Abstract
Purpose of Review
Diabetes is associated with an increased risk for several types of cancer. Therefore, use of antihyperglycemic medications to lower blood glucose may modify cancer risk. Here we review available data on the link between the most common classes of antihyperglycemic agents and cancer risk among patients with diabetes.
Recent Findings
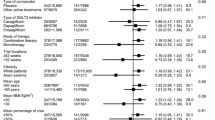
A database search was conducted between February 2022 and June 2022 on PubMed and Embase for systematic reviews and meta-analyses investigating the association between antihyperglycemic agents and risk of cancer. Use of biguanides such as metformin is associated with 20–30% lower risk for all cancer incidence, and somewhat greater benefit for cancer-related mortality. Alpha-glucosidase inhibitors, e.g., acarbose, have not been consistently associated with cancer. Similarly, no consistent effects have been reported for thiazolidinediones, but the relationship with cancer seems to depend on the type of drug, dose, and duration of treatment. Exposure to various types of incretin-based therapies (glucagon-like peptide-1 agonists and dipeptidyl peptidase-4 inhibitors) has not been found to significantly modify cancer risk. Inhibitors of sodium glucose cotransporter-2 may raise risk for bladder cancer and reduce risk for gastrointestinal cancer. Use of insulin and insulin analogs is associated with a significant increase in total cancer risk by almost 50% compared to other antihyperglycemic drugs. Likewise, insulin secretagogues like sulfonylureas have generally been linked to greater risk for cancer by ~ 20%, although these associations may be agent-specific and dose-dependent.
Summary
Current evidence suggests that the risk of cancer associated with the use of antihyperglycemic medications among patients with diabetes depends on the class of drug and type of agent, dosage, and duration of treatment. More research is needed to delineate the mechanisms by which these agents affect the process of carcinogenesis.
Similar content being viewed by others
Data Availability
This article does not contain any primary data.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–98. https://doi.org/10.1038/s41574-019-0176-8.
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10. https://doi.org/10.1016/j.metabol.2018.09.005.
World Health Organization. Obesity and overweight; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 23 Nov 2022.
Atawia RT, Bunch KL, Toque HA, Caldwell RB, Caldwell RW. Mechanisms of obesity-induced metabolic and vascular dysfunctions. Front Biosci. 2019;24:890–934. https://doi.org/10.2741/4758.
Martyn JA, Kaneki M, Yasuhara S. Obesity-induced insulin resistance and hyperglycemia: etiologic factors and molecular mechanisms. Anesthesiology. 2008;109:137–48. https://doi.org/10.1097/ALN.0b013e3181799d45.
Kasuga M. Insulin resistance and pancreatic beta cell failure. J Clin Invest. 2006;116:1756–60. https://doi.org/10.1172/jci29189.
World Health Organization. Obesity-complications; 2022. Available from: https://www.who.int/health-topics/obesity#tab=tab_2. Accessed 23 Nov 2022.
International Diabetes Federation. Diabetes atlas, 10 edn. Brussels: International Diabetes Federation; 2021. Available from: https://diabetesatlas.org/atlas/tenth-edition/. Accessed 23 Nov 2022.
World Health Organization. Diabetes; 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes. Accessed 23 Nov 2022.
Giri B, Dey S, Das T, Sarkar M, Banerjee J, Dash SK. Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: an update on glucose toxicity. Biomed Pharmacother. 2018;107:306–28. https://doi.org/10.1016/j.biopha.2018.07.157.
Cade WT. Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther. 2008;88:1322–35. https://doi.org/10.2522/ptj.20080008.
International Diabetes Federation. Diabetes complications; 2020. Available from: https://www.idf.org/aboutdiabetes/complications.html. Accessed 23 Nov 2022.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, et al. Management of hyperglycemia in type 2 diabetes, 2018 — a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41:2669–701. https://doi.org/10.2337/dci18-0033.
Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, et al. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33:1674–85. https://doi.org/10.2337/dc10-0666.
Wojciechowska J, Krajewski W, Bolanowski M, Kręcicki T, Zatoński T. Diabetes and cancer: a review of current knowledge. Exp Clin Endocrinol Diabetes. 2016;124:263–75. https://doi.org/10.1055/s-0042-100910.
