in the Netherlands. Cult Med Psychiatry. 2022;46(2):475-489. https://doi.org/10.1007/s11013-021-09726-5.
Roest B., Trappenburg M, Leget C. The involvement of family in the Dutch practice of euthanasia and physician assisted suicide: a systematic mixed studies review. BMC Med Ethics. 2019 Apr 5;20(1):23. https://doi.org/10.1186/s12910-019-0361-2.
Pronk R, Willems DL, van de Vathorst S. What about us? Experiences of relatives regarding physician-assisted death for patients suffering from mental illness: a qualitative study. Cult Med Psychiatry. 2021 Dec 16;1–15. https://doi.org/10.1007/s11013-021-09762.
Andriessen K, Krysinska K, Castelli Dransart DA, Dargis L, Mishara BL. Grief after euthanasia and physician-assisted suicide. Crisis. 2020;41(4):255–72. https://doi.org/10.1027/0227-5910/a000630.
Wagner B, Müller J, Maercker A. Death by request in Switzerland: posttraumatic stress disorder and complicated grief after witnessing assisted suicide. Eur Psychiatry. 2012;27(7):542–6. https://doi.org/10.1016/j.eurpsy.2010.12.003.
Pronk R, Sindram NP, van de Vathorst S, Willems DL. Experiences and views of Dutch general practitioners regarding physician-assisted death for patients suffering from severe mental illness: a mixed methods approach. Scand J Prim Health Care. 2021;39(2):166–73. https://doi.org/10.1080/02813432.2021.1913895.
Bolt EE, Snijdewind MC, Willems DL, van der Heide A, Onwuteaka-Philipsen BD. Can physicians conceive of performing euthanasia in case of psychiatric disease, dementia or being tired of living? J Med Ethics. 2015;41:592–8. https://doi.org/10.1136/medethics-2014-102150.
Bolt EE, Snijdewind MC, Willems DL, van der Heide A, Onwuteaka-Philipsen BD. Can physicians conceive of performing euthanasia in case of psychiatric disease, dementia or being tired of living? J Med Ethics. 2015;41(8):592–8. https://doi.org/10.1136/medethics-2014-102150.
Evenblij K, Pasman HRW, Van Der Heide A, Van Delden JJM, Onwuteaka-Philipsen BD. Public and physicians’ support for euthanasia in people suffering from psychiatric disorders: a cross-sectional survey study. BMC Med Ethics. 2019b;20:1–10. https://doi.org/10.1186/s12910-019-0404-8.
Evenblij K, Pasman HRW, Pronk R, Onwuteaka-Philipsen BD. Euthanasia and physician-assisted suicide in patients suffering from psychiatric disorders: a cross-sectional study exploring the experiences of Dutch psychiatrists. BMC Psychiatry. 2019a;19:1–10. https://doi.org/10.1186/s12888-019-2053-3.
Verhofstadt M, Audenaert K, Van Den Broeck K, Deliens L, Mortier F, Titeca K, Pardon K, Chambaere K. Belgian psychiatrists’ attitudes towards, and readiness to engage in, euthanasia assessment procedures with adults with psychiatric conditions: a survey. BMC Psychiatry. 2020;20:1–10. https://doi.org/10.1186/s12888-020-02775-x.
Demedts D, Roelands M, Libbrecht J, Bilsen J. The attitudes, role & knowledge of mental health nurses towards euthanasia because of unbearable mental suffering in Belgium: a pilot study. J Psychiatr Ment Health Nurs. 2018. https://doi.org/10.1111/jpm.12475.
De Hert M, Van Bos L, Sweers K, Wampers M, De Lepeleire J, Correll CU. Attitudes of psychiatric nurses about the request for euthanasia on the basis of unbearable mental suffering(UMS). PLoS One. 2015;10:1–13. https://doi.org/10.1371/journal.pone.0144749.
Hodel MA, Hoff P, Irwin SA, Biller-Andorno N, Riese F, Trachsel M. Attitudes toward assisted suicide requests in the context of severe and persistent mental illness: a survey of psychiatrists in Switzerland Palliat Support Care. 2019;17(6):621–7. https://doi.org/10.1017/S1478951519000233.
Canadian Psychiatric Association. Task force on medical assistance in dying: 2016 member survey results. Ottawa (ON): Canadian Psychiatric Assoc. 2017. https://www.cpa-apc.org/wp-content/uploads/CPA-MAIDTF-16Surv-Rep-FIN-EN.pdf.
Rousseau S, Turner S, Chochinov HM, Enns MW, Sareen J. A national survey of Canadian psychiatrists’ attitudes toward medical assistance in death. Can J Psychiatry. 2017;62(11):787–94. https://doi.org/10.1177/0706743717711174.
