Abstract
Purpose of Review
Management of head and neck cancer (HNC) typically involves a morbid combination of surgery, radiation, and systemic therapy. As the number of HNC survivors grows, there is growing interest in rehabilitation strategies to manage HNC-related comorbidity. In this review, we summarize the current state of HNC rehabilitation research.
Recent Findings
We have organized our review using the World Health Organization’s International Classification of Function (ICF) model of impairment, activity, and participation. Specifically, we describe the current research on rehabilitation strategies to prevent and treat impairments including dysphagia, xerostomia, dysgeusia, dysosmia, odynophagia, trismus, first bite syndrome, dysarthria, dysphonia, lymphedema, shoulder syndrome, cervicalgia, cervical dystonia and dropped head syndrome, deconditioning, and fatigue. We also discuss the broader impact of HNC-related impairment by exploring the state of rehabilitation literature on activity, participation, psychosocial distress, and suicidality in HNC survivors.
Summary
We demonstrate that research in HNC rehabilitation continues to focus primarily on impairment-driven interventions. There remains a dearth of HNC rehabilitation studies directly examining the impact of rehabilitation interventions on outcomes related to activity and participation. More high-quality interventional studies and reviews are needed to guide prevention and treatment of functional loss in HNC survivors.



Similar content being viewed by others
References
Lydiatt WM, Patel SG, O’Sullivan B, et al. Head and neck cancers—major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67:122–137.
Cohen N, Fedewa S, Chen AY. Epidemiology and demographics of the head and neck cancer population. Oral Maxillofac Surg Clin North Am. 2018;30:381–95.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Pulte D, Brenner H. Changes in survival in head and neck cancers in the late 20th and early 21st century: a period analysis. Oncologist. 2010;15:994–1001.
Stubblefield MD. Neuromuscular complications of radiation therapy. Muscle Nerve. 2017;56:1031–40.
Stubblefield MD. Clinical evaluation and management of radiation fibrosis syndrome. Phys Med Rehabil Clin N Am. 2017;28:89–100.
Stubblefield MD. Radiation fibrosis syndrome: neuromuscular and musculoskeletal complications in cancer survivors. PM R. 2011;3:1041–54.
Stubblefield MD. Radiation fibrosis syndrome. In: Therapeutic uses of botulinum toxin. Edited by: Cooper G. Totowa, N.J.: Humana; 2007. pp. 19–38.
Rong X, Tang Y, Chen M, et al. Radiation-induced cranial neuropathy in patients with nasopharyngeal carcinoma. A follow-up study. Strahlentherapie und Onkologie : Organ der Deutschen Rontgengesellschaft ... [et al] 2012; 188:282–286.
Dong Y, Ridge JA, Ebersole B, et al. Incidence and outcomes of radiation-induced late cranial neuropathy in 10-year survivors of head and neck cancer. Oral Oncol. 2019;95:59–64.
Dong Y, Ridge JA, Li T, et al. Long-term toxicities in 10-year survivors of radiation treatment for head and neck cancer. Oral Oncol. 2017;71:122–8.
Cohen EE, LaMonte SJ, Erb NL, et al. American Cancer Society Head and Neck Cancer Survivorship Care Guideline. CA Cancer J Clin. 2016;66:203–39.
Gane EM, Michaleff ZA, Cottrell MA, et al. Prevalence, incidence, and risk factors for shoulder and neck dysfunction after neck dissection: a systematic review. Eur J Surg Oncol. 2017;43:1199–218.
Schmitz S, Machiels JP, Weynand B, et al. Results of selective neck dissection in the primary management of head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2009;266:437–43.
Silver JK, Baima J, Mayer RS. Impairment-driven cancer rehabilitation: an essential component of quality care and survivorship. CA Cancer J Clin. 2013;63:295–317.
Capozzi LC, Dolgoy ND, McNeely ML. Physical rehabilitation and occupational therapy. Oral Maxillofac Surg Clin North Am. 2018;30:471–86.
Jamal N, Ebersole B, Erman A, Chhetri D. Maximizing functional outcomes in head and neck cancer survivors: assessment and rehabilitation. Otolaryngol Clin North Am. 2017;50:837–52.
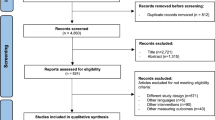
Parke SC, Oza S, Shahpar S, et al. Identifying gaps in research on rehabilitation for patients with head and neck cancer: a scoping review. Arch Phys Med Rehabil. 2019;100:2381–8.
Rauch A, Cieza A, Stucki G. How to apply the International Classification of Functioning, Disability and Health (ICF) for rehabilitation management in clinical practice. Eur J Phys Rehabil Med. 2008;44:329–42.
Crowder SL, Douglas KG, Yanina Pepino M, et al. Nutrition impact symptoms and associated outcomes in post-chemoradiotherapy head and neck cancer survivors: a systematic review. J Cancer Surviv. 2018;12:479–94.
Hutcheson KA, Nurgalieva Z, Zhao H, et al. Two-year prevalence of dysphagia and related outcomes in head and neck cancer survivors: an updated SEER-Medicare analysis. Head Neck. 2019;41:479–87.
Pezdirec M, Strojan P, Boltezar IH. Swallowing disorders after treatment for head and neck cancer. Radiol Oncol. 2019;53:225–30.
Jeans C, Ward EC, Brown B, et al. Association between external and internal lymphedema and chronic dysphagia following head and neck cancer treatment. Head Neck. 2021;43:255–67.
Loewen I, Jeffery CC, Rieger J, Constantinescu G. Prehabilitation in head and neck cancer patients: a literature review. J Otolaryngol Head Neck Surg. 2021;50:2.
