Abstract
Diabetic nephropathy, or diabetic kidney disease (DKD), is the most serious complication of diabetes mellitus (DM). Despite recent advances in therapy, DKD still often progresses to end-stage renal disease (ESRD). Recent studies have suggested that pentoxifylline (PTX) may be efficacious in the treatment of DKD. PTX is a rheologic modifier approved for use in the USA for the symptomatic relief of claudication. It competitively inhibits phosphodiesterase (PDE), resulting in increased intracellular cyclic AMP (cAMP), activation of protein kinase A (PKA), inhibition of interleukin (IL) and tumor necrosis factor (TNF) synthesis, and reduced inflammation. PTX improves red blood cell deformability, reduces blood viscosity, and decreases platelet aggregation. In combination with renin-angiotensin-aldosterone (RAAS) blockers, PTX may help prevent progression to ESRD in patients with DKD. This review focuses on the possible mechanisms of action of PTX in DKD and studies suggesting possible efficacy of this old drug for a new indication.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Alsaad KO, Herzenberg AM. Distinguishing diabetic nephropathy from other causes of glomerulosclerosis: an update. J Clin Pathol. 2007;60(1):18–26.
Cravedi P, Remuzzi G. Pathophysiology of proteinuria and its value as an outcome measure in chronic kidney disease. Br J Clin Phamacol. 2013;76(4):516–23. The authors conclude that proteinuria is a valuable surrogate end point for clinical trials in patients with chronic renal diseases and a target for reno- and cardioprotective strategies.
Gregg E, Li Y, Wang J, Burrows N, Ali M, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–23. Rates of diabetes-related complications have declined substantially in the past two decades, but a large burden of disease persists because of the continued increase in the prevalence of diabetes.
Rossing K, Christensen PK, Hovind P, Tarnow L, Rossing P, Parving HH. Progression of nephropathy in type 2 diabetic patients. Kidney Int. 2004;66(4):1596–605.
Kawabata N, Kawamura T, Utsunomiya K, Kusano E. High salt intake is associated with renal involvement in Japanese patients with type 2 diabetes mellitus. Intern Med. 2015;54(3):311–7. This study investigated clinical and nutritional factors that contribute to renal disease in type 2 diabetes.
Haffner S, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial Infarction. N Engl J Med. 1998;339(4):229–34.
Afkarian M, Sachs M, Kestenbaum B, Hirsch I, Tuttle K, Himmelfarb J, et al. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol. 2013;24(2):302–8. This is an analysis of cardiovascular and non-cardiovascular causes of mortality of patients with type 2 diabetes. The data suggest that diabetes is equivalent to prior myocardial infarction as a cardiovascular risk factor.
National Kidney Foundation. KDOQI clinical practice guideline for diabetes and CKD: 2012 update. Am J Kidney Dis. 2012;60:850–86.
Parving HH, Brenner BM, McMurray JJ, de Zeeuw D, Haffner SM, Solomon SD, et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. N Engl J Med. 2012;367(23):2204–13. The addition of aliskiren to standard RAAS blockade in patients with type 2 diabetes who are at high risk for cardiovascular and renal events may be harmful.
Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin inhibition for treatment of diabetic nephropathy. N Engl J Med. 2013;369:1892–903. Compared to ARB monotherapy, combination therapy with an ACE inhibitor and an ARB was associated with an increased risk of adverse events among patients with diabetic nephropathy.
De Sanctis M, Cesarone M, Belcaro G. Treatment of intermittent claudication with pentoxifylline: a 12-month, randomized trial—walking distance and microcirculation. Angiology. 2002;53 Suppl 1:S7–S12.
Aviado DM, Dettelbach HR. Pharmacology of pentoxifylline, a hemorheologic agent for the treatment of intermittent claudication. Angiology. 1984;35(7):407–17.
Aviado DM, Porter JM. Pentoxifylline: a new drug for the treatment of intermittent claudication. Mechanism of action, pharmacokinetics, clinical efficacy and adverse effects. Pharmacotherapy. 1984;4(6):297–307.
Rames A, Poirier JM, LeCoz F, et al. Pharmacokinetics of intravenous and oral pentoxifylline in healthy volunteers and in cirrhotic patients. Clin Pharmacol Ther. 1990;47:354–9.
Rodríguez-Morán M, Guerrero-Romero F. Efficacy of pentoxifylline in the management of microalbuminuria in patients with diabetes. Curr Diabetes Rev. 2008;4(1):55–62.
Ward A, Clissold S. Pentoxifylline: a review of its pharmacodynamics and pharmacokinetic properties and its therapeutic efficacy. Drugs. 1987;34(1):50–97.