Zelenko Z, Gallagher EJ. Diabetes and cancer. Endocrinol Metab Clin North Am. 2014;43:167–85. https://doi.org/10.1016/j.ecl.2013.09.008.
Karlstad O, Starup-Linde J, Vestergaard P, Hjellvik V, Bazelier MT, Schmidt MK, et al. Use of insulin and insulin analogs and risk of cancer — systematic review and meta-analysis of observational studies. Curr Drug Saf. 2013;8:333–48. https://doi.org/10.2174/15680266113136660067.
Dahlén AD, Dashi G, Maslov I, Attwood MM, Jonsson J, Trukhan V, et al. Trends in antidiabetic drug discovery: FDA approved drugs, new drugs in clinical trials and global sales. Front Pharmacol. 2021;12:807548. https://doi.org/10.3389/fphar.2021.807548 (An updated review of currently available antihyperglycemic pharmacotherapies and future developments.).
Haas B, Eckstein N, Pfeifer V, Mayer P, Hass MD. Efficacy, safety and regulatory status of SGLT2 inhibitors: focus on canagliflozin. Nutr Diabetes. 2014;4: e143. https://doi.org/10.1038/nutd.2014.40.
Srivastava SP, Goodwin JE. Cancer biology and prevention in diabetes. Cells. 2020;9(6):1380. https://doi.org/10.3390/cells9061380 (A review of our understanding of the mechanistic links between diabetes and cancer.).
Alsaggaf R, Pfeiffer RM, Wang Y, St George DMM, Zhan M, Wagner KR, et al. Diabetes, metformin and cancer risk in myotonic dystrophy type I. Int J Cancer. 2020;147:785–92. https://doi.org/10.1002/ijc.32801 (A case-control study in more than 13,000 people demonstrating that diabetes confers increased cancer risk in patients with myotonic dystrophy type I but this increase is abolished among those treated with metformin.).
Wang Z, Bao C, Su C, Xu W, Luo H, Chen L, et al. Association between diabetes or antidiabetic therapy and lung cancer: a meta-analysis. J Diabetes Investig. 2013;4:659–66. https://doi.org/10.1111/jdi.12112.
Evans JMM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD. Metformin and reduced risk of cancer in diabetic patients. BMJ. 2005;330:1304–5. https://doi.org/10.1136/bmj.38415.708634.F7.
Bowker SL, Majumdar SR, Veugelers P, Johnson JA. Increased cancer-related mortality for patients with type 2 diabetes who use sulfonylureas or insulin. Diabetes Care. 2006;29:254–8. https://doi.org/10.2337/diacare.29.02.06.dc05-1558.
Zhang K, Bai P, Dai H, Deng Z. Metformin and risk of cancer among patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Prim Care Diabetes. 2021;15:52–8. https://doi.org/10.1016/j.pcd.2020.06.001 (A recent systematic review with meta-analysis of 67 studies with more than 10 million patients with diabetes, demonstrating that (i) those who have ever used metformin have 30% lower risk than those who have never used metofrmin, and (ii) metformin is associated with 20% lower risk compared with other antidiabetic medications.).
Ng CW, Jiang AA, Toh EMS, Ng CH, Ong ZH, Peng S, et al. Metformin and colorectal cancer: a systematic review, meta-analysis and meta-regression. Int J Colorectal Dis. 2020;35:1501–12. https://doi.org/10.1007/s00384-020-03676-x (A recent systematic review with meta-analysis of 58 studies in about 1.8 million patients with type 2 diabetes showing that metformin use is associated with reduced incidence of, and improved survival from, colorectal cancer.).
Farmer RE, Ford D, Forbes HJ, Chaturvedi N, Kaplan R, Smeeth L, et al. Metformin and cancer in type 2 diabetes: a systematic review and comprehensive bias evaluation. Int J Epidemiol. 2017;46:728–44. https://doi.org/10.1093/ije/dyw275.