Perry A, Lee SH, Cotton S, Kennedy C. Therapeutic exercises for affecting post‐treatment swallowing in people treated for advanced‐stage head and neck cancers. Cochrane Database of Systematic Reviews; 2016.
Greco E, Simic T, Ringash J, et al. Dysphagia treatment for patients with head and neck cancer undergoing radiation therapy: a meta-analysis review. Int J Radiat Oncol Biol Phys. 2018;101:421–44.
Banda KJ, Chu H, Kao CC, et al. Swallowing exercises for head and neck cancer patients: a systematic review and meta-analysis of randomized control trials. Int J Nurs Stud. 2021;114:103827.
Hsiang CC, Chen AW, Chen CH, Chen MK. Early postoperative oral exercise improves swallowing function among patients with oral cavity cancer: a randomized controlled trial. Ear Nose Throat J. 2019;98:E73-e80.
Govender R, Smith CH, Taylor SA, et al. Swallowing interventions for the treatment of dysphagia after head and neck cancer: a systematic review of behavioural strategies used to promote patient adherence to swallowing exercises. BMC Cancer. 2017;17:43.
Benfield JK, Everton LF, Bath PM, England TJ. Does therapy with biofeedback improve swallowing in adults with dysphagia? A systematic review and meta-analysis. Arch Phys Med Rehabil. 2019;100:551–61.
Alghadir AH, Zafar H, Al-Eisa ES, Iqbal ZA. Effect of posture on swallowing. Afr Health Sci. 2017;17:133–7.
Steele CM, Alsanei WA, Ayanikalath S, et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30:2–26.
Flynn E, Smith CH, Walsh CD, Walshe M. Modifying the consistency of food and fluids for swallowing difficulties in dementia. Cochrane Database Syst Rev. 2018;9:CD011077.
Gary JJ, Johnson AC, Garner FT. The role of the prosthodontist regarding aspirative dysphagia. J Prosthet Dent. 1992;67:101–6.
De Felice F, de Vincentiis M, Luzzi V, et al. Late radiation-associated dysphagia in head and neck cancer patients: evidence, research and management. Oral Oncol. 2018;77:125–30.
Pinna R, Campus G, Cumbo E, et al. Xerostomia induced by radiotherapy: an overview of the physiopathology, clinical evidence, and management of the oral damage. Ther Clin Risk Manag. 2015;11:171–88.
Strojan P, Hutcheson KA, Eisbruch A, et al. Treatment of late sequelae after radiotherapy for head and neck cancer. Cancer Treat Rev. 2017;59:79–92.
Chiu YH, Tseng WH, Ko JY, Wang TG. Radiation-induced swallowing dysfunction in patients with head and neck cancer: a literature review. J Formos Med Assoc. 2021.
Yang WF, Liao GQ, Hakim SG, et al. Is pilocarpine effective in preventing radiation-induced xerostomia? A systematic review and meta-analysis. Int J Radiat Oncol Biol Phys. 2016;94:503–11.
Jensen SB, Vissink A, Limesand KH, Reyland ME. Salivary gland hypofunction and xerostomia in head and neck radiation patients. J Natl Cancer Inst Monogr. 2019; 2019.
Riley P, Glenny AM, Hua F, Worthington HV. Pharmacological interventions for preventing dry mouth and salivary gland dysfunction following radiotherapy. Cochrane Database of Systematic Reviews. 2017.
Lee MG, Freeman AR, Roos DE, et al. Randomized double-blind trial of amifostine versus placebo for radiation-induced xerostomia in patients with head and neck cancer. J Med Imaging Radiat Oncol. 2019;63:142–50.
Bonomo P, Stocchi G, Caini S, et al. Acupuncture for radiation-induced toxicity in head and neck squamous cell carcinoma: a systematic review based on PICO criteria. Eur Arch Otorhinolaryngol. 2021.
Louzeiro GC, Teixeira DDS, Cherubini K, et al. Does laser photobiomodulation prevent hyposalivation in patients undergoing head and neck radiotherapy? A systematic review and meta-analysis of controlled trials. Crit Rev Oncol Hematol. 2020;156:103115.
Ma SJ, Rivers CI, Serra LM, Singh AK. Long-term outcomes of interventions for radiation-induced xerostomia: a review. World J Clin Oncol. 2019;10:1–13.
Mercadante V, Al Hamad A, Lodi G, et al. Interventions for the management of radiotherapy-induced xerostomia and hyposalivation: a systematic review and meta-analysis. Oral Oncol. 2017;66:64–74.
Johnstone PA, Peng YP, May BC, et al. Acupuncture for pilocarpine-resistant xerostomia following radiotherapy for head and neck malignancies. Int J Radiat Oncol Biol Phys. 2001;50:353–7.
Furness S, Bryan G, McMillan R, et al. Interventions for the management of dry mouth: non‐pharmacological interventions. Cochrane Database of Systematic Reviews 2013.
Ni X, Tian T, Chen D, et al. Acupuncture for radiation-induced xerostomia in cancer patients: a systematic review and meta-analysis. Integr Cancer Ther. 2020;19:1534735420980825.
Salimi F, Saavedra F, Andrews B, et al. Trans-cutaneous electrical nerve stimulation to treat dry mouth (xerostomia) following radiotherapy for head and neck cancer? A systematic review. Ann Med Surg (Lond). 2021;63:102146.
Iovoli AJ, Ostrowski A, Rivers CI, et al. Two- versus four-times weekly acupuncture-like transcutaneous electrical nerve stimulation for treatment of radiation-induced xerostomia: a pilot study. J Altern Complement Med. 2020;26:323–8.
Kaae JK, Stenfeldt L, Hyrup B, et al. A randomized phase III trial for alleviating radiation-induced xerostomia with chewing gum. Radiother Oncol. 2020;142:72–8.
