Abstract
Purpose of Review
Melanoma has one of the highest incidences of causing leptomeningeal disease (LMD) among solid tumors. LMD patients have very poor prognosis with a dismal survival despite aggressive management. In this article, we review the current approaches in the management of patients with LMD secondary to melanoma, including updates in diagnosis, treatment, up-to-date clinical studies, and future directions.
Recent Findings
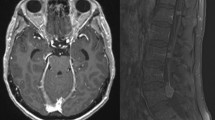
Cerebrospinal fluid (CSF) cytology remains the gold standard for diagnosis, and alternatively, MRI based on clinical presentation can be used. Other approaches such as “liquid biopsies” that detect circulating tumor cells and cell-free DNA have the potential to considerably enhance the diagnosis of LMD from melanoma. As for treatment options, several systemic therapies, involving systemic targeted and immunotherapies have evolved that showed to have possible benefit in LMD patients. Intrathecal chemotherapy, cellular therapy, and immunotherapy are currently under evaluation in Phase I/II clinical trials. In addition, new radiation therapy approaches such as proton cranial-spinal irradiation (CSI) are currently under investigation.
Summary
LMD management still remains challenging. Future studies are critical to elucidate the pathophysiology of LMD in order to develop new urgently needed diagnostic tools and therapies. Clinical trials ought to be expanded to include patients with LMD. Future clinical studies should also integrate tissue interrogation, scientifically designed therapies, and aggressive, early intervention in patients with suspected LMD.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Cohen JV, Tawbi H, Margolin KA, et al. Melanoma central nervous system metastases: current approaches, challenges, and opportunities. Pigment Cell Melanoma Res. 2016;29(6):627–42.
Leal T, Chang JE, Mehta M, Robins HI. Leptomeningeal metastasis: challenges in diagnosis and treatment. Curr Cancer Ther Rev. 2011;7(4):319–27.
Glitza IC, Smalley KSM, Brastianos PK, et al. Leptomeningeal disease in melanoma patients: an update to treatment, challenges, and future directions. Pigment Cell Melanoma Res. 2020;33(4):527–41.
Davies MA, Liu P, McIntyre S, et al. Prognostic factors for survival in melanoma patients with brain metastases. Cancer. 2011;117(8):1687–96.
Ferguson SD, Bindal S, Bassett RL, Jr., et al. Predictors of survival in metastatic melanoma patients with leptomeningeal disease (LMD). J Neurooncol. 2019;142(3):499-509. (Largest contemporary cohort of melanoma LMD patients, describing the outcome and predictors of survival.)
Le Rhun E, Taillibert S, Chamberlain MC. Carcinomatous meningitis: leptomeningeal metastases in solid tumors. Surg Neurol Int. 2013;4(Suppl 4):S265-288. (Excellent overview of diagnosis, presentation, and OS of LMD from solid tumors in general.)
Taillibert S, Chamberlain MC. Leptomeningeal metastasis. Handb Clin Neurol. 2018;149:169–204.
Wang N, Bertalan MS, Brastianos PK. Leptomeningeal metastasis from systemic cancer: review and update on management. Cancer. 2018;124(1):21–35.
Cagney DN, Lamba N, Sinha S, et al. Association of neurosurgical resection with development of pachymeningeal seeding in patients with brain metastases. JAMA Oncol. 2019;5(5):703–9.
Chamberlain M, Junck L, Brandsma D, et al. Leptomeningeal metastases: a RANO proposal for response criteria. Neuro Oncol. 2017;19(4):484–92.
Glantz MJ, Cole BF, Glantz LK, et al. Cerebrospinal fluid cytology in patients with cancer: minimizing false-negative results. Cancer. 1998;82(4):733–9.
Boire A, Brandsma D, Brastianos PK, et al. Liquid biopsy in central nervous system metastases: a RANO review and proposals for clinical applications. Neuro Oncol. 2019;21(5):571-584. (Outstanding contemporary review of the state of liquid biopsies for CNS metastases.)