Franciosi M, Lucisano G, Lapice E, Strippoli GF, Pellegrini F, Nicolucci A. Metformin therapy and risk of cancer in patients with type 2 diabetes: systematic review. PLoS ONE. 2013;8:e71583. https://doi.org/10.1371/journal.pone.0071583.
Dowling RJO, Zakikhani M, Fantus IG, Pollak M, Sonenberg N. Metformin inhibits mammalian target of rapamycin–dependent translation initiation in breast cancer cells. Cancer Res. 2007;67:10804–12. https://doi.org/10.1158/0008-5472.Can-07-2310.
Shaw RJ, Lamia KA, Vasquez D, Koo S-H, Bardeesy N, DePinho RA, et al. The kinase LKB1 mediates glucose homeostasis in liver and therapeutic effects of metformin. Science. 2005;310:1642–6. https://doi.org/10.1126/science.1120781.
Shackelford DB, Shaw RJ. The LKB1–AMPK pathway: metabolism and growth control in tumour suppression. Nat Rev Cancer. 2009;9:563–75. https://doi.org/10.1038/nrc2676.
Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia. 2017;60:1577–85. https://doi.org/10.1007/s00125-017-4342-z.
Wu L, Zhu J, Prokop LJ, Murad MH. Pharmacologic therapy of diabetes and overall cancer risk and mortality: a meta-analysis of 265 studies. Sci Rep. 2015;5:10147. https://doi.org/10.1038/srep10147.
Tseng YH, Tsan YT, Chan WC, Sheu WH, Chen PC. Use of an alpha-glucosidase inhibitor and the risk of colorectal cancer in patients with diabetes: a nationwide, population-based cohort study. Diabetes Care. 2015;38:2068–74. https://doi.org/10.2337/dc15-0563.
Valent F. Diabetes mellitus and cancer of the digestive organs: an Italian population-based cohort study. J Diabetes Complicat. 2015;29:1056–61. https://doi.org/10.1016/j.jdiacomp.2015.07.017.
Zhao Y, Wang Y, Lou H, Shan L. Alpha-glucosidase inhibitors and risk of cancer in patients with diabetes mellitus: a systematic review and meta-analysis. Oncotarget. 2017;8:81027–39. https://doi.org/10.18632/oncotarget.17515.
Chen YL, Cheng KC, Lai SW, Tsai IJ, Lin CC, Sung FC, et al. Diabetes and risk of subsequent gastric cancer: a population-based cohort study in Taiwan. Gastric Cancer. 2013;16:389–96. https://doi.org/10.1007/s10120-012-0197-7.
Lai SW, Liao KF, Chen PC, Tsai PY, Hsieh DP, Chen CC. Antidiabetes drugs correlate with decreased risk of lung cancer: a population-based observation in Taiwan. Clin Lung Cancer. 2012;13:143–8. https://doi.org/10.1016/j.cllc.2011.10.002.
Lin CM, Huang HL, Chu FY, Fan HC, Chen HA, Chu DM, et al. Association between gastroenterological malignancy and diabetes mellitus and anti-diabetic therapy: a nationwide, population-based cohort study. PLoS ONE. 2015;10: e0125421. https://doi.org/10.1371/journal.pone.0125421.
Chang CH, Lin JW, Wu LC, Lai MS, Chuang LM, Chan KA. Association of thiazolidinediones with liver cancer and colorectal cancer in type 2 diabetes mellitus. Hepatology. 2012;55:1462–72. https://doi.org/10.1002/hep.25509.
Bosco JL, Antonsen S, Sorensen HT, Pedersen L, Lash TL. Metformin and incident breast cancer among diabetic women: a population-based case-control study in Denmark. Cancer Epidemiol Biomark Prev. 2011;20:101–11. https://doi.org/10.1158/1055-9965.EPI-10-08170.
Chen YC, Kok VC, Chien CH, Horng JT, Tsai JJ. Cancer risk in patients aged 30 years and above with type 2 diabetes receiving antidiabetic monotherapy: a cohort study using metformin as the comparator. Ther Clin Risk Manag. 2015;11:1315–23. https://doi.org/10.2147/TCRM.S91513.