Paterson C, Thomson MC, Caldwell B, et al. Radiotherapy-induced xerostomia: a randomised, double-blind, controlled trial of Visco-ease™ oral spray compared with placebo in patients with cancer of the head and neck. Br J Oral Maxillofac Surg. 2019;57:1119–25.
Apperley O, Medlicott N, Rich A, et al. A clinical trial of a novel emulsion for potential use as a saliva substitute in patients with radiation-induced xerostomia. J Oral Rehabil. 2017;44:889–95.
Lam-Ubol A, Matangkasombut O, Trachootham D, et al. Efficacy of gel-based artificial saliva on Candida colonization and saliva properties in xerostomic post-radiotherapy head and neck cancer patients: a randomized controlled trial. Clin Oral Investig. 2021;25:1815–27.
Nuchit S, Lam-Ubol A, Paemuang W, et al. Alleviation of dry mouth by saliva substitutes improved swallowing ability and clinical nutritional status of post-radiotherapy head and neck cancer patients: a randomized controlled trial. Support Care Cancer. 2020;28:2817–28.
Marimuthu D, Han KM, Mohamad MSF, Azman M. Saliva substitute mouthwash in nasopharyngeal cancer survivors with xerostomia: a randomized controlled trial. Clin Oral Investig. 2021;25:3105–15.
Marchand DK, McCormack S. CADTH rapid response reports. In: Pilocarpine for radiotherapy-induced dry mouth and dry eyes: a review of clinical effectiveness, cost-effectiveness, and guidelines. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health Copyright © 2020 Canadian Agency for Drugs and Technologies in Health; 2020.
Louzeiro GC, Cherubini K, de Figueiredo MAZ, Salum FG. Effect of photobiomodulation on salivary flow and composition, xerostomia and quality of life of patients during head and neck radiotherapy in short term follow-up: a randomized controlled clinical trial. J Photochem Photobiol B. 2020;209:111933.
Palma LF, Gonnelli FAS, Marcucci M, et al. Impact of low-level laser therapy on hyposalivation, salivary pH, and quality of life in head and neck cancer patients post-radiotherapy. Lasers Med Sci. 2017;32:827–32.
Ravi P, Vaishnavi D, Gnanam A, Krishnakumar Raja VB. The role of hyperbaric oxygen therapy in the prevention and management of radiation-induced complications of the head and neck – a systematic review of literature. J Stomatol Oral Maxillofac Surg. 2017;118:359–62.
Fox NF, Xiao C, Sood AJ, et al. Hyperbaric oxygen therapy for the treatment of radiation-induced xerostomia: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:22–8.
Heydarirad G, Rezaeizadeh H, Choopani R, et al. Efficacy of a traditional Persian medicine preparation for radiation-induced xerostomia: a randomized, open-label, active-controlled trial. J Integr Med. 2017;15:201–8.
Lim RJ, Nabil WNN, Chan SY, et al. Effects of herbal medicine for xerostomia in head and neck cancer patients: an observational study in a tertiary cancer hospital. Support Care Cancer. 2019;27:3491–8.
Nabil WNN, Lim RJ, Chan SY, et al. A systematic review on Chinese herbal treatment for radiotherapy-induced xerostomia in head and neck cancer patients. Complement Ther Clin Pract. 2018;30:6–13.
Charalambous A, Lambrinou E, Katodritis N, et al. The effectiveness of thyme honey for the management of treatment-induced xerostomia in head and neck cancer patients: a feasibility randomized control trial. Eur J Oncol Nurs. 2017;27:1–8.
Hoppe C, Kutschan S, Dörfler J, et al. Zinc as a complementary treatment for cancer patients: a systematic review. Clin Exp Med. 2021;21:297–313.
Gunn L, Gilbert J, Nenclares P, et al. Taste dysfunction following radiotherapy to the head and neck: a systematic review. Radiother Oncol. 2021;157:130–40.
Azzam P, Mroueh M, Francis M, et al. Radiation-induced neuropathies in head and neck cancer: prevention and treatment modalities. Ecancermedicalscience. 2020;14:1133.
Chen W-C, Tsai M-S, Tsai Y-T, et al. Long-term taste impairment after intensity-modulated radiotherapy to treat head-and-neck cancer: correlations with glossectomy and the mean radiation dose to the oral cavity. Chem Senses. 2019;44:319–26.
Epstein JB, Villines D, Epstein GL, Smutzer G. Oral examination findings, taste and smell testing during and following head and neck cancer therapy. Support Care Cancer. 2020;28:4305–11.
Alfaro R, Crowder S, Sarma KP, et al. Taste and smell function in head and neck cancer survivors. Chem Senses. 2021;46.
Sevryugin O, Kasvis P, Vigano M, Vigano A. Taste and smell disturbances in cancer patients: a scoping review of available treatments. Support Care Cancer. 2021;29:49–66.
Longobardi Y, Parrilla C, Di Cintio G, et al. Olfactory perception rehabilitation after total laryngectomy (OPRAT): proposal of a new protocol based on training of sensory perception skills. Eur Arch Otorhinolaryngol. 2020;277:2095–105.
Elting LS, Keefe DM, Sonis ST, et al. Patient-reported measurements of oral mucositis in head and neck cancer patients treated with radiotherapy with or without chemotherapy: demonstration of increased frequency, severity, resistance to palliation, and impact on quality of life. Cancer. 2008;113:2704–13.
Riley P, Glenny AM, Worthington HV, et al. Interventions for preventing oral mucositis in patients with cancer receiving treatment: cytokines and growth factors. Cochrane Database Syst Rev. 2017;11:CD011990.