Lin X, Fleisher M, Rosenblum M, et al. Cerebrospinal fluid circulating tumor cells: a novel tool to diagnose leptomeningeal metastases from epithelial tumors. Neuro Oncol. 2017;19(9):1248–54.
Miller AM, Shah RH, Pentsova EI, et al. Tracking tumour evolution in glioma through liquid biopsies of cerebrospinal fluid. Nature. 2019;565(7741):654–8.
Le Rhun E, Tu Q, De Carvalho BM, et al. Detection and quantification of CSF malignant cells by the Cell Search technology in patients with melanoma leptomeningeal metastasis. Med Oncol. 2013;30(2):538.
Smalley I, Evernden B, Law V, et al. Abstract 2108: detection and molecular profiling of leptomeningeal disease in melanoma. Can Res. 2018;78(13 Supplement):2108–2108.
Pentsova EI, Shah RH, Tang J, et al. Evaluating cancer of the central nervous system through next-generation sequencing of cerebrospinal fluid. J Clin Oncol. 2016;34(20):2404-2415. (The first large scale sequencing of CSF.)
De Mattos-Arruda L, Mayor R, Ng CKY, et al. Cerebrospinal fluid-derived circulating tumour DNA better represents the genomic alterations of brain tumours than plasma. Nat Commun. 2015;6:8839.
Fan Y, Zhu X, Xu Y, et al. Cell-cycle and DNA-damage response pathway is involved in leptomeningeal metastasis of non-small cell lung cancer. Clin Cancer Res. 2018;24(1):209–16.
Li YS, Jiang BY, Yang JJ, et al. Unique genetic profiles from cerebrospinal fluid cell-free DNA in leptomeningeal metastases of EGFR-mutant non-small-cell lung cancer: a new medium of liquid biopsy. Ann Oncol. 2018;29(4):945–52.
Marchiò C, Mariani S, Bertero L, et al. Liquoral liquid biopsy in neoplastic meningitis enables molecular diagnosis and mutation tracking: a proof of concept. Neuro Oncol. 2017;19(3):451–3.
Momtaz P, Pentsova E, Abdel-Wahab O, et al. Quantification of tumor-derived cell free DNA(cfDNA) by digital PCR (DigPCR) in cerebrospinal fluid of patients with BRAFV600 mutated malignancies. Oncotarget. 2016;7(51):85430–6.
Siravegna G, Geuna E, Mussolin B, et al. Genotyping tumour DNA in cerebrospinal fluid and plasma of a HER2-positive breast cancer patient with brain metastases. ESMO Open. 2017;2(4):e000253.
Siravegna G, Marsoni S, Siena S, Bardelli A. Integrating liquid biopsies into the management of cancer. Nat Rev Clin Oncol. 2017;14(9):531–48.
Ballester LY, Glitza Oliva IC, Douse DY, et al. Evaluating circulating tumor DNA from the cerebrospinal fluid of patients with melanoma and leptomeningeal disease. J Neuropathol Exp Neurol. 2018;77(7):628–35.
Abaskharoun M. A Randomized, Double-Blind Phase 2/3 Study of Relatlimab Combined with Nivolumab versus Nivolumab in Participants with Previously Untreated Metastatic or Unresectable Melanoma. 2019.
Havel JJ, Chowell D, Chan TA. The evolving landscape of biomarkers for checkpoint inhibitor immunotherapy. Nat Rev Cancer. 2019;19(3):133–50.
Yu X, Huang X, Chen X, et al. Characterization of a novel anti-human lymphocyte activation gene 3 (LAG-3) antibody for cancer immunotherapy. MAbs. 2019;11(6):1139–48.
Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23.
Koller KM, Mackley HB, Liu J, et al. Improved survival and complete response rates in patients with advanced melanoma treated with concurrent ipilimumab and radiotherapy versus ipilimumab alone. Cancer Biol Ther. 2017;18(1):36–42.
