Abstract
Purpose of Review
While clinicians have been using antidepressants for off-label indications in the treatment of chronic pain in recent years, newer studies have proven effectiveness and provided additional mechanistic understanding and defined potential adverse effects. As depression and chronic pain are frequently comorbid conditions, the use of antidepressants has allowed for treatment of both conditions concomitantly in the same patient population.
Recent Findings
The most commonly used antidepressants for chronic pain are tricyclic antidepressants (TCAs), though selective serotonin or noradrenaline reuptake inhibitors and other atypical antidepressants have been shown to be effective at treating chronic pain. In addition to neuropathic pain, bupropion has also demonstrated effectiveness in treating chronic pain caused by inflammatory bowel disease. Selective norepinephrine receptor inhibitors (SNRIs), including duloxetine, serve to suppress neuropathic pain by altering recovery of the noradrenergic descending inhibitory system in the spinal cord. While the direct mechanism of action is largely unknown, TCAs may suppress the noradrenergic descending inhibitory system to produce an antihyperalgesic effect.
Summary
The use of antidepressants offers alternative and adjunctive therapy options for patients suffering from chronic pain from various modalities. TCAs, mono-amine oxidase inhibitors, selective serotonin receptor inhibitors, SNRIs, and atypical antidepressants have been shown to have analgesic and sometimes antiinflammatory capabilities that are independent of their mood-stabilizing effects. Further studies are warranted to establish better safety profiles and efficacy of antidepressant use in chronic pain.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Jackson KC, St. Onge EL. Antidepressant pharmacotherapy: considerations for the pain clinician. Pain Pract. 2003;3:135–43.
Murnion BP. Neuropathic pain: current definition and review of drug treatment. Aust Prescr NPS Med Wise. 2018;41:60–3.
Mika J, Zychowska M, Makuch W, Rojewska E, Przewlocka B. Neuronal and immunological basis of action of antidepressants in chronic pain – clinical and experimental studies. Pharmacol Reports. 2013;65(6):1611–21.
Morris DW, Trivedi MH, Fava M, Wisniewski SR, Balasubramani GK, Khan AY, et al. Diurnal mood variation in outpatients with major depressive disorder. Depress Anxiety. 2009;26:851–63.
Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs. placebo in patients with painful diabetic neuropathy. Pain. 2005;116:109–18.
Hirschfeld RMA, Mallinckrodt C, Lee TC, Detke MJ. Time course of depression-symptom improvement during treatment with duloxetine. Depress Anxiety. 2005;21:170–7.
Mico J, Ardid D, Berrocoso E, Eschalier A. Antidepressants and pain. Trends Pharmacol Sci. 2006;27:348–54.
•• Riediger C, Schuster T, Barlinn K, Maier S, Weitz J, Siepmann T. Adverse effects of antidepressants for chronic pain: a systematic review and meta-analysis. Front Neurol. 2017;8:307. A systematic review of adverse effects of antidepressants.
Fava M, Rush AJ, Thase ME, Clayton A, Stahl SM, Pradko JF, Johnston JA. 15 years of clinical experience with bupropion HCl: from bupropion to bupropion SR to bupropion XL. Prim Care Companion J Clin Psychiatry. 2005;7(3):106–13.
Mikocka-Walus AA, Turnbull DA, Moulding NT, Wilson IG, Andrews JM, Holtmann GJ. Antidepressants and inflammatory bowel disease: a systematic review. Clin Pract Epidemiol Ment Health Bentham Science Publishers. 2006;2:24.
Arias HR. Is the inhibition of nicotinic acetylcholine receptors by bupropion involved in its clinical actions? Int J Biochem Cell Biol. 2009;41:2098–108.
Dhillon S, Yang LPH, Curran MP. Bupropion: a review of its use in the management of major depressive disorder. Drugs. 2008;68:653–89.
Montgomery SA. Antidepressants and seizures: emphasis on newer agents and clinical implications. Int J Clin Pract. 2005;59:1435–40.