Campos TM, do Prado Tavares Silva CA, Sobral APT, et al. Photobiomodulation in oral mucositis in patients with head and neck cancer: a systematic review and meta-analysis followed by a cost-effectiveness analysis. Support Care Cancer. 2020;28:5649–59.
de Lima VHS, de Oliveira-Neto OB, da Hora Sales PH, et al. Effectiveness of low-level laser therapy for oral mucositis prevention in patients undergoing chemoradiotherapy for the treatment of head and neck cancer: a systematic review and meta-analysis. Oral Oncol. 2020;102:104524.
Mallick S, Benson R, Rath GK. Radiation induced oral mucositis: a review of current literature on prevention and management. Eur Arch Otorhinolaryngol. 2016;273:2285–93.
An W, Li S, Qin L. Role of honey in preventing radiation-induced oral mucositis: a meta-analysis of randomized controlled trials. Food Funct. 2021;12:3352–65.
Liu TM, Luo YW, Tam KW, et al. Prophylactic and therapeutic effects of honey on radiochemotherapy-induced mucositis: a meta-analysis of randomized controlled trials. Support Care Cancer. 2019;27:2361–70.
Zhang L, Tang G, Wei Z. Prophylactic and therapeutic effects of curcumin on treatment-induced oral mucositis in patients with head and neck cancer: a meta-analysis of randomized controlled trials. Nutr Cancer. 2021;73:740–9.
Alsubaie HM, Alsini AY, Alsubaie KM, et al. Glutamine for prevention and alleviation of radiation-induced oral mucositis in patients with head and neck squamous cell cancer: systematic review and meta-analysis of controlled trials. Head Neck. 2021;43:3199–213.
Saunders DP, Rouleau T, Cheng K, et al. Systematic review of antimicrobials, mucosal coating agents, anesthetics, and analgesics for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. 2020;28:2473–84.
Judge LF, Farrugia MK, Singh AK. Narrative review of the management of oral mucositis during chemoradiation for head and neck cancer. Ann Transl Med. 2021;9:916.
Roldan CJ, Chung M, Feng L, Bruera E. Methylene blue for the treatment of intractable pain from oral mucositis related to cancer treatment: an uncontrolled cohort. J Natl Compr Canc Netw. 2021;19:521–7.
Chen SC. Oral dysfunction in patients with head and neck cancer: a systematic review. J Nurs Res. 2019;27:e58.
Dijkstra PU, Huisman PM, Roodenburg JL. Criteria for trismus in head and neck oncology. Int J Oral Maxillofac Surg. 2006;35:337–42.
van der Geer SJ, van Rijn PV, Roodenburg JLN, Dijkstra PU. Prognostic factors associated with a restricted mouth opening (trismus) in patients with head and neck cancer: systematic review. Head Neck. 2020;42:2696–721.
Hajdú SF, Wessel I, Johansen C, et al. Swallowing therapy and progressive resistance training in head and neck cancer patients undergoing radiotherapy treatment: randomized control trial protocol and preliminary data. Acta Oncol. 2017;56:354–9.
Kamstra JI, van Leeuwen M, Roodenburg JLN, Dijkstra PU. Exercise therapy for trismus secondary to head and neck cancer: a systematic review. Head Neck. 2017;39:2352–62.
Sandler ML, Lazarus CL, Ru M, et al. Effects of jaw exercise intervention timing on outcomes following oral and oropharyngeal cancer surgery: pilot study. Head Neck. 2019;41:3806–17.
Shao CH, Chiang CC, Huang TW. Exercise therapy for cancer treatment-induced trismus in patients with head and neck cancer: a systematic review and meta-analysis of randomized controlled trials. Radiother Oncol. 2020;151:249–55.
Zatarain LA, Smith DK, Deng J, et al. A randomized feasibility trial to evaluate use of the jaw dynasplint to prevent trismus in patients with head and neck cancer receiving primary or adjuvant radiation-based therapy. Integr Cancer Ther. 2018;17:960–7.
Du T, Xiao J, Qiu Z, Wu K. The effectiveness of intensity-modulated radiation therapy versus 2D-RT for the treatment of nasopharyngeal carcinoma: a systematic review and meta-analysis. PloS One. 2019;14:e0219611.
Chen D, Chen X, Chen X, et al. The efficacy of positioning stents in preventing oral complications after head and neck radiotherapy: a systematic literature review. Radiat Oncol. 2020;15:90.
Nayar S, Greer A, Mosaku A, Vere J. The use of intraoral devices in reducing oral and dental side effects in head and neck cancer patients undergoing radiotherapy - a systematic review. Int J Prosthodont. 2021.
Brandão TB, da Graça Pinto H, Vechiato Filho AJ et al. Are intraoral stents effective in reducing oral toxicities caused by radiotherapy? A systematic review and meta-analysis. J Prosthet Dent. 2021.
Alves LDB, Menezes ACS, Pereira DL, et al. Benefits of intraoral stents in patients with head and neck cancer undergoing radiotherapy: systematic review. Head Neck. 2021;43:1652–63.
Hague C, Beasley W, Garcez K, et al. Prospective evaluation of relationships between radiotherapy dose to masticatory apparatus and trismus. Acta Oncol. 2018;57:1038–42.
Nichols AC, Theurer J, Prisman E, et al. Radiotherapy versus transoral robotic surgery and neck dissection for oropharyngeal squamous cell carcinoma (ORATOR): an open-label, phase 2, randomised trial. Lancet Oncol. 2019;20:1349–59.
Chee S, Byrnes YM, Chorath KT, et al. Interventions for trismus in head and neck cancer patients: a systematic review of randomized controlled trials. Integr Cancer Ther. 2021;20:15347354211006474.
Wang TJ, Su JH, Leung KW, et al. Effects of a mouth-opening intervention with remote support on adherence, the maximum interincisal opening, and mandibular function of postoperative oral cancer patients: a randomized clinical trial. Eur J Oncol Nurs. 2019;40:111–9.