Schadendorf D, Hodi FS, Robert C, et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33(17):1889–94.
Margolin K, Ernstoff MS, Hamid O, et al. Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol. 2012;13(5):459–65.
Bot I, Blank CU, Brandsma D. Clinical and radiological response of leptomeningeal melanoma after whole brain radiotherapy and ipilimumab. J Neurol. 2012;259(9):1976–8.
Wu RC, Newman W, Patanowitz L, Branstetter BF, Amankulor N, Tarhini AA. Long-term control of leptomeningeal disease after radiation therapy and nivolumab in a metastatic melanoma patient. Immunotherapy. 2020;12(11):763–9.
Glitza I, Bucheit A. Clinical response of central nervous system melanoma to anti-PD1 therapy in 2 melanoma patients. Arch Immunol. 2017;1(1):1–3.
Long GV, Atkinson V, Lo S, et al. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol. 2018.
National Institute of Health (NIH) Cg. Tumors metastatic to brain. 2021.
Fedorenko IV, Gibney GT, Sondak VK, Smalley KSM. Beyond BRAF: where next for melanoma therapy? Brit J Cancer. 2015;112(2):217–26.
Arasaratnam M, Hong A, Shivalingam B, et al. Leptomeningeal melanoma—a case series in the era of modern systemic therapy. Pigment Cell Melanoma Res. 2018;31(1):120–4.
Mittapalli RK, Vaidhyanathan S, Sane R, Elmquist WF. Impact of P-glycoprotein (ABCB1) and breast cancer resistance protein (ABCG2) on the brain distribution of a novel BRAF inhibitor: vemurafenib (PLX4032). J Pharmacol Exp Ther. 2012;342(1):33–40.
Mittapalli RK, Vaidhyanathan S, Dudek AZ, Elmquist WF. Mechanisms limiting distribution of the threonine-protein kinase B-RaF(V600E) inhibitor dabrafenib to the brain: implications for the treatment of melanoma brain metastases. J Pharmacol Exp Ther. 2013;344(3):655–64.
Davies MA, Saiag P, Robert C, et al. Dabrafenib plus trametinib in patients with BRAFV600-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol. 2017;18(7):863–73.
Sakji-Dupre L, Le Rhun E, Templier C, Desmedt E, Blanchet B, Mortier L. Cerebrospinal fluid concentrations of vemurafenib in patients treated for brain metastatic BRAF-V600 mutated melanoma. Melanoma Res. 2015;25(4):302–5.
Lee JM, Mehta UN, Dsouza LH, Guadagnolo BA, Sanders DL, Kim KB. Long-term stabilization of leptomeningeal disease with whole-brain radiation therapy in a patient with metastatic melanoma treated with vemurafenib: a case report. Melanoma Res. 2013;23(2):175–8.
Schäfer N, Scheffler B, Stuplich M, et al. Vemurafenib for leptomeningeal melanomatosis. J Clin Oncol. 2013;31(11):e173-174.
Kim DW, Barcena E, Mehta UN, et al. Prolonged survival of a patient with metastatic leptomeningeal melanoma treated with BRAF inhibition-based therapy: a case report. BMC Cancer. 2015;15:400.
Wilgenhof S, Neyns B. Complete cytologic remission of V600E BRAF-mutant melanoma-associated leptomeningeal carcinomatosis upon treatment with dabrafenib. J Clin Oncol. 2015;33(28):e109-111.
Abu-Gheida I, Chao S, Murphy E, et al. Targeted therapy after brain radiotherapy for BRAF-mutated melanoma with extensive ependymal disease with prolonged survival: case report and review of the literature. Front Oncol. 2019;9:168.
Floudas CS, Chandra AB, Xu Y. Vemurafenib in leptomeningeal carcinomatosis from melanoma: a case report of near-complete response and prolonged survival. Melanoma Res. 2016;26(3):312–5.