Semenchuk MR, Sherman S, Davis B. Double-blind, randomized trial of bupropion SR for the treatment of neuropathic pain. Neurology. 2001;57:1583–8.
Bielefeldt K, Davis B, Binion DG. Pain and inflammatory bowel disease. Inflamm Bowel Dis NIH Public Access. 2009;15:778–88.
Sadeghi H, Hajhashemi V, Minaiyan M, Movahedian A, Talebi A. Further studies on anti-inflammatory activity of maprotiline in carrageenan-induced paw edema in rat. Int Immunopharmacol. 2013;15:505–10.
Kast RE, Altschuler EL. Remission of Crohn’s disease on bupropion. Gastroenterology. 2001;121:1260–1.
Brustolim D, Ribeiro-dos-Santos R, Kast RE, Altschuler EL, Soares MBP. A new chapter opens in anti-inflammatory treatments: the antidepressant bupropion lowers production of tumor necrosis factor-alpha and interferon-gamma in mice. Int Immunopharmacol. 2006;6:903–7.
Hajhashemi V, Khanjani P. Analgesic and anti-inflammatory activities of bupropion in animal models. Res Pharm Sci Wolters Kluwer -- Medknow Publications. 2014;9:251–7.
Spina E, Trifirò G, Caraci F. Clinically significant drug interactions with newer antidepressants. CNS Drugs. Springer International Publishing. 2012;26:39–67.
Debonnel G, Saint-André E, Hébert C, de Montigny C, Lavoie N, Blier P. Differential physiological effects of a low dose and high doses of venlafaxine in major depression. Int J Neuropsychopharmacol. 2007;10:51–61.
• Ito S, Suto T, Saito S, Obata H. Repeated administration of duloxetine suppresses neuropathic pain by accumulating effects of noradrenaline in the spinal cord. Anesth Analg. 2018;126:298–307. A mechanism of action by which duloxetine serves to reduce neuropathic pain.
Fava GA, Benasi G, Lucente M, Offidani E, Cosci F, Guidi J. Withdrawal symptoms after serotonin-noradrenaline reuptake inhibitor discontinuation: systematic review. Psychother Psychosom Karger Publishers. 2018;87:195–203.
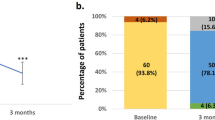
Uchio Y, Enomoto H, Ishida M, Tsuji T, Ochiai T, Konno S. Safety and efficacy of duloxetine in Japanese patients with chronic knee pain due to osteoarthritis: an open-label, long-term, phase III extension study. J Pain Res. 2018;11:1391–403.
Sofat N, Harrison A, Russell MD, Ayis S, Kiely PD, Baker EH, et al. The effect of pregabalin or duloxetine on arthritis pain: a clinical and mechanistic study in people with hand osteoarthritis. J Pain Res Dove Press. 2017;10:2437–49.
Iqbal Z, Azmi S, Yadav R, Ferdousi M, Kumar M, Cuthbertson DJ, et al. Diabetic peripheral neuropathy: epidemiology, diagnosis, and pharmacotherapy. Clin Ther. 2018;40:828–49.
Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy or chronic pain. In: Lunn MP, editor. Cochrane database Syst Rev. Chichester: John Wiley & Sons, Ltd; 2009. p. CD007115.
Avan R, Janbabaei G, Hendouei N, Alipour A, Borhani S, Tabrizi N, et al. The effect of pregabalin and duloxetine treatment on quality of life of breast cancer patients with taxane-induced sensory neuropathy: a randomized clinical trial. J Res Med Sci Wolters Kluwer -- Medknow Publications. 2018;23:52.
Farshchian N, Alavi A, Heydarheydari S, Moradian N. Comparative study of the effects of venlafaxine and duloxetine on chemotherapy-induced peripheral neuropathy. Cancer Chemother Pharmacol. Springer Berlin Heidelberg. 2018;82:787–93.