Li YH, Chang WC, Chiang TE, et al. Mouth-opening device as a treatment modality in trismus patients with head and neck cancer and oral submucous fibrosis: a prospective study. Clin Oral Investig. 2019;23:469–76.
van der Geer SJ, Reintsema H, Kamstra JI, et al. The use of stretching devices for treatment of trismus in head and neck cancer patients: a randomized controlled trial. Support Care Cancer. 2020;28:9–11.
Lee R, Yeo ST, Rogers SN, et al. Randomised feasibility study to compare the use of Therabite® with wooden spatulas to relieve and prevent trismus in patients with cancer of the head and neck. Br J Oral Maxillofac Surg. 2018;56:283–91.
Stubblefield MD, Manfield L, Riedel ER. A preliminary report on the efficacy of a dynamic jaw opening device (Dynasplint Trismus System) as part of the multimodal treatment of trismus in patients with head and neck cancer. Arch Phys Med Rehabil. 2010;91:1278–82.
Laccourreye O, Werner A, Garcia D, et al. First bite syndrome. Eur Ann Otorhinolaryngol Head Neck Dis. 2013;130:269–73.
Steel SJ, Robertson CE. First bite syndrome: what neurologists need to know. Curr Pain Headache Rep. 2021;25:31.
Sims JR, Suen JY. First bite syndrome: case report of 3 patients treated with botulinum toxin and review of other treatment modalities. Head Neck. 2013;35:E288-291.
Cohen SM, Elackattu A, Noordzij JP, et al. Palliative treatment of dysphonia and dysarthria. Otolaryngol Clin North Am. 2009;42(107–121):x.
Jacobi I, van Rossum MA, van der Molen L, et al. Acoustic analysis of changes in articulation proficiency in patients with advanced head and neck cancer treated with chemoradiotherapy. Ann Otol Rhinol Laryngol. 2013;122:754–62.
Okada N, Sasaguri K, Otsuka T, et al. Effect of articulatory rehabilitation after oral cancer surgery on higher brain activation. Int J Oral Maxillofac Surg. 2014;43:933–40.
Zebralla V, Wichmann G, Pirlich M, et al. Dysphagia, voice problems, and pain in head and neck cancer patients. Eur Arch Otorhinolaryngol. 2021:1–10.
Rosa MEd, Mituuti CT, Ghirardi ACdAM. Correlation between the voice handicap and swallowing quality of life in patients with laryngeal cancer submitted to chemoradiotherapy. In: CoDAS. SciELO Brasil; 2018.
Arenaz Búa B, Pendleton H, Westin U, Rydell R. Voice and swallowing after total laryngectomy. Acta Otolaryngol. 2018;138:170–4.
Jacobi I, Navran A, van der Molen L, et al. Radiation dose to the tongue and velopharynx predicts acoustic-articulatory changes after chemo-IMRT treatment for advanced head and neck cancer. Eur Arch Otorhinolaryngol. 2016;273:487–94.
Stachler RJ, Francis DO, Schwartz SR, et al. Clinical practice guideline: hoarseness (dysphonia) (update). Otolaryngology-Head Neck Surg. 2018;158:S1–42.
van der Molen L, van Rossum MA, Jacobi I, et al. Pre- and posttreatment voice and speech outcomes in patients with advanced head and neck cancer treated with chemoradiotherapy: expert listeners’ and patient’s perception. J Voice. 2012;26(664):e625-633.
Kraaijenga S, Oskam I, Van Son R, et al. Assessment of voice, speech, and related quality of life in advanced head and neck cancer patients 10-years+ after chemoradiotherapy. Oral Oncol. 2016;55:24–30.
Chen SC, Yu PJ, Hong MY, et al. Communication dysfunction, body image, and symptom severity in postoperative head and neck cancer patients: factors associated with the amount of speaking after treatment. Support Care Cancer. 2015;23:2375–82.
Bridhikitti J, Chotigavanich C, Apiwarodom N. Voice outcomes after radiotherapy for laryngeal cancer. Asian J Oncol. 2021;7:096–104.
Naunheim MR, Garneau J, Park C, et al. Voice outcomes after radiation for early-stage laryngeal cancer. J Voice. 2020;34:460–4.
Ryu CH, Kwon TK, Kim H, et al. Guidelines for the management of unilateral vocal fold paralysis from the Korean Society of Laryngology, Phoniatrics and Logopedics. Clin Exp Otorhinolaryngol. 2020;13:340–60.
Taito M, Taito S, Banno M, et al. Voice rehabilitation for laryngeal cancer after radiotherapy: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol. 2019;276:1573–83.
Karlsson T, Tuomi L, Andréll P, et al. Effects of voice rehabilitation after radiotherapy for laryngeal cancer: a longitudinal study. Logoped Phoniatr Vocol. 2017;42:167–77.
Millgård M, Tuomi L. Voice quality in laryngeal cancer patients: a randomized controlled study of the effect of voice rehabilitation. J Voice. 2020;34:486.e413-486.e422.
Angadi V, Dressler E, Kudrimoti M, et al. Efficacy of voice therapy in improving vocal function in adults irradiated for laryngeal cancers: a pilot study. J Voice. 2020;34:962.e969-962.e918.
Şahin M, Ogut MF, Vardar R, et al. Novel esophageal speech therapy method in total laryngectomized patients: biofeedback by intraesophageal impedance. Dis Esophagus. 2016;29:41–7.
van Sluis KE, van der Molen L, van Son R, et al. Objective and subjective voice outcomes after total laryngectomy: a systematic review. Eur Arch Otorhinolaryngol. 2018;275:11–26.