Glitza IC, Ferguson SD, Guha-Thakurta N. Rapid resolution of leptomeningeal disease with targeted therapy in a metastatic melanoma patient. J Neurooncol. 2017;133(3):663–5.
GeukesFoppen MH, Brandsma D, Blank CU, van Thienen JV, Haanen JB, Boogerd W. Targeted treatment and immunotherapy in leptomeningeal metastases from melanoma. Ann Oncol. 2016;27(6):1138–42.
DeVita VT, Lawrence, T.S., Rosenberg, S.A. DeVita, Hellman, and Rosenberg’s Cancer: Principles & Practice of Oncology. 11th ed. 2011.
Gammon DC, Bhatt MS, Tran L, Van Horn A, Benvenuti M, Glantz MJ. Intrathecal topotecan in adult patients with neoplastic meningitis. Am J Health Syst Pharm. 2006;63(21):2083–6.
Grossman SA, Finkelstein DM, Ruckdeschel JC, Trump DL, Moynihan T, Ettinger DS. Randomized prospective comparison of intraventricular methotrexate and thiotepa in patients with previously untreated neoplastic meningitis. Eastern Cooperative Oncology Group. J Clin Oncol. 1993;11(3):561–9.
Lukas RV, Mata-Machado NA, Nicholas MK, Salgia R, Antic T, Villaflor VM. Leptomeningeal carcinomatosis in esophageal cancer: a case series and systematic review of the literature. Dis Esophagus. 2015;28(8):772–81.
Pape E, Desmedt E, Zairi F, et al. Leptomeningeal metastasis in melanoma: a prospective clinical study of nine patients. In Vivo. 2012;26(6):1079–86.
Blaney SM, Balis FM, Poplack DG. Pharmacologic approaches to the treatment of meningeal malignancy. Oncology (Williston Park). 1991;5(5):107–16 (discussion 123, 127).
Patil S, Rathnum KK. Management of leptomeningeal metastases in non-small cell lung cancer. Indian J Cancer. 2019;56(Supplement):S1–9.
Tsujimura M, Kusamori K, Nishikawa M. Rapid regulation of human mesenchymal stem cell proliferation using inducible caspase-9 suicide gene for safe cell-based therapy. Int J Mol Sci. 2019;20(22).
De Clercq E, Edy VG, De Vlieger H, Eeckels R, Desmyter J. Intrathecal administration of interferon in neonatal herpes. J Pediatr. 1975;86(5):736–9.
Meyers CA, Obbens EA, Scheibel RS, Moser RP. Neurotoxicity of intraventricularly administered alpha-interferon for leptomeningeal disease. Cancer. 1991;68(1):88–92.
List J, Moser RP, Steuer M, Loudon WG, Blacklock JB, Grimm EA. Cytokine responses to intraventricular injection of interleukin 2 into patients with leptomeningeal carcinomatosis: rapid induction of tumor necrosis factor alpha, interleukin 1 beta, interleukin 6, gamma-interferon, and soluble interleukin 2 receptor (Mr 55,000 protein). Cancer Res. 1992;52(5):1123–8.
Samlowski WE, Park KJ, Galinsky RE, Ward JH, Schumann GB. Intrathecal administration of interleukin-2 for meningeal carcinomatosis due to malignant melanoma: sequential evaluation of intracranial pressure, cerebrospinal fluid cytology, and cytokine induction. J Immunother Emphasis Tumor Immunol. 1993;13(1):49–54.
Papadopoulos N, Gerber D, Eton O, Bedikian A. The role of intrathecal (IT) use of interleukin-2 (IL-2) in the treatment of leptomeningeal disease (LMD) in patients (pts) with melanoma. Paper presented at: Proc Am Soc Clin Oncol. 2002.