Chiu CC, Huang CC, Chen YC, Chen TJ, Liang Y, Lin SJ, et al. Increased risk of gastrointestinal malignancy in patients with diabetes mellitus and correlations with anti-diabetes drugs: a nationwide population-based study in Taiwan. Intern Med. 2013;52:939–46. https://doi.org/10.2169/internalmedicine.52.8276.
Dabrowski M, Szymanska-Garbacz E, Miszczyszyn Z, Derezinski T, Czupryniak L. Risk factors for cancer development in type 2 diabetes: a retrospective case-control study. BMC Cancer. 2016;16:785. https://doi.org/10.1186/s12885-016-2836-6.
Kawaguchi T, Taniguchi E, Morita Y, Shirachi M, Tateishi I, Nagata E, et al. Association of exogenous insulin or sulphonylurea treatment with an increased incidence of hepatoma in patients with hepatitis C virus infection. Liver Int. 2010;30:479–86. https://doi.org/10.1111/j.1478-3231.2009.02191.x.
Kawamori R, Inagaki N, Araki E, Watada H, Hayashi N, Horie Y, et al. Linagliptin monotherapy provides superior glycaemic control versus placebo or voglibose with comparable safety in Japanese patients with type 2 diabetes: a randomized, placebo and active comparator-controlled, double-blind study. Diabetes Obes Metab. 2012;14:348–57. https://doi.org/10.1111/j.1463-1326.2011.01545.x.
Lai SW, Chen PC, Liao KF, Muo CH, Lin CC, Sung FC. Risk of hepatocellular carcinoma in diabetic patients and risk reduction associated with anti-diabetic therapy: a population-based cohort study. Am J Gastroenterol. 2012;107:46–52. https://doi.org/10.1038/ajg.2011.384.
Liao KF, Lai SW, Li CI, Chen WC. Diabetes mellitus correlates with increased risk of pancreatic cancer: a population-based cohort study in Taiwan. J Gastroenterol Hepatol. 2012;27:709–13. https://doi.org/10.1111/j.1440-1746.2011.06938.x.
Monami M, Colombi C, Balzi D, Dicembrini I, Giannini S, Melani C, et al. Metformin and cancer occurrence in insulin-treated type 2 diabetic patients. Diabetes Care. 2011;34:129–31. https://doi.org/10.2337/dc10-1287.
Nakamura T, Matsuda T, Kawagoe Y, Ogawa H, Takahashi Y, Sekizuka K, et al. Effect of pioglitazone on carotid intima-media thickness and arterial stiffness in type 2 diabetic nephropathy patients. Metabolism. 2004;53:1382–6. https://doi.org/10.1016/j.metabol.2004.05.013.
Origasa H, Lee SH, Nakagawa H, Kumagai N, Fuse H, Tobe K. Pioglitazone use and bladder cancer — hospital-based results from a nested case-control study in Japan. Jpn Pharmacol Ther. 2013;41:663–7.
Pan C, Yang W, Barona JP, Wang Y, Niggli M, Mohideen P, et al. Comparison of vildagliptin and acarbose monotherapy in patients with type 2 diabetes: a 24-week, double-blind, randomized trial. Diabet Med. 2008;25:435–41. https://doi.org/10.1111/j.1464-5491.2008.02391.x.
Simo R, Plana-Ripoll O, Puente D, Morros R, Mundet X, Vilca LM, et al. Impact of glucose-lowering agents on the risk of cancer in type 2 diabetic patients The Barcelona case-control study. PLoS One. 2013;8:e79968. https://doi.org/10.1371/journal.pone.0079968.
Son JW, Lee IK, Woo JT, Baik SH, Jang HC, Lee KW, et al. A prospective, randomized, multicenter trial comparing the efficacy and safety of the concurrent use of long-acting insulin with mitiglinide or voglibose in patients with type 2 diabetes. Endocr J. 2015;62:1049–57. https://doi.org/10.1507/endocrj.EJ15-0325.
Tseng CH. Diabetes and risk of prostate cancer: a study using the National Health Insurance. Diabetes Care. 2011;34:616–21. https://doi.org/10.2337/dc10-1640.
