Abstract
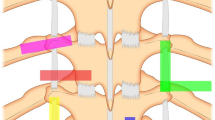
Chronic pain is a common medical condition. Patients who suffer uncontrolled chronic pain may require interventions including spinal injections and various nerve blocks. Interventional procedures have evolved and improved over time since epidural injection was first introduced for low back pain and sciatica in 1901. One of the major contributors in the improvement of these interventions is the advancement of imaging guidance technologies. The utilization of image guidance has dramatically improved the accuracy and safety of these interventions. The first image guidance technology adopted by pain specialists was fluoroscopy. This was followed by CT and ultrasound. Fluoroscopy can be used to visualize bony structures of the spine. It is still the most commonly used guidance technology in spinal injections. In the recent years, ultrasound guidance has been increasingly adopted by interventionists to perform various injections. Because its ability to visualize soft tissue, vessels, and nerves, this guidance technology appears to be a better option than fluoroscopy for interventions including SGB and celiac plexus blocks, when visualization of the vessels may prevent intravascular injection. The current evidence indicates the efficacies of these interventions are similar between ultrasound guidance and fluoroscopy guidance for SGB and celiac plexus blocks. For facet injections and interlaminar epidural steroid injections, it is important to visualize bony structures in order to perform these procedures accurately and safely. It is worth noting that facet joint injections can be done under ultrasound guidance with equivalent efficacy to fluoroscopic guidance. However, obese patients may present challenge for ultrasound guidance due to its poor visualization of deep anatomical structures. Regarding transforaminal epidural steroid injections, there are limited evidence to support that ultrasound guidance technology has equivalent efficacy and less complications comparing to fluoroscopy. However, further studies are required to prove the efficacy of ultrasound-guided transforaminal epidural injections. SI joint is unique due to its multiplanar orientation, irregular joint gap, partial ankylosis, and thick dorsal and interosseous ligament. Therefore, it can be difficult to access the joint space with fluoroscopic guidance and ultrasound guidance. CT scan, with its cross-sectional images, can identify posterior joint gap, is most likely the best guidance technology for this intervention. Intercostal nerves lie in the subcostal grove close to the plural space. Significant risk of pneumothorax is associated with intercostal blocks. Ultrasound can provide visualization of ribs and pleura. Therefore, it may improve the accuracy of the injection and reduce the risk of pneumothorax. At present time, most pain specialists are familiar with fluoroscopic guidance techniques, and fluoroscopic machines are readily available in the pain clinics. In the contrast, CT guidance can only be performed in specially equipped facilities. Ultrasound machine is generally portable and inexpensive in comparison to CT scanner and fluoroscopic machine. As pain specialists continue to improve their patient care, ultrasound and CT guidance will undoubtedly be incorporated more into the pain management practice. This review is based on a paucity of clinical evidence to compare these guidance technologies; clearly, more clinical studies is needed to further elucidate the pro and cons of each guidance method for various pain management interventions.
Similar content being viewed by others
References
Papers of Particular Interest, Published Recently, Have Been Highlighted as: • Of importance •• Of major importance
Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. https://doi.org/10.1001/jama.2013.13805.
Elias M. Cervical sympathetic and stellate ganglion blocks. Pain Physician. 2000;3(3):294–304.
Abdi S, Zhou Y, Patel N, Saini B, Nelson JA. New and easy technique to block the stellate ganglion. Pain Physician. 2004;7(3):327–31.
Nabil Abbas D, Abd El Ghafar EM, Ibrahim WA, Omran AF. Fluoroscopic stellate ganglion block for postmastectomy pain: a comparison of the classic anterior approach and the oblique approach. Clin J Pain. 2011;27(3):207–13. https://doi.org/10.1097/AJP.0b013e3181fb1ef1.