Glitza IC, Rohlfs M, Guha-Thakurta N, et al. Retrospective review of metastatic melanoma patients with leptomeningeal disease treated with intrathecal interleukin-2. ESMO Open. 2018;3(1):e000283.
Clemons-Miller AR, Chatta GS, Hutchins L, et al. Intrathecal cytotoxic T-cell immunotherapy for metastatic leptomeningeal melanoma. Clin Cancer Res. 2001;7(3 Suppl):917s–24s.
Glitza IC, Haymaker C, Bernatchez C, et al. Intrathecal administration of tumor-infiltrating lymphocytes is well tolerated in a patient with leptomeningeal disease from metastatic melanoma: a case report. Cancer Immunol Res. 2015;3(11):1201-1206. (The largest cohort of melanoma LMD patients treated with intrathecal interleukin-2.)
Sridhar P, Petrocca F. Regional delivery of chimeric antigen receptor (CAR) T-cells for cancer therapy. Cancers (Basel). 2017;9(7).
Land CA, Musich PR, Haydar D, Krenciute G, Xie Q. Chimeric antigen receptor T-cell therapy in glioblastoma: charging the T cells to fight. J Transl Med. 2020;18(1):428.
Pluim D, Ros W, van Bussel MTJ, Brandsma D, Beijnen JH, Schellens JHM. Enzyme linked immunosorbent assay for the quantification of nivolumab and pembrolizumab in human serum and cerebrospinal fluid. J Pharm Biomed Anal. 2019;164:128–34.
van Bussel MTJ, Beijnen JH, Brandsma D. Intracranial antitumor responses of nivolumab and ipilimumab: a pharmacodynamic and pharmacokinetic perspective, a scoping systematic review. BMC Cancer. 2019;19(1):519.
Huppert LA, Melisko ME, Glastonbury CM, Khanafshar E, Daud AI. Treatment of metastatic melanoma with leptomeningeal disease using intrathecal immunotherapy. JCO Oncol Pract. 2020;16(11):757–9.
Ommaya AK. Subcutaneous reservoir and pump for sterile access to ventricular cerebrospinal fluid. Lancet. 1963;2(7315):983-984. (Dr. Ommaya communicates for the first time his invention of the Ommaya reservoir for IT treatment.)
Bauer DF, Razdan SN, Bartolucci AA, Markert JM. Meta-analysis of hemorrhagic complications from ventriculostomy placement by neurosurgeons. Neurosurgery. 2011;69(2):255–60.
Prandoni P, Lensing AW, Piccioli A, et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood. 2002;100(10):3484–8.
Horsted F, West J, Grainge MJ. Risk of venous thromboembolism in patients with cancer: a systematic review and meta-analysis. PLoS Med. 2012;9(7):e1001275.
Mead PA, Safdieh JE, Nizza P, Tuma S, Sepkowitz KA. Ommaya reservoir infections: a 16-year retrospective analysis. J Infect. 2014;68(3):225–30 undefinedOmmaya and risk of infection, showing the risk of infection being generally acceptable, with OmR infection occurring in one of every 20 persons with the device.
Szvalb AD, Raad II, Weinberg JS, Suki D, Mayer R, Viola GM. Ommaya reservoir-related infections: clinical manifestations and treatment outcomes. J Infect. 2014;68(3):216–24.
Bin Nafisah S, Ahmad M. Ommaya reservoir infection rate: a 6-year retrospective cohort study of Ommaya reservoir in pediatrics. Childs Nerv Syst. 2015;31(1):29–36.
Greenfield JP, Schwartz TH. Catheter placement for Ommaya reservoirs with frameless surgical navigation: technical note. Stereotact Funct Neurosurg. 2008;86(2):101–5.
Wilson TJ, Stetler WR Jr, Al-Holou WN, Sullivan SE. Comparison of the accuracy of ventricular catheter placement using freehand placement, ultrasonic guidance, and stereotactic neuronavigation. J Neurosurg. 2013;119(1):66–70.