Tseng CH. Diabetes and risk of bladder cancer: a study using the National Health Insurance database in Taiwan. Diabetologia. 2011;54:2009–15. https://doi.org/10.1007/s00125-011-2171-z.
Tseng CH. Thyroid cancer risk is not increased in diabetic patients. PLoS ONE. 2012;7:e53096. https://doi.org/10.1371/journal.pone.0053096.
Tseng CH. Use of metformin and risk of kidney cancer in patients with type 2 diabetes. Eur J Cancer. 2016;52:19–25. https://doi.org/10.1016/j.ejca.2015.09.027.
Yang X, So WY, Ma RC, Yu LW, Ko GT, Kong AP, et al. Use of sulphonylurea and cancer in type 2 diabetes—the Hong Kong Diabetes Registry. Diabetes Res Clin Pract. 2010;90:343–51. https://doi.org/10.1016/j.diabres.2010.08.022.
Coyle C, Cafferty FH, Vale C, Langley RE. Metformin as an adjuvant treatment for cancer: a systematic review and meta-analysis. Ann Oncol. 2016;27:2184–95. https://doi.org/10.1093/annonc/mdw410.
Daugan M, Dufay Wojcicki A, d’Hayer B, Boudy V. Metformin: an anti-diabetic drug to fight cancer. Pharmacol Res. 2016;113:675–85. https://doi.org/10.1016/j.phrs.2016.10.006.
Liu Y, Jin PP, Sun XC, Hu TT. Thiazolidinediones and risk of colorectal cancer in patients with diabetes mellitus: a meta-analysis. Saudi J Gastroenterol. 2018;24:75–81. https://doi.org/10.4103/sjg.SJG_295_17.
Bosetti C, Rosato V, Buniato D, Zambon A, La Vecchia C, Corrao G. Cancer risk for patients using thiazolidinediones for type 2 diabetes: a meta-analysis. Oncologist. 2013;18:148–56. https://doi.org/10.1634/theoncologist.2012-0302.
Mamtani R, Haynes K, Bilker WB, Vaughn DJ, Strom BL, Glanz K, et al. Association between longer therapy with thiazolidinediones and risk of bladder cancer: a cohort study. J Natl Cancer Inst. 2012;104:1411–21. https://doi.org/10.1093/jnci/djs328.
Nagamine M, Okumura T, Tanno S, Sawamukai M, Motomura W, Takahashi N, et al. PPAR gamma ligand-induced apoptosis through a p53-dependent mechanism in human gastric cancer cells. Cancer Sci. 2003;94:338–43. https://doi.org/10.1111/j.1349-7006.2003.tb01443.x.
Cellai I, Petrangolini G, Tortoreto M, Pratesi G, Luciani P, Deledda C, et al. In vivo effects of rosiglitazone in a human neuroblastoma xenograft. Br J Cancer. 2010;102:685–92. https://doi.org/10.1038/sj.bjc.6605506.
Luconi M, Mangoni M, Gelmini S, Poli G, Nesi G, Francalanci M, et al. Rosiglitazone impairs proliferation of human adrenocortical cancer: preclinical study in a xenograft mouse model. Endocr Relat Cancer. 2010;17:169–77. https://doi.org/10.1677/erc-09-0170.
Cao C, Yang S, Zhou Z. GLP-1 receptor agonists and risk of cancer in type 2 diabetes: an updated meta-analysis of randomized controlled trials. Endocrine. 2019;66:157–65. https://doi.org/10.1007/s12020-019-02055-z.
Bethel MA, Patel RA, Merrill P, Lokhnygina Y, Buse JB, Mentz RJ, et al. Cardiovascular outcomes with glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: a meta-analysis. Lancet Diabetes Endocrinol. 2018;6:105–13. https://doi.org/10.1016/s2213-8587(17)30412-6.
Monami M, Nreu B, Scatena A, Cresci B, Andreozzi F, Sesti G, et al. Safety issues with glucagon-like peptide-1 receptor agonists (pancreatitis, pancreatic cancer and cholelithiasis): data from randomized controlled trials. Diabetes Obes Metab. 2017;19:1233–41. https://doi.org/10.1111/dom.12926.