Navarro J, Mora C. Role of inflammation in diabetic complications. Nephrol Dial Transplant. 2005;20(12):2601–4.
Dávila-Esqueda M, Martínez-Morales F. Pentoxifylline diminishes the oxidative damage to renal tissue induced by streptozotocin in the rat. Exp Diabesity Res. 2004;5(4):245–51.
Elmarakby A, Sullivan J. Relationship between oxidative stress and inflammatory cytokines in diabetic nephropathy. Cardiovasc Ther. 2012;30(1):49–59.
Navarro JF, Mora C, Rivero A, et al. Urinary protein excretion and serum tumor necrosis factor in diabetic patients with advanced renal failure: effects of pentoxifylline administration. Am J Kidney Dis. 1999;33:458–63.
Mora C, Navarro JF. Inflammation and diabetic nephropathy. Curr Diab Rep. 2006;6:463–8.
Pickup JC, Roberts GA, Kehely AM, Pasapula C, Chusney GD, Mather HM. Higher serum sialic acid in women than in men with NIDDM: possible relevance to increased cardiovascular risk in NIDDM women. Diabetes Care. 1997;20:1496.
Johansen JS, Harris AK, Rychly DJ, Ergul A. Oxidative stress and the use of antioxidants in diabetes: linking basic science to clinical practice. Cardiovasc Diabetol. 2005;4:5.
Fredholm BB, Perssob CGA. Xanthine derivatives as adenosine receptor antagonists. Eur J Phrarmacol. 1982;81:673–6.
Angielski S, Jakubowski Z, Pawelczyk T, Piec G, Redlak M. Renal handling and metabolism of adenosine in diabetic rats. Contrib Nephrol. 1989;73:52–7.
Schmidt A, Yan S, Wautier J, Stern D. Activation of receptor for advanced glycation end products: a mechanism for chronic vascular dysfunction in diabetic vasculopathy and atherosclerosis. Circ Res. 1999;84(5):489–97.
Hayaishi-Okano R, Yamasaki Y, Katakami N, Ohtoshi K, Gorogawa S, Kuroda A, et al. Elevated C-reactive protein associates with early-stage carotid atherosclerosis in young subjects with type 1 diabetes. Diabetes Care. 2002;25(8):1432–8.
Goicoechea M, Garcia de Vinuesa S, Quiroga B, Verdalles U, Barraca D, Yuste C, et al. Effects of pentoxifylline on inflammatory parameters in chronic kidney disease patients: a randomized trial. J Nephrol. 2012;25:969–75. In a randomized trial, inflammatory markers—e.g., high-sensitivity C-reactive protein (hs-CRP), serum fibrinogen and TNF-alpha—were decreased by pentoxifylline in patients with chronic kidney disease.
Han J, Thompson P, Beutler D. Dexamethasone and pentoxifylline inhibit endotoxin-induced cachectin/tumor necrosis factor synthesis at separate points in the signaling pathway. J Exp Med. 1990;172:393–4.
Doherty GM, Jensen JC, Alexander HR, Buresh CM, Norton JA. Pentoxifyl line suppression of tumor necrosis factor gene transcription. Surgery. 1991;110:192–8.
Ortiz A, González-Cuadrado R, Sharma M, et al. Tumor necrosis factor as a mediator of glomerular damage. J Nephrol. 1995;8:27–34.
Kalantarinia K, Awad AS, Siragy HM. Urinary and renal interstitial concen trations of TNF-alpha increase prior to the rise in albuminuria in diabetic rats. Kidney Int. 2003;64:1208–13.
Navarro JF, Milena FJ, Mora C, Leon C, Garcia J. Renal pro-inflammatory cytokine gene expression in diabetic nephropathy: effect of angiotensin- converting enzyme inhibition and pentoxifylline administration. Am J Nephrol. 2006;26:562–70.
Royall JA, Berkow RL, Beckman JS, Cunningham MK, Matalon S, Freeman BA. Tumor necrosis factor and interleukin 1 alpha increase vascular endothelial permeability. Am J Physiol. 1989;257(6 Pt 1):L399–410.
Dalla Vestra M, Mussap M, Gallina P, et al. Acute-phase markers of inflammation and glomerular structure in patients with type 2 diabetes. J Am Soc Nephrol. 2005;16 Suppl 1:S78–82.
Dipetrillo K, Coutermarsh B, Gesek FA. Urinary tumor necrosis factor contributes to sodium retention and renal hypertrophy during diabetes. Am J Physiol Ren Physiol. 2003;284:F113–21.
Strutz F, Heeg M, Kochsiek T, et al. Effects of pentoxifylline, pentifylline and gamma-interferon on proliferation, differentiaton and matrix synthesis of human renal fibroblasts. Nephrol Dial Transplant. 2000;15(10):1535–46.