Kennedy BC, Brown LT, Komotar RJ, McKhann GM 2nd. Stereotactic catheter placement for Ommaya reservoirs. J Clin Neurosci. 2016;27:44–7.
Chamberlain MC. Radioisotope CSF flow studies in leptomeningeal metastases. J Neurooncol. 1998;38(2–3):135–40.
Omuro AM, Lallana EC, Bilsky MH, DeAngelis LM. Ventriculoperitoneal shunt in patients with leptomeningeal metastasis. Neurology. 2005;64(9):1625–7.
Kim HS, Park JB, Gwak H-S, Kwon J-W, Shin S-H, Yoo H. Clinical outcome of cerebrospinal fluid shunts in patients with leptomeningeal carcinomatosis. World J Surg Oncol. 2019;17(1):59.
Jung TY, Chung WK, Oh IJ. The prognostic significance of surgically treated hydrocephalus in leptomeningeal metastases. Clin Neurol Neurosurg. 2014;119:80–3.
Murakami Y, Ichikawa M, Bakhit M, et al. Palliative shunt surgery for patients with leptomeningeal metastasis. Clin Neurol Neurosurg. 2018;168:175–8.
Brower JV, Saha S, Rosenberg SA, Hullett CR, Ian RH. Management of leptomeningeal metastases: prognostic factors and associated outcomes. J Clin Neurosci. 2016;27:130–7.
Chamberlain M, Kormanik P. Leptomeningeal metastases due to melanoma. Int J Oncol. 1996;9(3):505–10.
Cao Y, Tsien CI, Shen Z, et al. Use of magnetic resonance imaging to assess blood-brain/blood-glioma barrier opening during conformal radiotherapy. J Clin Oncol. 2005;23(18):4127–36.
Brown PD, Pugh S, Laack NN, et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol. 2013;15(10):1429–37.
Chowdhary S, Chamberlain M. Leptomeningeal metastases: current concepts and management guidelines. J Natl Compr Canc Netw. 2005;3(5):693–703.
Yang TJ, Wijetunga NA, Yamada J, et al. Clinical trial of proton craniospinal irradiation for leptomeningeal metastases. Neuro Oncol. 2020. (This Phase I study of proton craniospinal radiation for leptomeningeal disease represents a potential novel approach to offering comprehensive RT for LMD from metastatic solid malignancies to the entire CSF. The outcomes in comparison to the standard of care of WBRT and partial spinal RT will be studied in a current randomized controlled trial to inform management for the future.)
Devecka M, Duma MN, Wilkens JJ, et al. Craniospinal irradiation(CSI) in patients with leptomeningeal metastases: risk-benefit-profile and development of a prognostic score for decision making in the palliative setting. BMC Cancer. 2020;20(1):501.
Yeboa DN, Gibbs IC. Stereotactic radiotherapy and resection of brain metastases: the role of hypofractionation. JAMA Oncol. 2020. (Contemporary summary of the role of hypofractionation, with a focus on LMD risk.)
Bertke MH, Burton EC, Shaughnessy JN. Stereotactic radiosurgery as part of multimodal treatment in a bulky leptomeningeal recurrence of breast cancer. Cureus. 2016;8(3):e523.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yolanda Piña declares that she has no conflict of interest. Sirisha Yadugiri declares that she has no conflict of interest. Debra N. Yeboa declares that she has no conflict of interest. Sherise D. Ferguson has received research funding from Codiak BioSciences. Peter A. Forsyth declares that he has no conflict of interest. Isabella C. Glitza Oliva declares that he has no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Melanoma
Rights and permissions
About this article
Cite this article
Piña, Y., Yadugiri, S., Yeboa, D.N. et al. Advances in Diagnosis and Treatment for Leptomeningeal Disease in Melanoma. Curr Oncol Rep 24, 43–54 (2022). https://doi.org/10.1007/s11912-021-01162-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-021-01162-3