Levy TB, Azar S, Huberfeld R, Siegel AM, Strous RD. Attitudes towards euthanasia and assisted suicide: a comparison between psychiatrists and other physicians. Bioethics. 2013;27:402–8. https://doi.org/10.1111/j.1467-8519.2012.01968.x.
Verhofstadt M, Audenaert K, Van Den Broeck K, Deliens L, Mortier F, Titeca K, Pardon K, De Bacquer D, Chambaere K. The engagement of psychiatrists in the assessment of euthanasia requests from psychiatric patients in Belgium: a survey study. BMC Psychiatry. 2020;20:1–11. https://doi.org/10.1186/s12888-020-02792-w.
Pronk R, Evenblij K, Willems DL, van de Vathorst S. Considerations by Dutch psychiatrists regarding euthanasia and physician-assisted suicide in psychiatry: a qualitative study. J Clin Psychiatry. 2019;80. https://doi.org/10.4088/JCP.19m12736.
Miller FG, Appelbaum PS. Physician-assisted death for psychiatric patients - misguided public policy. N Engl J Med. 2018;378(10):883–5. https://doi.org/10.1056/NEJMp1709024.
Wittwer H. The problem of the possible rationality of suicide and the ethics of physician-assisted suicide. Int J Law Psychiatry. 2013;36(5–6):419–26. https://doi.org/10.1016/j.ijlp.2013.06.009.
Hewitt J. Why are people with mental illness excluded from the rational suicide debate? Int J Law Psychiatry. 2013;36(5–6):358–65. https://doi.org/10.1016/j.ijlp.2013.06.006.
Hewitt J. Rational suicide: philosophical perspectives on schizophrenia. Med Health Care Philos. 2010;13(1):25–31. https://doi.org/10.1007/s11019-009-9183-1.
•• Grigoriou M, Upthegrove R, Bortolotti L. Instrumental rationality and suicide in schizophrenia: a case for rational suicide?. Med Ethics. 2019;45(12):802–805. https://doi.org/10.1136/medethics-2019-105454. The paper examines how not delusional beliefs or perception disorders, but other under-examined, perhaps rational reasons, such as extreme social isolation, severe depression, or emotional withdrawal, may cause rational suicidal ideation in patients with schizophrenia.
Evenblij K, Pasman HRW, Pronk R, Onwuteaka-Philipsen BD. Euthanasia and physician-assisted suicide in patients suffering from psychiatric disorders: a cross-sectional study exploring the experiences of Dutch psychiatrists. BMC Psychiatry. 2019;19:1–10. https://doi.org/10.1186/s12888-019-2053-3.
Evenblij K, Pasman HRW, Pronk R, Onwuteaka-Philipsen BD. Euthanasia and physician-assisted suicide in patients suffering from psychiatric disorders: a cross-sectional study exploring the experiences of Dutch psychiatrists. BMC Psychiatry 2019a;19:1–10. https://doi.org/10.1186/s12888-019-2053-3.
Evenblij K, Pasman HRW, Pronk R, Onwuteaka-Philipsen BD. Euthanasia and physician-assisted suicide in patients suffering from psychiatric disorders: a cross-sectional study exploring the experiences of Dutch psychiatrists. BMC Psychiatry. 2019a;19:1–10. https://doi.org/10.1186/s12888-019-2053-3.
Dierickx S, Deliens L, Cohen J, Chambaere K. Euthanasia for people with psychiatric disordersor dementia in Belgium : analysis of officially reported cases. 2017;1–9. https://doi.org/10.1186/s12888-017-1369-0.
Thienpont L. Euthanasia requests, procedures and outcomes for 100 Belgian patients suffering from psychiatric disorders: a retrospective , descriptive study. 2015. https://doi.org/10.1136/bmjopen-2014-007454.
Kim SYH, Vries RD, Peteet JR. Euthanasia and assisted suicide of patients with psychiatric disorders in the Netherlands 2011–2014 H. HHS Public Access. 2017;73:362–8. https://doi.org/10.1001/jamapsychiatry.2015.2887.
Kim SYH, Conwell Y, Caine ED. Suicide and physician-assisted death for persons with psychiatric disorders: how much overlap? JAMA Psychiatry. 2018;75(11):1099–1100. https://doi.org/10.1001/jamapsychiatry.2018.2065.
Dom G, Stoop H, Haek A, Sigrid S. Euthanasia and assisted suicide in the context of psychiatric disorders : sharing experiences from the Low Countries. 2020;54:661–672. https://doi.org/10.12740/PP/124078.
Kim SYH, Conwell Y, Caine ED. Suicide and physician-assisted death for persons with psychiatric disorders: how much overlap? JAMA Psychiatry. 2018;75(11):1099–1100.https://doi.org/10.1001/jamapsychiatry.2018.2065.