Piccoli GF, Mesquita LA, Stein C, Aziz M, Zoldan M, Degobi NAH, et al. Do GLP-1 receptor agonists increase the risk of breast cancer? A systematic review and meta-analysis. J Clin Endocrinol Metab. 2021;106:912–21. https://doi.org/10.1210/clinem/dgaa891 (A meta-analysis of 52 randomized controlled trials in patients with type 2 diabetes and/or obesity, who were treated with GLP-1 receptor agonists for at least 6 months. Results indicated that treatment did not increase the risk of breast neoplasms.).
Guo X, Yang Q, Dong J, Liao L, Zhang W, Liu F. Tumour risk with once-weekly glucagon-like peptide-1 receptor agonists in type 2 diabetes mellitus patients: a systematic review. Clin Drug Investig. 2016;36:433–41. https://doi.org/10.1007/s40261-016-0389-8.
Liu Y, Zhang X, Chai S, Zhao X, Ji L. Risk of malignant neoplasia with glucagon-like peptide-1 receptor agonist treatment in patients with type 2 diabetes: a meta-analysis. J Diabetes Res. 2019;2019:1534365. https://doi.org/10.1155/2019/1534365.
Shaefer CF Jr, Kushner P, Aguilar R. User’s guide to mechanism of action and clinical use of GLP-1 receptor agonists. Postgrad Med. 2015;127:818–26. https://doi.org/10.1080/00325481.2015.1090295.
Drucker DJ. Mechanisms of action and therapeutic application of glucagon-like peptide-1. Cell Metab. 2018;27:740–56. https://doi.org/10.1016/j.cmet.2018.03.001.
Bjerre Knudsen L, Madsen LW, Andersen S, Almholt K, de Boer AS, Drucker DJ, et al. Glucagon-like peptide-1 receptor agonists activate rodent thyroid C-cells causing calcitonin release and C-cell proliferation. Endocrinology. 2010;151:1473–86. https://doi.org/10.1210/en.2009-1272.
Smits MM, Van Raalte DH. Safety of semaglutide. Front Endocrinol. 2021;12:645563. https://doi.org/10.3389/fendo.2021.645563 (An overview of the safety aspects of the most popular and effective (at present) GLP-1 receoptor agonist, concluding there is overall low risk for severe adverse events, including pancreatic and thyroid cancers.).
Zhang X, Wang M, Wang X, Zhu Z, Zhang W, Zhou Z, et al. Comparison of new glucose-lowering drugs on the risk of pancreatitis in type 2 diabetes: a network meta-analysis. Endocr Pract. 2022;28:333–41. https://doi.org/10.1016/j.eprac.2021.12.007 (A meta-analysis of 17 studies with more than 100,000 patients with type 2 diabetes demonstrating that GLP-1 agonists and DPP-4 inhibitors do not increase the risk for pancreatic cancer.).
Zhang Z, Chen X, Lu P, Zhang J, Xu Y, He W, et al. Incretin-based agents in type 2 diabetic patients at cardiovascular risk: compare the effect of GLP-1 agonists and DPP-4 inhibitors on cardiovascular and pancreatic outcomes. Cardiovasc Diabetol. 2017;16:31. https://doi.org/10.1186/s12933-017-0512-z.
Abd El Aziz M, Cahyadi O, Meier JJ, Schmidt WE, Nauck MA. Incretin-based glucose-lowering medications and the risk of acute pancreatitis and malignancies: a meta-analysis based on cardiovascular outcomes trials. Diabetes Obes Metab. 2020;22:699–704. https://doi.org/10.1111/dom.13924 (A meta-analysis of 11 randomized, placebo-controlled, prospective cardiovascular outcomes studies with GLP-1 receptor agonists and DPP-4 inhibitors that found no increase in the risk for pancreatic cancer.).