Matsuoka H, Ishiki H, Iwase S, Koyama A, Kawaguchi T, Kizawa Y, et al. Study protocol for a multi-institutional, randomised, double-blinded, placebo-controlled phase III trial investigating additive efficacy of duloxetine for neuropathic cancer pain refractory to opioids and gabapentinoids: the DIRECT study. BMJ Open British Medical Journal Publishing Group. 2017;7:e017280.
Alev L, Fujikoshi S, Yoshikawa A, Enomoto H, Ishida M, Tsuji T, Ogawa K, Konno S Duloxetine 60 mg for chronic low back pain: post hoc responder analysis of double-blind, placebo-controlled trials. J Pain Res. Dove Press; 2017;10:1723–1731.
Tsuji T, Itoh N, Ishida M, Ochiai T, Konno S. Response to duloxetine in chronic low back pain: exploratory post hoc analysis of a Japanese phase III randomized study. J Pain Res. 2017;10:2157–68.
Enomoto H, Fujikoshi S, Funai J, Sasaki N, Ossipov M, Tsuji T, et al. Assessment of direct analgesic effect of duloxetine for chronic low back pain: post hoc path analysis of double-blind, placebo-controlled studies. J Pain Res. 2017;10:1357–68.
Lunn MP, Hughes RA, Wiffen PJ. Duloxetine for treating painful neuropathy or chronic pain. In: Lunn MP, editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd; 2009. p. CD007 115.
Murakami M, Osada K, Mizuno H, Ochiai T, Alev L, Nishioka K. A randomized, double-blind, placebo-controlled phase III trial of duloxetine in Japanese fibromyalgia patients. Arthritis Res Ther BioMed Central. 2015;17:224.
Welsch P, Üçeyler N, Klose P, Walitt B, Häuser W. Serotonin and noradrenaline reuptake inhibitors (SNRIs) for fibromyalgia. Cochrane Database Syst Rev Wiley-Blackwell. 2018;2:CD010292.
Gilron I, Chaparro LE, Tu D, Holden RR, Milev R, Towheed T, et al. Combination of pregabalin with duloxetine for fibromyalgia. Pain. 2016;157:1532–40.
Attia JZ, Mansour HS. Perioperative duloxetine and etoricoxibto improve postoperative pain after lumbar laminectomy: a randomized, double-blind, controlled study. BMC Anesthesiol BioMed Central. 2017;17:162.
YaDeau JT, Brummett CM, Mayman DJ, Lin Y, Goytizolo EA, Padgett DE, et al. Duloxetine and subacute pain after knee arthroplasty when added to a multimodal analgesic regimen. Anesthesiology The American Society of Anesthesiologists. 2016;125:561–72.
Forest Pharmaceuticals I. SAVELLA® Tablets (milnacipran HCl) [Internet]. PRESCRIBING INFORMATION. 2011. p. 1–27.
Keks NA, Hope J, Keogh S, Copolov DL. Milnacipran: serotonin-noradrenaline reuptake inhibitor approved for fibromyalgia may be a useful antidepressant. Australas Psychiatry. 2018;26:537–40.
Derry S, Phillips T, Moore RA, Wiffen PJ. Milnacipran for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;(7):CD011789.
Cording M, Derry S, Phillips T, Moore RA, Wiffen PJ. Milnacipran for pain in fibromyalgia in adults. Cochrane Database Syst Rev. 2015;(10):CD008244.
Pickering G, Macian N, Delage N, Picard P, Cardot J-M, Sickout-Arondo S, et al. Milnacipran poorly modulates pain in patients suffering from fibromyalgia: a randomized double-blind controlled study. Drug Des Devel Ther. 2018;12:2485–96.
Petzke F, Jensen KB, Kosek E, Choy E, Carville S, Fransson P, et al. Using fMRI to evaluate the effects of milnacipran on central pain processing in patients with fibromyalgia. Scand J Pain. 2013;4:65–74.
Wyeth Pharmaceuticals. EFFEXOR - venlafaxine hydrochloride tablet [Internet]. Wyeth Pharmaceuticals Inc. 2008. p. 1–21.