Johansson M, Finizia C, Persson J, Tuomi L. Cost-effectiveness analysis of voice rehabilitation for patients with laryngeal cancer: a randomized controlled study. Support Care Cancer. 2020;28:5203.
Cucchi F, Rossmeislova L, Simonsen L, et al. A vicious circle in chronic lymphoedema pathophysiology? An adipocentric view. Obes Rev. 2017;18:1159–69.
Ridner SH, Dietrich MS, Niermann K, et al. A prospective study of the lymphedema and fibrosis continuum in patients with head and neck cancer. Lymphat Res Biol. 2016;14:198–205.
Deng J, Murphy BA, Dietrich MS, et al. Impact of secondary lymphedema after head and neck cancer treatment on symptoms, functional status, and quality of life. Head Neck. 2013;35:1026–35.
Jeans C, Ward EC, Cartmill B, et al. Patient perceptions of living with head and neck lymphoedema and the impacts to swallowing, voice and speech function. Eur J Cancer Care (Engl). 2019;28:e12894.
Deng J, Ridner SH, Dietrich MS, et al. Prevalence of secondary lymphedema in patients with head and neck cancer. J Pain Symptom Manage. 2012;43:244–52.
Deng J, Ridner SH, Murphy BA. Lymphedema in patients with head and neck cancer. Oncol Nurs Forum. 2011;38:E1–10.
Deng J, Ridner SH, Aulino JM, Murphy BA. Assessment and measurement of head and neck lymphedema: state-of-the-science and future directions. Oral Oncol. 2015;51:431–7.
Aulino JM, Wulff-Burchfield EM, Dietrich MS, et al. Evaluation of CT changes in the head and neck after cancer treatment: development of a measurement tool. Lymphat Res Biol. 2018;16:69–74.
Deng J, Dietrich MS, Niermann KJ, et al. Refinement and validation of the head and neck lymphedema and fibrosis symptom inventory. Int J Radiat Oncol Biol Phys. 2021;109:747–55.
Ridner SH, Dietrich MS, Deng J, et al. Advanced pneumatic compression for treatment of lymphedema of the head and neck: a randomized wait-list controlled trial. Support Care Cancer. 2021;29:795–803.
Starmer HM, Drinnan M, Bhabra M, et al. Development and reliability of the revised Patterson Edema Scale. Clin Otolaryngol. 2021;46:752–7.
Tyker A, Franco J, Massa ST, et al. Treatment for lymphedema following head and neck cancer therapy: a systematic review. Am J Otolaryngol. 2019;40:761–9.
Smith BG, Hutcheson KA, Little LG, et al. Lymphedema outcomes in patients with head and neck cancer. Otolaryngol Head Neck Surg. 2015;152:284–91.
Doke KN, Bowman L, Shnayder Y, et al. Quantitative clinical outcomes of therapy for head and neck lymphedema. Adv Radiat Oncol. 2018;3:366–71.
Tacani PM, Franceschini JP, Tacani RE, et al. Retrospective study of the physical therapy modalities applied in head and neck l ymphedema treatment. Head Neck. 2016;38:301–8.
Krisciunas GP, Golan H, Marinko LN, et al. A novel manual therapy programme during radiation therapy for head and neck cancer – our clinical experience with five patients. Clin Otolaryngol. 2016;41:425–31.
Nixon JL, Pigott AE, Cartmill B, et al. A mixed methods examination of distress and person-centred experience of head and neck lymphoedema. Oral Oncol. 2018;83:18–24.
Pigott A, Nixon J, Fleming J, Porceddu S. Head and neck lymphedema management: evaluation of a therapy program. Head Neck. 2018;40:1131–7.
Ozdemir K, Keser I, Duzlu M, et al. The effects of clinical and home-based physiotherapy programs in secondary head and neck lymphedema. Laryngoscope. 2021;131:E1550-e1557.
Gutierrez C, Karni RJ, Naqvi S, et al. Head and neck lymphedema: treatment response to single and multiple sessions of advanced pneumatic compression therapy. Otolaryngol Head Neck Surg. 2019;160:622–6.
Gutiérrez C, Mayrovitz HN, Naqvi SHS, Karni RJ. Longitudinal effects of a novel advanced pneumatic compression device on patient-reported outcomes in the management of cancer-related head and neck lymphedema: a preliminary report. Head Neck. 2020;42:1791–9.
Tritter AG, Spiller PT, Brown ML et al. Pilot study: pneumatic compression garment therapy for postradiotherapy laryngopharyngeal edema. Ear Nose Throat J 2020:145561320942362.
Carvalho APV, Vital FMR, Soares BGO. Exercise interventions for shoulder dysfunction in patients treated for head and neck cancer. Cochrane Database of Systematic Reviews 2012.
Bradley PJ, Ferlito A, Silver CE, et al. Neck treatment and shoulder morbidity: still a challenge. Head Neck. 2011;33:1060–7.
Almeida KAM, Rocha AP, Carvas N, Pinto A. Rehabilitation interventions for shoulder dysfunction in patients with head and neck cancer: systematic review and meta-analysis. Phys Ther. 2020;100:1997–2008.
Dijkstra PU, van Wilgen PC, Buijs RP, et al. Incidence of shoulder pain after neck dissection: a clinical explorative study for risk factors. Head Neck. 2001;23:947–53.
Dziegielewski PT, McNeely ML, Ashworth N, et al. 2b or not 2b? Shoulder function after level 2b neck dissection: a double-blind randomized controlled clinical trial. Cancer. 2020;126:1492–501.
Baima J, Reynolds S-G, Edmiston K, et al. Teaching of independent exercises for prehabilitation in breast cancer. J Cancer Educ. 2017;32:252–6.
Yang A, Sokolof J, Gulati A. The effect of preoperative exercise on upper extremity recovery following breast cancer surgery: a systematic review. Int J Rehabil Res. 2018;41:189–96.