Narouze SN. Ultrasound-guided cervical spine injections: ultrasound “prevents” whereas contrast fluoroscopy “detects” intravascular injections. Reg Anesth Pain Med. 2012;37(2):127–30. https://doi.org/10.1097/AAP.0b013e31823f3c80.
Narouze S, Vydyanathan A, Patel N. Ultrasound-guided stellate ganglion block successfully prevented esophageal puncture. Pain Physician. 2007;10(6):747–52.
Lee MH, Kim KY, Song JH, Jung HJ, Lim HK, Lee DI, et al. Minimal volume of local anesthetic required for an ultrasound-guided SGB. Pain Med. 2012;13(11):1381–8. https://doi.org/10.1111/j.1526-4637.2012.01495.x.
Mercadante S, Nicosia F. Celiac plexus block: a reappraisal. Reg Anesth Pain Med. 1998;23(1):37–48.
FK M. Sensitivity (means “pain sensation” in this context) and local anesthesia in the surgical area of the abdominal cavity, with special focus on anesthesia of the splanchnic nerve [Sensibilitat und lokale Anasthesieim chirurgischen Gebiet der Bauchhohle mit besonderer Berucksichtigung der splanchnicus–Aasthesie]. Beitrage zur klinischen chirurgie. 1919;115:161–75.
Jacobs JB, Jackson SH, Doppman JL. A radiographic approach to celiac ganglion block. Radiology. 1969;92(6):1372–3. https://doi.org/10.1148/92.6.1372.
Buy JN, Moss AA, Singler RC. CT guided celiac plexus and splanchnic nerve neurolysis. J Comput Assist Tomogr. 1982;6(2):315–9. https://doi.org/10.1097/00004728-198204000-00016.
Haaga JR, Kori SH, Eastwood DW, Borkowski GP. Improved technique for CT-guided celiac ganglia block. AJR Am J Roentgenol. 1984;142(6):1201–4. https://doi.org/10.2214/ajr.142.6.1201.
Bhatnagar S, Joshi S, Rana SP, Mishra S, Garg R, Ahmed SM. Bedside ultrasound-guided celiac plexus neurolysis in upper abdominal cancer patients: a randomized, prospective study for comparison of percutaneous bilateral paramedian vs. unilateral paramedian needle-insertion technique. Pain Pract. 2014;14(2):E63–8. https://doi.org/10.1111/papr.12107.
Moore DC. Computed tomography eliminates paraplegia and/or death from neurolytic celiac plexus block. Reg Anesth Pain Med. 1999;24(5):483–6. https://doi.org/10.1016/S1098-7339(99)90027-5.
Moore DC. The dreaded complications from neurolytic celiac plexus blocks are preventable. Reg Anesth Pain Med. 2004;29(4):377–8. https://doi.org/10.1097/00115550-200407000-00016.
Wang PJ, Shang MY, Qian Z, Shao CW, Wang JH, Zhao XH. CT-guided percutaneous neurolytic celiac plexus block technique. Abdom Imaging. 2006;31(6):710–8. https://doi.org/10.1007/s00261-006-9153-5.
Moura RN, De Moura EG, Bernardo WM, Otoch JP, Bustamante FA, Albers DV, et al. Endoscopic-ultrasound versus percutaneous-guided celiac plexus block for chronic pancreatitis pain. A systematic review and meta-analysis. Rev Gastroenterol Peru. 2015;35(4):333–41.
Edelstein MR, Gabriel RT, Elbich JD, Wolfe LG, Sydnor MK. Pain outcomes in patients undergoing CT-guided celiac plexus neurolysis for intractable abdominal visceral pain. Am J Hosp Palliat Care. 2017;34(2):111–4. https://doi.org/10.1177/1049909115604670.
Gress F, Schmitt C, Sherman S, Ikenberry S, Lehman G. A prospective randomized comparison of endoscopic ultrasound- and computed tomography-guided celiac plexus block for managing chronic pancreatitis pain. Am J Gastroenterol. 1999;94(4):900–5. https://doi.org/10.1111/j.1572-0241.1999.01042.x.