Dicembrini I, Nreu B, Montereggi C, Mannucci E, Monami M. Risk of cancer in patients treated with dipeptidyl peptidase-4 inhibitors: an extensive meta-analysis of randomized controlled trials. Acta Diabetol. 2020;57:689–96. https://doi.org/10.1007/s00592-020-01479-8 (A meta-analysis of 157 placebo-controlled trials with more than 60,000 patients with type 2 diabetes per arm, demonstrating that use of DPP-4 inhibitors is not associated with the risk for overall cancer, and may in fact have beneficial effect on colorectal cancer risk (30% reduction).).
Thornberry NA, Gallwitz B. Mechanism of action of inhibitors of dipeptidyl-peptidase-4 (DPP-4). Best Pract Res Clin Endocrinol Metab. 2009;23:479–86. https://doi.org/10.1016/j.beem.2009.03.004.
Metzemaekers M, Van Damme J, Mortier A, Proost P. Regulation of chemokine activity — a focus on the role of dipeptidyl peptidase IV/CD26. Front Immunol. 2016;7:483. https://doi.org/10.3389/fimmu.2016.00483.
Yang F, Takagaki Y, Yoshitomi Y, Ikeda T, Li J, Kitada M, et al. Inhibition of dipeptidyl peptidase-4 accelerates epithelial-mesenchymal transition and breast cancer metastasis via the CXCL12/CXCR4/mTOR axis. Cancer Res. 2019;79:735–46. https://doi.org/10.1158/0008-5472.Can-18-0620.
Li S, Fan Y, Kumagai A, Kawakita E, Kitada M, Kanasaki K, et al. Deficiency in dipeptidyl peptidase-4 promotes chemoresistance through the CXCL12/CXCR4/mTOR/TGFβ signaling pathway in breast cancer cells. Int J Mol Sci. 2020;21:805. https://doi.org/10.3390/ijms21030805 (A cell culture and animal model study showing that DPP-4 inhibitors potentiate chemotherapy resistance via the induction of ABC transporters by the CXCL12/CXCR4/mTOR/TGFβ signaling pathway in breast cancer cells.).
Mortier A, Gouwy M, Van Damme J, Proost P, Struyf S. CD26/dipeptidylpeptidase IV-chemokine interactions: double-edged regulation of inflammation and tumor biology. J Leukoc Biol. 2016;99:955–69. https://doi.org/10.1189/jlb.3MR0915-401R.
Lin HW, Tseng CH. A review on the relationship between SGLT2 inhibitors and cancer. Int J Endocrinol. 2014;2014: 719578. https://doi.org/10.1155/2014/719578.
Burki TK. FDA rejects novel diabetes drug over safety fears. Lancet. 2012;379:507. https://doi.org/10.1016/s0140-6736(12)60216-5.
US Department of Health and Human Services. FDA briefing document — NDA 202293: dapagliflozin tablets, 5 and 10mg; 2011. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2014/202293Orig1s000ltr.pdf. Accessed 23 Nov 2022.
Tang H, Dai Q, Shi W, Zhai S, Song Y, Han J. SGLT2 inhibitors and risk of cancer in type 2 diabetes: a systematic review and meta-analysis of randomised controlled trials. Diabetologia. 2017;60:1862–72. https://doi.org/10.1007/s00125-017-4370-8.
Scafoglio C, Hirayama BA, Kepe V, Liu J, Ghezzi C, Satyamurthy N, et al. Functional expression of sodium-glucose transporters in cancer. Proc Natl Acad Sci U S A. 2015;112:E4111–9. https://doi.org/10.1073/pnas.1511698112.
Lutz SZ, Staiger H, Fritsche A, Haring HU. Antihyperglycaemic therapies and cancer risk. Diab Vasc Dis Res. 2014;11:371–89. https://doi.org/10.1177/1479164114549553.
Greco DS, Broussard JD, Peterson ME. Insulin therapy. Vet Clin North Am Small Anim Pract. 1995;25:677–89. https://doi.org/10.1016/s0195-5616(95)50062-2.
Haller MJ, Atkinson MA, Schatz D. Type 1 diabetes mellitus: etiology, presentation, and management. Pediatr Clin North Am. 2005;52:1553–78. https://doi.org/10.1016/j.pcl.2005.07.006.