Barber B, Seikaly H, Ming Chan K, et al. Intraoperative brief electrical stimulation of the spinal accessory nerve (BEST SPIN) for prevention of shoulder dysfunction after oncologic neck dissection: a double-blinded, randomized controlled trial. J Otolaryngol Head Neck Surg. 2018;47:7–7.
Chen YH, Lin CR, Liang WA, Huang CY. Motor control integrated into muscle strengthening exercises has more effects on scapular muscle activities and joint range of motion before initiation of radiotherapy in oral cancer survivors with neck dissection: a randomized controlled trial. PLoS One. 2020;15:e0237133.
Conboy VB, Morris RW, Kiss J, Carr AJ. An evaluation of the Constant-Murley shoulder assessment. J Bone Jt Surg Br. 1996;78-B:229–32.
Chatterjee M, Murthy V, Gupta T, et al. Effect of progressive resistive exercises on shoulder abduction range of motion in post operative oral cancer patients undergoing radiation therapy. Physiotherapy. 2015;101:e216–7.
McGarvey AC, Hoffman GR, Osmotherly PG, Chiarelli PE. Maximizing shoulder function after accessory nerve injury and neck dissection surgery: a multicenter randomized controlled trial. Head Neck. 2015;37:1022–31.
McNeely ML, Parliament M, Courneya KS, et al. A pilot study of a randomized controlled trial to evaluate the effects of progressive resistance exercise training on shoulder dysfunction caused by spinal accessory neurapraxia/neurectomy in head and neck cancer survivors. Head Neck. 2004;26:518–30.
McNeely ML, Parliament MB, Seikaly H, et al. Effect of exercise on upper extremity pain and dysfunction in head and neck cancer survivors: a randomized controlled trial. Cancer. 2008;113:214–22.
Do JH, Yoon IJ, Cho YK, et al. Comparison of hospital based and home based exercise on quality of life, and neck and shoulder function in patients with spinal accessary nerve injury after head and neck cancer surgery. Oral Oncol. 2018;86:100–4.
Su T-L, Chen A-N, Leong C-P, et al. The effect of home-based program and outpatient physical therapy in patients with head and neck cancer: a randomized, controlled trial. Oral Oncol. 2017;74:130–4.
Kline-Quiroz C, Nori P, Stubblefield MD. Cancer rehabilitation: acute and chronic issues, nerve injury, radiation sequelae, surgical and chemo-related, part 1. Med Clin North Am. 2020;104:239–50.
van Wilgen CP, Dijkstra PU, van der Laan BF, et al. Morbidity of the neck after head and neck cancer therapy. Head Neck. 2004;26:785–91.
Nilsen ML, Lyu L, Belsky MA, et al. Impact of neck disability on health-related quality of life among head and neck cancer survivors. Otolaryngol Head Neck Surg. 2020;162:64–72.
Bossi P, Di Pede P, Guglielmo M, et al. Prevalence of fatigue in head and neck cancer survivors. Ann Otol Rhinol Laryngol. 2019;128:413–9.
Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;11:Cd006145.
Sagaonkar PS, Pattanshetty R. Effect of medical qigong therapy on distress, fatigue, and quality of life in head and neck cancer patients undergoing intensity-modulated radiation therapy: a single arm clinical trial. 2021.
Wang H-L, McMillan SC, Vijayakumar N, et al. A behavioral physical activity intervention to manage moderate and severe fatigue among head and neck cancer patients—pre-efficacy study in the National Institutes of Health ORBIT model. Cancer Nurs. 2019;42:E1–14.
Lavigne C, Twomey R, Lau H, et al. Feasibility of eccentric overloading and neuromuscular electrical stimulation to improve muscle strength and muscle mass after treatment for head and neck cancer. J Cancer Surviv. 2020;14:790–805.
Sun X, Chen Y, Cheung WK, et al. Pharmacological interventions for the management of cancer-related fatigue among cancer survivors: systematic review and meta-analysis. Integr Cancer Ther. 2021;20:15347354211038008.
Ramasamy V, Binti Mat Lazim N, Abdullah B, Singh A. Effects of Tualang honey on cancer related fatigue: a multicenter open-label trial of H&N cancer patients. Gulf J Oncol. 2019;1:43–51.
Guglielmo M, Di Pede P, Alfieri S, et al. A randomized, double-blind, placebo controlled, phase II study to evaluate the efficacy of ginseng in reducing fatigue in patients treated for head and neck cancer. J Cancer Res Clin Oncol. 2020;146:2479–87.
Martins SPdS, Ferreira CL, Del Giglio A. Placebo-controlled, double-blind, randomized study of a dry guarana extract in patients with head and neck tumors undergoing chemoradiotherapy: effects on fatigue and quality of life. J Diet Suppl. 2017;14:32–41.
Buffart LM, Kalter J, Sweegers MG, et al. Effects and moderators of exercise on quality of life and physical function in patients with cancer: an individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev. 2017;52:91–104.
Yen CJ, Hung CH, Kao CL, et al. Multimodal exercise ameliorates exercise responses and body composition in head and neck cancer patients receiving chemotherapy. Support Care Cancer. 2019;27:4687–95.
Lin KY, Cheng HC, Yen CJ, et al. Effects of exercise in patients undergoing chemotherapy for head and neck cancer: a pilot randomized controlled trial. Int J Environ Res Public Health 2021; 18.
Lynch PT, Horani S, Lee R, et al. Effectiveness of physical activity interventions in improving objective and patient-reported outcomes in head and neck cancer survivors: a systematic review. Oral Oncol. 2021;117:105253.
Bye A, Sandmael JA, Stene GB, et al. Exercise and nutrition interventions in patients with head and neck cancer during curative treatment: a systematic review and meta-analysis. Nutrients. 2020;12.