Borenstein D. Does osteoarthritis of the lumbar spine cause chronic low back pain? Curr Pain Headache Rep. 2004;8(6):512–7. https://doi.org/10.1007/s11916-004-0075-z.
Manchikanti L. The growth of interventional pain management in the new millennium: a critical analysis of utilization in the medicare population. Pain Physician. 2004;7(4):465–82.
Bogduk N. International spinal injection society guidelines for the performance of spinal injection procedures. Part 1: zygapophysial joint blocks. Clin J Pain. 1997;13(4):285–302. https://doi.org/10.1097/00002508-199712000-00003.
Galiano K, Obwegeser AA, Bodner G, Freund M, Maurer H, Kamelger FS, et al. Ultrasound guidance for facet joint injections in the lumbar spine: a computed tomography-controlled feasibility study. Anesth Analg. 2005;101(2):579–583, table of contents. https://doi.org/10.1213/01.ANE.0000158609.64417.93.
Yun DH, Kim HS, Yoo SD, Kim DH, Chon JM, Choi SH, et al. Efficacy of ultrasonography-guided injections in patients with facet syndrome of the low lumbar spine. Ann Rehabil Med. 2012;36(1):66–71. https://doi.org/10.5535/arm.2012.36.1.66.
Wu T, Zhao WH, Dong Y, Song HX, Li JH. Effectiveness of ultrasound-guided versus fluoroscopy or computed tomography scanning guidance in lumbar facet joint injections in adults with facet joint syndrome: a meta-analysis of controlled trials. Arch Phys Med Rehabil. 2016;97(9):1558–63. https://doi.org/10.1016/j.apmr.2015.11.013.
Galiano K, Obwegeser AA, Walch C, Schatzer R, Ploner F, Gruber H. Ultrasound-guided versus computed tomography-controlled facet joint injections in the lumbar spine: a prospective randomized clinical trial. Reg Anesth Pain Med. 2007;32(4):317–22. https://doi.org/10.1016/j.rapm.2007.03.010.
Lutz GE, Vad VB, Wisneski RJ. Fluoroscopic transforaminal lumbar epidural steroids: an outcome study. Arch Phys Med Rehabil. 1998;79(11):1362–6. https://doi.org/10.1016/S0003-9993(98)90228-3.
Galiano K, Obwegeser AA, Bodner G, Freund M, Maurer H, Kamelger FS, et al. Real-time sonographic imaging for periradicular injections in the lumbar spine: a sonographic anatomic study of a new technique. J Ultrasound Med. 2005;24(1):33–8. https://doi.org/10.7863/jum.2005.24.1.33.
Jee H, Lee JH, Kim J, Park KD, Lee WY, Park Y. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: a randomized, blinded, controlled study. Skelet Radiol. 2013;42(1):69–78. https://doi.org/10.1007/s00256-012-1434-1.
Yang G, Liu J, Ma L, Cai Z, Meng C, Qi S, et al. Ultrasound-guided versus fluoroscopy-controlled lumbar transforaminal epidural injections: a prospective randomized clinical trial. Clin J Pain. 2016;32(2):103–8. https://doi.org/10.1097/AJP.0000000000000237.
Schwarzer AC, Aprill CN, Bogduk N. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976). 1995;20(1):31–7. https://doi.org/10.1097/00007632-199501000-00007.
• Narouze S, Peng PW. Ultrasound-guided interventional procedures in pain medicine: a review of anatomy, sonoanatomy, and procedures. Part II: axial structures. Reg Anesth Pain Med. 2010;35(4):386–96. A very good review with excellent descriptions of various ultrasound guided interventional pain management procedures.