Baron V, Van Obberghen E. Mechanism of insulin action. C R Seances Soc Biol Fil. 1995;189:25–41.
Home P. Insulin therapy and cancer. Diabetes Care. 2013;36(Suppl 2):S240–4. https://doi.org/10.2337/dcS13-2002.
Pollak M, Russell-Jones D. Insulin analogues and cancer risk: cause for concern or cause celebre? Int J Clin Pract. 2010;64:628–36. https://doi.org/10.1111/j.1742-1241.2010.02354.x.
Hernandez-Diaz S, Adami HO. Diabetes therapy and cancer risk: causal effects and other plausible explanations. Diabetologia. 2010;53:802–8. https://doi.org/10.1007/s00125-010-1675-2.
Pocock SJ, Smeeth L. Insulin glargine and malignancy: an unwarranted alarm. Lancet. 2009;374:511–3. https://doi.org/10.1016/S0140-6736(09)61307-6.
Renehan AG. Insulin analogues and cancer risk: the emergence of second-generation studies. Diabetologia. 2012;55:7–9. https://doi.org/10.1007/s00125-011-2352-9.
Suissa S, Azoulay L. Metformin and the risk of cancer: time-related biases in observational studies. Diabetes Care. 2012;35:2665–73. https://doi.org/10.2337/dc12-0788.
Dejgaard A, Lynggaard H, Rastam J, Krogsgaard TM. No evidence of increased risk of malignancies in patients with diabetes treated with insulin detemir: a meta-analysis. Diabetologia. 2009;52:2507–12. https://doi.org/10.1007/s00125-009-1568-4.
Investigators OT, Gerstein HC, Bosch J, Dagenais GR, Diaz R, Jung H, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012;367:319–28. https://doi.org/10.1056/NEJMoa1203858.
Carstensen B, Witte DR, Friis S. Cancer occurrence in Danish diabetic patients: duration and insulin effects. Diabetologia. 2012;55:948–58. https://doi.org/10.1007/s00125-011-2381-4.
Li D, Tang H, Hassan MM, Holly EA, Bracci PM, Silverman DT. Diabetes and risk of pancreatic cancer: a pooled analysis of three large case-control studies. Cancer Causes Control. 2011;22:189–97. https://doi.org/10.1007/s10552-010-9686-3.
Li D, Yeung SC, Hassan MM, Konopleva M, Abbruzzese JL. Antidiabetic therapies affect risk of pancreatic cancer. Gastroenterology. 2009;137:482–8. https://doi.org/10.1053/j.gastro.2009.04.013.
Mizuno S, Nakai Y, Isayama H, Yanai A, Takahara N, Miyabayashi K, et al. Risk factors and early signs of pancreatic cancer in diabetes: screening strategy based on diabetes onset age. J Gastroenterol. 2013;48:238–46. https://doi.org/10.1007/s00535-012-0622-z.
Thakkar B, Aronis KN, Vamvini MT, Shields K, Mantzoros CS. Metformin and sulfonylureas in relation to cancer risk in type II diabetes patients: a meta-analysis using primary data of published studies. Metabolism. 2013;62:922–34. https://doi.org/10.1016/j.metabol.2013.01.014.
Mekuria AN, Ayele Y, Tola A, Mishore KM. Monotherapy with metformin versus sulfonylureas and risk of cancer in type 2 diabetic patients: a systematic review and meta-analysis. J Diabetes Res. 2019;2019:7676909. https://doi.org/10.1155/2019/7676909.
Author information
Authors and Affiliations
Contributions
C.S.S. and P.N.E. were involved in study conceptualization, data extraction, analysis, methodology, visualization, and writing the original draft. M.D. was involved in reviewing and editing the manuscript. F.M. was involved in study conceptualization, data extraction, methodology, supervision, visualization, and writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors do not have any potential conflicts of interest to disclose.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Søndergaard, C.S., Esquivel, P.N., Dalamaga, M. et al. Use of Antihyperglycemic Drugs and Risk of Cancer in Patients with Diabetes. Curr Oncol Rep 25, 29–40 (2023). https://doi.org/10.1007/s11912-022-01344-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-022-01344-7