Abstract
Objectives
To compare the short-term effects and advantages of ultrasound-guided selective nerve root block with fluoroscopy-guided transforaminal epidural block for radicular pain in the lower cervical spine through assessment of pain relief, functional improvement, and safety.
Methods
A total of 120 patients with radicular pain from cervical spinal stenosis or cervical herniated disc were enrolled. All procedures were performed using a fluoroscopy or ultrasound apparatus. The subjects were randomly assigned to either the fluoroscopy (FL) or ultrasound (US) group. The complication frequencies during the procedures, treatment effects, and functional improvement of the nerve root block were compared at 2 and 12 weeks after the procedures.
Results
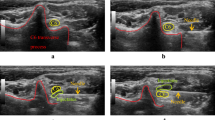
Verbal Numeric Pain Scale (VNS) improved 2 weeks and 12 weeks after the injections in both groups. Statistical differences were not observed in VNS, Neck Disability Index (NDI), and effectiveness between the groups. In 21 patients at US, vessels were identified at the anterior aspect of the foramen. Eleven patients had a critical vessel at the posterior aspect of the foramen and five patients had on artery continue medially into the foramen, forming, or joining a segmental feeder artery. In both cases, the vessels might well have been in the pathway of the needle correctly positioned under fluoroscopic guidance. Five cases of intravascular injections were observed only in FL without significant difference between the groups.
Conclusions
The US-guided method may facilitate identifying critical vessels at unexpected locations relative to the intervertebral foramen and avoiding injury to such vessels, which is the leading cause of the reported complications from cervical transforaminal injections. On treatment effect, using either method of epidural injections to deliver steroids for cervical radicular pain, secondary to herniated intervertebral disc or foraminal stenosis, significant improvements in function and pain relief were observed in both groups after the intervention. However, significant difference was not observed between the groups. Therefore, the ultrasound-guided method was shown to be as effective as the fluoroscopy-guided method in pain relief and functional improvement, in addition to the absence of radiation and avoiding vessel injury at real-time imaging.



Similar content being viewed by others
References
Bush K, Hiller S. Outcome of cervical radiculopathy treated with periradicular/epidural corticosteroid injections: a prospective study with independent clinical review. Eur Spine J. 1996;5:319–25.
Slipman CW, Lipetz JS, Jackson HB, et al. Therapeutic selective nerve root block in the nonsurgical treatment of atraumatic cervical spondylotic radicular pain: a retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000;81:741–6.
Sung DH. Selective nerve root injection of steroids in cervical radiculopathy: a prospective case series. Poster presentation. AAPM&R. November 4, 2000.
Marshall LL, Trethewie ER, Curtain CC. Chemical radiculitis: a clinical, physiological, and immunological study. Clin Orthop. 1977;190:61–7.
Rathmell JP, Aprill C, Bogduk N. Cervical transforaminal injection of steroids Anesthesiology. 2004;100:1595–1600.
Tiso RL, Cutler T, Catania JA, Whalen K. Adverse central nervous system sequelae after selective transforaminal block: the role of corticosteroids. Spine. 2004;4:468–74.
Baker R, Dreyfuss P, Mercer S, Bogduk N. Cervical transforaminal injections of corticosteroids into a radicular artery: a possible mechanism for spinal cord injury. Pain. 2003;103:211–5.
Galiano K, Obwegeser AA, Bodner G, et al. Ultrasound-guided periradicular injections in the middle to lower cervical spine: an imaging study of a new approach. Reg Anesth Pain Med. 2005;30:391–6.
Narouze SN, Vydyanathan A, Kapural L, Sessler DI, Mekhail N. Ultrasound-guided cervical selective nerve root block: a fluoroscopy-controlled feasibility study. Reg Anesth Pain Med. 2009;34:343–8.
Yamauchi M, Suzuki D, Niiya T, Honma H, Tachibana N, Watanabe A, Fujimiya M, Yamakage M. Ultrasound-Guided Cervical Nerve Root Block: Spread of Solution and Clinical Effect. Pain Med. 2011 Jun 21. doi: 10.1111/j.1526-4637.2011.01170.x.
Galiano K, Obwegeser AA, Walch C, Schatzer R, Ploner F, Gruber H. Ultrasound-guided versus computed tomography-controlled facet joint injections in the lumbar spine: a prospective randomized clinical trial. Reg Anesth Pain Med. 2007;32:317–22.
Martinoli C, Bianchi S, Santacroce E, Pugliese F, Graif M, Derchi LE. Brachial plexus sonography: a technique for assessing the root level. AJR Am J Roentgenol. 2002;179:699–702.
Smuck M, Maxwell MD, Kennedy D, Rittenberg JD, Lansberg MG, Plastaras CT. Utility of the anesthetic test dose to avoid catastrophic injury during cervical transforaminal epidural injections. Spine J. 2010;10:857–64.
Nahm FS, Lee CJ, Lee SH, Kim TH, Sim WS, Cho HS, Park SY, Kim YC, Lee SC. Risk of intravascular injection in transforaminal epidural injections. Anaesth. 2010;65:917–21. doi:10.1111/j.1365-2044.2010.06447.x.
Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003;3:310–6.
Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–15.
Browner WS, Newman TB, Cummings SR, Hulley SB. Estimating sample size and power. In: Hulley SB, Cummings SR, Browner WS, Grady D, Hearst N, Newman TB, editors. Designing Clinical Research: An Epidemiologic Approach, 2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2001. p. 65–84.
Manchikanti L, Singh V, Falco FJ, Cash KA, Fellows B. Cervical medial branch blocks for chronic cervical facet joint pain: a randomized double-blind, controlled trial with one-year follow-up. Spine (Phila Pa 1976). 2008;33:1813–20.
Manchikanti L, Singh V, Falco FJE, Cash KA, Pampati V. Effectiveness of thoracic medial branch blocks in managing chronic pain: a preliminary report of a randomized, double-blind controlled trial: Clinical trial NCT00355706. Pain Physician. 2008;11:491–504.
Manchikanti L, Cash KA, McManus CD, Pampati V, Smith HS. Preliminary results of randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 1. Discogenic pain without disc herniation or radiculitis. Pain Physician. 2008;11:785–800.
Manchikanti L, Singh V, Cash KA, Pampati V, Damron KS, Boswell MV. Preliminary results of randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 2. Disc herniation and radiculitis. Pain Physician. 2008;11:801–15.
Manchikanti L, Singh V, Cash KA, Pampati V, Datta S. Preliminary results of randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: Part 3. Post surgery syndrome. Pain Physician. 2008;11:817–31.
Wallace MA, Fukui MB, Williams RL, Ku A, Baghai P. Complications of cervical selective nerve root blocks performed with fluoroscopic guidance. Am J Roentgenol. 2007;188:1218–21.
Brouwers PJ, Kottink EJ, Simon MA, Prevo RL. A cervical anterior spinal artery syndrome after diagnostic blockade of the right C6-nerve root. Pain. 2001;91:397–9.
Ma DJ, Gilula LA, Riew KD. Complications of fluoroscopically guided extraforaminal cervical nerve blocks. An analysis of 1036 injections. J Bone Joint Surg Am. 2005;87:1025–30.
Furman MB, Giovanniello MT, O’Brien EM. Incidence of intravascular penetration in transforaminal cervicalepidural steroid injections. Spine. 2003;28:21–5.
Huntoon MA. Anatomy of the cervical intervertebral foramina: vulnerable arteries and ischemic neurologic2005;117:104–111.
Narouze S. Ultrasonography in pain medicine: a sneak peak at the future. Pain Pract. 2008;8:223–5.
Narouze SN. Ultrasound-guided interventional procedures in pain management: evidence-based medicine. Reg Anesth Pain Med. 2010;35(2 Suppl):S55–58.
Sullivan WJ, Willick SE, Chira-Adisai W, et al. Incidence of intravascular uptake in lumbar spinal injection procedures. Spine. 2000;25:481–6.
Furman MB, O’Brien EM, Zgleszewski TM. Incidence of intravascular penetration in transforaminal lumbosacral epidural steroid injections. Spine. 2000;25:2628–32.
Smuck M, Fuller BJ, Yoder B, et al. Incidence of simultaneous epidural and vascular injection during lumbosacral transforaminal epidural injections. Spine J. 2007;7:79–82.
Houten JK, Errico TJ. Paraplegia after lumbosacral nerve root block: report of three cases. Spine J. 2002;2:70–5.
Breslin DS, Martin G, MacLeod DB, et al. Central nervous system toxicity following the administration of levobupivacaine for lumbar plexus block: a report of two cases. Reg Anesth Pain Med. 2003;28:144–7.
Smuck M, Fuller BJ, Chiodo A, Benny B, Singaracharlu B, Tong H, Ho S. Accuracy of intermittent fluoroscopy to detect intravascular injection during transforaminal epidural injections. Spine (Phila Pa 1976). 2008;33:E205–210.
Derby R, Lee SH, Date ES, Lee JH, Lee CH. Size and aggregation of corticosteroids used for epidural injections. Pain Med. 2008;9:227–34.
Muro K, O'Shaughnessy B, Ganju A. Infarction of the cervical spinal cord following multilevel transforaminal epidural steroid injection: case report and review of the literature. J Spinal Cord Med. 2007;30:385–8.
Scanlon GC, Moeller-Bertram T, Romanowsky SM, et al. Cervical transforaminal epidural steroid injections: more dangerous than we think? Spine. 2007;32:1249–56.
Malhotra G, Abbasi A, Rhee M. Complications of transforaminal cervical epidural steroid injections. Spine (Phila Pa 1976). 2009;34(7):731–9.
Furman MB, Mehta AR, Kim RE, Simon JI, Patel R, Lee TS, Reeves RS. Injectate volumes needed to reach specific landmarks in lumbar transforaminal epidural injections. PM R. 2010;2:625–35.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jee, H., Lee, J.H., Kim, J. et al. Ultrasound-guided selective nerve root block versus fluoroscopy-guided transforaminal block for the treatment of radicular pain in the lower cervical spine: A randomized, blinded, controlled study. Skeletal Radiol 42, 69–78 (2013). https://doi.org/10.1007/s00256-012-1434-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-012-1434-1