Bill C-7. An Act to amend the Criminal Code (medical assistance in dying), 17th March, 2021. Last Accessed 07 June 2022. https://lop.parl.ca/sites/PublicWebsite/default/en_CA/ResearchPublications/LegislativeSummaries/432C7E
Perreault A, Benrimoh D, Fielding A. Euthanasia requests in a Canadian psychiatric outpatient clinic: a case series part 2 of the McGill University euthanasia in psychiatry case series . Int J Law Psychiatry. 2019;66:101464. https://doi.org/10.1016/j.ijlp.2019.101464.
Benrimoh D, Perreault A, Van Den Eynde F. Euthanasia requests in a Canadian psychiatric emergency room: a case series: Part 1 of the McGill University euthanasia in psychiatry case series. Int J Law Psychiatry. 2017;55:37–44. https://doi.org/10.1016/j.ijlp.2017.10.006.
•• Mehlum L, Schmahl C, Berens A, et al. Euthanasia and assisted suicide in patients with personality disorders: a review of current practice and challenges. Borderline Personal Disord Emot Dysregul. 2020;7(1):15. https://doi.org/10.1186/s40479-020-00131-9. This paper analyzes the problem of MAiD-NT in patients with personality disorder suggesting that the current legislation is based on an inadequate understanding of underlying psychopathology and a lack of awareness about the contemporary treatment literature of these disorders. Also, the authors assert that MAiD-NT neglects the individual’s potential for having a life worth living.
Gaind KS, Crawford A, Geist R, Henick M, Kim SYH, Lemmens T, Mishara B, Simpson S, Shakespeare T, Stainton T, et al. Expert advisory group on MAiD. Canada at a crossroads: recommendations on medical assistance in dying and persons with a mental disorder—an evidence-based critique of the Halifax group IRPP Report. Toronto (ON): EAG. 2020. https://doi.org/10.13140/RG.2.2.36236.87687.
Mangino DR, Nicolini ME, De Vries RG, Kim SYH. Euthanasia and assisted suicide of persons with dementia in the Netherlands. Am J Geriatr Psychiatry. 2020;28(4):466–77. https://doi.org/10.1016/j.jagp.2019.08.015.
Gaind KS. What does “irremediability” in mental illness mean? Can J Psych. 2020;65(9):604–6. https://doi.org/10.1177/0706743720928656. Epub 2020 May 22.
Thienpont L, Verhofstadt M, Van Loon T, Distelmans W, Audenaert K, De Deyn PP. Euthanasia requests, procedures and outcomes for 100 Belgian patients suffering from psychiatric disorders: a retrospective, descriptive study. BMJ Open. 2015. https://doi.org/10.1136/bmjopen-2014-007454.
Pronk R, Willems DL, van de Vathorst S. Do doctors differentiate between suicide and physician-assisted death? A qualitative study into the views of psychiatrists and general practitioners. Cult Med Psychiatry. 2021;45(2):268–81.
• Kelly B, Handley T, Kissane D, Vamos M, Attia J. “An indelible mark” the response to participation in euthanasia and physician-assisted suicide among doctors: a review of research findings. Palliat Support Care. 2020;18(1):82–8. This is a review of the emotional impact of MAiD on participating clinicians, showing the negative consequences in terms of professional roles, responsibilities, and personal expectations.
Grassi L, Gaind KS, Nash T, Caruso R. Euthanasia and medical assistance in dying as challenges for physicians’ well-being. In Luigi Grassi, Daniel McFarland, Michelle B. Riba (Eds), Depression, Burnout and Suicide in Physicians, Springer, Berlin, pp, 113–125, 2021.
Kerkhof JF. Assisted suicide among psychiatric patients in The Netherlands. Crisis. 1994;15(2):50–2.
Schoevers RA, Asmus FP, Van Tilburg W. Physician-assisted suicide in psychiatry: developments in The Netherlands. Psychiatr Serv. 1998;49(11):1475–80. https://doi.org/10.1176/ps.49.11.1475.
Acknowledgements
The editors would like to thank Dr. Harvey Max Chochinov for taking the time to review this manuscript.
Funding
Funding Open access funding provided by Università degli Studi di Ferrara within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Federica Folesani, Marco Marella, Elisa Tiberto, Michelle B. Riba, Lisa Bortolotti, Tommaso Toffanin, Laura Palagini, Martino Belvederi Murri, Bruno Biancosino, Maria Ferrara, and Rosangela Caruso declare that they have no conflict of interest. Luigi Grassi has received royalties for books from Springer, and personal fees from EISAI and ANGELINI for scientific consultancy outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Complex Medical-Psychiatric Issues
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grassi, L., Folesani, F., Marella, M. et al. Debating Euthanasia and Physician-Assisted Death in People with Psychiatric Disorders. Curr Psychiatry Rep 24, 325–335 (2022). https://doi.org/10.1007/s11920-022-01339-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11920-022-01339-y