Gallagher HC, Gallagher RM, Butler M, Buggy DJ, Henman MC. Venlafaxine for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;(8):CD011091.
Trouvin A-P, Perrot S, Lloret-Linares C. Efficacy of venlafaxine in neuropathic pain: a narrative review of optimized treatment. Clin Ther. 2017;39:1104–22.
Farshchian N, Alavi A, Heydarheydari S, Moradian N. Comparative study of the effects of venlafaxine and duloxetine on chemotherapy-induced peripheral neuropathy. Cancer Chemother Pharmacol. 2018;82:787–93.
Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J. 2001;18(4):236–41.
Trindade E, Menon D, Topfer LA, Coloma C. Adverse effects associated with selective serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis. CMAJ. 1998;159(10):1245–52.
Lynch R. Tricyclic antidepressant overdose. Emerg Med J. 2002;19:596.
Hiroki T, Suto T, Saito S, Obata H. Repeated administration of amitriptyline in neuropathic pain. Anesth Analg. 2017;125:1281–8.
Moore RA, Derry S, Aldington D, Cole P, Wiffen PJ. Amitriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;(7):CD008242.
Derry S, Wiffen PJ, Aldington D, Moore RA. Nortriptyline for neuropathic pain in adults. Cochrane Database Syst Rev. 2015;1:CD011209.
Liu W-Q, Kanungo A, Toth C. Equivalency of tricyclic antidepressants in open-label neuropathic pain study. Acta Neurol Scand Wiley/Blackwell (10.1111). 2014;129:132–41.
Blier P, Abbott F. Putative mechanisms of action of antidepressant drugs in affective and anxiety disorders and pain. J Psychiatry Neurosci. 2001;26:37–43.
Slack SE, Pezet S, McMahon SB, Thompson SWN, Malcangio M. Brain-derived neurotrophic factor induces NMDA receptor subunit one phosphorylation via ERK and PKC in the rat spinal cord. Eur J Neurosci. 2004;20:1769–78.
Henneberger C, Jüttner R, Rothe T, Grantyn R. Postsynaptic action of BDNF on GABAergic synaptic transmission in the superficial layers of the mouse superior colliculus. J Neurophysiol. 2002;88:595–603.
Lee B-H, Kim Y-K. The roles of BDNF in the pathophysiology of major depression and in antidepressant treatment. Psychiatry Investig. 2010;7:231–5.
U.S. Food and Drug Administration (FDA). Abnormal heart rhythms associated with high doses of Celexa (citalopram hydrobromide) [Internet]. FDA Drug Safety Communication. 2017. p. 1.
Research. C for DE and. Drug safety and availability - FDA drug safety communication: selective serotonin reuptake inhibitor (SSRI) antidepressant use during pregnancy and reports of a rare heart and lung condition in newborn babies. U S food drug Adm home page. Cent Drug Eval Res. 2011.
Patetsos E, Horjales-Araujo E. Treating chronic pain with SSRIs: what do we know? Pain Res Manag. 2016;2016:2020915.
Hamdy MM, Elbadr MM, Barakat A. Fluoxetine uses in nociceptive pain management: a promising adjuvant to opioid analgesics. Fundam Clin Pharmacol. 2018;32:532–46.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ivan Urits, Jacquelin Peck, Mariam Salisu Orhurhu, John Wolf, Riki Patel, Vwaire Orhurhu, and Omar Viswanath declare no conflict of interest. Alan D. Kaye discloses that he is on the Speakers Bureau for Depomed, Inc. and Merck.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Other Pain
Rights and permissions
About this article
Cite this article
Urits, I., Peck, J., Orhurhu, M.S. et al. Off-label Antidepressant Use for Treatment and Management of Chronic Pain: Evolving Understanding and Comprehensive Review. Curr Pain Headache Rep 23, 66 (2019). https://doi.org/10.1007/s11916-019-0803-z
Published:
DOI: https://doi.org/10.1007/s11916-019-0803-z