Nekhlyudov L, Lacchetti C, Davis NB, et al. Head and Neck Cancer Survivorship Care Guideline: American Society of Clinical Oncology Clinical Practice Guideline Endorsement of the American Cancer Society Guideline. J Clin Oncol. 2017;35:1606–21.
Nguyen NA, Ringash J. Head and neck cancer survivorship care: a review of the current guidelines and remaining unmet needs. Curr Treat Options Oncol. 2018;19:44.
Jiang W, Ding H, Li W, et al. Benefits of oral nutritional supplements in patients with locally advanced nasopharyngeal cancer during concurrent chemoradiotherapy: an exploratory prospective randomized trial. Nutr Cancer. 2018;70:1299–307.
de Carvalho CS, Silva TH, André JCS, et al. Preoperative fasting abbreviation with whey protein reduces the occurrence of postoperative complications in patients with head and neck cancer: a randomized clinical trial. Nutr Clin Pract. 2021;36:665–72.
Zahn KL, Wong G, Bedrick EJ, et al. Relationship of protein and calorie intake to the severity of oral mucositis in patients with head and neck cancer receiving radiation therapy. Head Neck. 2012;34:655–62.
Cereda E, Cappello S, Colombo S, et al. Nutritional counseling with or without systematic use of oral nutritional supplements in head and neck cancer patients undergoing radiotherapy. Radiother Oncol. 2018;126:81–8.
Cereda E, Turri A, Klersy C, et al. Whey protein isolate supplementation improves body composition, muscle strength, and treatment tolerance in malnourished advanced cancer patients undergoing chemotherapy. Cancer Med. 2019;8:6923–32.
Hutcheson KA, Bhayani MK, Beadle BM, et al. Eat and exercise during radiotherapy or chemoradiotherapy for pharyngeal cancers: use it or lose it. JAMA Otolaryngol Head Neck Surg. 2013;139:1127–34.
Samuel SR, Maiya AG, Fernandes DJ, et al. Effectiveness of exercise-based rehabilitation on functional capacity and quality of life in head and neck cancer patients receiving chemo-radiotherapy. Support Care Cancer. 2019;27:3913–20.
Dunne S, Mooney O, Coffey L, et al. Psychological variables associated with quality of life following primary treatment for head and neck cancer: a systematic review of the literature from 2004 to 2015. Psychooncology. 2017;26:149–60.
Davidson A, Williams J. Factors affecting quality of life in patients experiencing facial disfigurement due to surgery for head and neck cancer. Br J Nurs. 2019;28:180–4.
Castellano A, Sharma A. Systematic review of validated quality of life and swallow outcomes after transoral robotic surgery. Otolaryngol Head Neck Surg. 2019;161:561–7.
Wulff NB, Dalton SO, Wessel I, et al. Health-related quality of life, dysphagia, voice problems, depression, and anxiety after total laryngectomy. Laryngoscope. 2021.
Bressan V, Bagnasco A, Aleo G, et al. The life experience of nutrition impact symptoms during treatment for head and neck cancer patients: a systematic review and meta-synthesis. Support Care Cancer. 2017;25:1699–712.
Qualizza M, Bressan V, Rizzuto A, et al. Listening to the voice of patients with head and neck cancer: a systematic review and meta-synthesis. Eur J Cancer Care (Engl). 2019;28:e12939.
Manier KK, Rowe LS, Welsh J, Armstrong TS. The impact and incidence of altered body image in patients with head and neck tumors: a systematic review. Neurooncol Pract. 2018;5:204–13.
Hazzard E, Gulliver S, Walton K, et al. The patient experience of having a feeding tube during treatment for head and neck cancer: a systematic literature review. Clin Nutr ESPEN. 2019;33:66–85.
Morris N, Moghaddam N, Tickle A, Biswas S. The relationship between coping style and psychological distress in people with head and neck cancer: a systematic review. Psychooncology. 2018;27:734–47.
Osazuwa-Peters N, Adjei Boakye E, Walker RJ, Varvares MA. Suicide: a major threat to head and neck cancer survivorship. J Clin Oncol. 2016;34:1151.
Osazuwa-Peters N, Arnold LD, Loux TM, et al. Factors associated with increased risk of suicide among survivors of head and neck cancer: a population-based analysis. Oral Oncol. 2018;81:29–34.
Osazuwa-Peters N, Barnes JM, Okafor SI et al. Incidence and risk of suicide among patients with head and neck cancer in rural, urban, and metropolitan areas. JAMA Otolaryngol Head Neck Surg. 2021.
Osazuwa-Peters N, Simpson MC, Zhao L, et al. Suicide risk among cancer survivors: head and neck versus other cancers. Cancer. 2018;124:4072–9.
Kam D, Salib A, Gorgy G, et al. Incidence of suicide in patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg. 2015;141:1075–81.
Twigg JA, Anderson JM, Humphris G, et al. Best practice in reducing the suicide risk in head and neck cancer patients: a structured review. Br J Oral Maxillofac Surg. 2020;58:e6–15.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sara Parke declares that she has no conflict of interest. David Langelier declares that he has no conflict of interest. Jessica Tse Cheng declares that she has no conflict of interest. Cristina Kline-Quiroz declares that she has no conflict of interest. Michael Dean Stubblefield has received compensation for service as a consultant from Tactile Medical.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cancer Rehabilitation
Rights and permissions
About this article
Cite this article
Parke, S.C., Langelier, D.M., Cheng, J.T. et al. State of Rehabilitation Research in the Head and Neck Cancer Population: Functional Impact vs. Impairment-Focused Outcomes. Curr Oncol Rep 24, 517–532 (2022). https://doi.org/10.1007/s11912-022-01227-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-022-01227-x