Hartung W, Ross CJ, Straub R, Feuerbach S, Scholmerich J, Fleck M, et al. Ultrasound-guided sacroiliac joint injection in patients with established sacroiliitis: precise IA injection verified by MRI scanning does not predict clinical outcome. Rheumatology (Oxford). 2010;49(8):1479–82. https://doi.org/10.1093/rheumatology/kep424.
Jee H, Lee JH, Park KD, Ahn J, Park Y. Ultrasound-guided versus fluoroscopy-guided sacroiliac joint intra-articular injections in the noninflammatory sacroiliac joint dysfunction: a prospective, randomized, single-blinded study. Arch Phys Med Rehabil. 2014;95(2):330–7. https://doi.org/10.1016/j.apmr.2013.09.021.
Walker JM. The sacroiliac joint: a critical review. Phys Ther. 1992;72(12):903–16. https://doi.org/10.1093/ptj/72.12.903.
Gupta S. Double needle technique: an alternative method for performing difficult sacroiliac joint injections. Pain Physician. 2011;14(3):281–4.
Pulisetti D, Ebraheim NA. CT-guided sacroiliac joint injections. J Spinal Disord. 1999;12(4):310–2.
Braun J, Bollow M, Seyrekbasan F, Haberle HJ, Eggens U, Mertz A, et al. Computed tomography guided corticosteroid injection of the sacroiliac joint in patients with spondyloarthropathy with sacroiliitis: clinical outcome and followup by dynamic magnetic resonance imaging. J Rheumatol. 1996;23(4):659–64.
Bollow M, Braun J, Taupitz M, Haberle J, Reibhauer BH, Paris S, et al. CT-guided intraarticular corticosteroid injection into the sacroiliac joints in patients with spondyloarthropathy: indication and follow-up with contrast-enhanced MRI. J Comput Assist Tomogr. 1996;20(4):512–21. https://doi.org/10.1097/00004728-199607000-00002.
Kissoon NR, Graff-Radford J, Watson JC, Laughin RS. Spinal cord injury from fluoroscopically guided intercostal blocks with phenol. Pain Physician. 2014;17(2):E219–24.
Gollapalli L, Muppuri R. Paraplegia after intercostal neurolysis with phenol. J Pain Res. 2014;7:665–8. https://doi.org/10.2147/JPR.S63570.
Kowalewski R, Schurch B, Hodler J, Borgeat A. Persistent paraplegia after an aqueous 7.5% phenol solution to the anterior motor root for intercostal neurolysis: a case report. Arch Phys Med Rehabil. 2002;83(2):283–5. https://doi.org/10.1053/apmr.2002.27477.
•• Bhatia A, Gofeld M, Ganapathy S, Hanlon J, Johnson M. Comparison of anatomic landmarks and ultrasound guidance for intercostal nerve injections in cadavers. Reg Anesth Pain Med. 2013;38(6):503–7. https://doi.org/10.1097/AAP.0000000000000006. A well designed study that provided clear evidence to support ultrasound guidance for intercostal nerve blocks.
Luo M, Liu X, Ning L, Sun Y, Cai Y, Shen S. Comparison of ultrasonography-guided bilateral intercostal nerve blocks and conventional patient-controlled intravenous analgesia for pain control after the Nuss procedure in children: a prospective randomized study. Clin J Pain. 2017;33(7):604–10. https://doi.org/10.1097/AJP.0000000000000449.
Shankar H, Eastwood D. Retrospective comparison of ultrasound and fluoroscopic image guidance for intercostal steroid injections. Pain Pract. 2010;10(4):312–7. https://doi.org/10.1111/j.1533-2500.2009.00345.x.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Anesthetic Techniques in Pain Management
Rights and permissions
About this article
Cite this article
Wang, D. Image Guidance Technologies for Interventional Pain Procedures: Ultrasound, Fluoroscopy, and CT. Curr Pain Headache Rep 22, 6 (2018). https://doi.org/10.1007/s11916-018-0660-1
Published:
DOI: https://doi.org/10.1007/s11916-018-0660-1