Han KH, Han SY, Kim HS, Kang YS, Cha DR. Prolonged administration enhances the renoprotective effect of pentoxifylline via anti-inflammatory activity in streptozotocin-induced diabetic nephropathy. Inflammation. 2010;33(3):137–43.
Sun HK, Lee YM, Han KH, Kim HS, Ahn SH, Han SY. Phosphodiesterase inhibitor improves renal tubulointerstitial hypoxia of the diabetic rat kidney. Korean J Intern Med. 2012;27(2):163–70.
Badri S, Dashti-Khavidaki S, Lessan-Pezeshki M, Abdollahi M. A review of the potential benefits of pentoxifylline in diabetic and non-diabetic proteinuria. J Pharm Pharm Sci. 2011;14(1):128–37.
An ZM, Dong XG, Guo Y, Zhou JL, Qin T. Effects and clinical significance of pentoxifylline on the oxidative stress of rats with diabetic nephropathy. Huazhong Univ Sci Technolog Med Sci. 2015;35(3):356–61.
Nangaku M. Mechanisms of tubulointerstitial injury in the kidney: final common pathways to end-stage renal failure. Intern Med. 2004;43(1):9–17.
Abdel-Salam OM, Baiuomy AR, El-Shenawy SM, Arbid MS. The anti-inflammatory effects of the phosphodiesterase inhibitor pentoxifylline in the rat. Pharmacol Res. 2003;47:331–40.
de Zeeuw D, Remuzzi G, Parving H, Keane W, Zhang Z, Shahinfar S, et al. Proteinuria, a target for renoprotection in patients with type 2 diabetic nephropathy: lessons from RENAAL. Kidney Int. 2004;65(6):2309–20.
Ghorbani A, Omidvar B, Beladi-Mousavi SS, Lak E, Vaziri S. The effect of pentoxifylline on reduction of proteinuria among patients with type 2 diabetes under blockade of angiotensin system: a double blind and randomized clinical trial. Nefrologia. 2012;32(6):790–6. Pentoxifylline has an antiproteinuric effect and may slow the decrease in GFR among patients with type 2 DM receiving RAAS blockers.
Shan D, Wu H, Yuan Q, Li J, Zhou R, Liu G. Pentoxifylline for diabetic kidney disease. Cochrane Database Syst Rev. 2012;2, CD006800. This was a meta-analysis looking at the risks and benefits of pentoxifylline as a treatment option in patients with diabetic nephropathy.
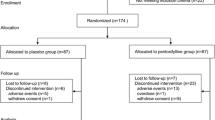
Navarro-Gonzalez J, Mora-Fernandez C, Fuentes M, Chahin J, Mendez M, Gallego E, et al. Effect of pentoxifylline on renal function and urinary albumin excretion in patients with diabetic kidney disease: the PREDIAN trial. J Am Soc Nephrol. 2015;26(1):220–9. This was a single-centered randomized controlled clinical trial (169 patients) that explored the benefits and harms of pentoxifylline as add-on treatment (in addition to RAAS blockers) for diabetic nephropathy. Pentoxifylline had renoprotective effects (antiproteinuric and slowed decline of eGFR).
Cowie C, Port F, Wolfe R, Savage P, Moll P, Hawthorne V. Disparities in incidence of diabetic end-stage renal disease according to race and type of diabetes. N Engl J Med. 1989;321(16):1074–9.
Chen P, Lai T, Chen P, Lai C, Wu V, Chiang W, et al. Renoprotective effect of combining pentoxifylline with angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker in advanced chronic kidney disease. J Formos Med Assoc. 2015;114(1):95–6. A single-center retrospective study of the effects of pentoxifylline in combination with ACEi/ARBs (661 patients) as a therapeutic treatment option in patients chronic kidney disease.
Tian ML, Shen Y, Sun ZL, Zha Y. Efficacy and safety of combining pentoxifylline with angiotensin-converting enzyme inhibitor or angiotensin II receptor blocker in diabetic nephropathy: a meta-analysis. Int Urol Nephrol. 2015;47(5):815–22. This was a meta-analysis indicating that pentoxifylline has antiproteinuric effects patients with DKD undergoing RAAS blockade. The authors state that further large, multicenter, high-quality studies with long duration are necessary to determine it really has renoprotective effects in this patient population.
Han SJ, Kim HJ, Kim DJ, Sheen SS, Chung CH, Ahn CW, et al. Effects of pentoxifylline on proteinuria and glucose control in patients with type 2 diabetes: a prospective randomized double-blind multicenter study. Diabetol Metab Syndr. 2015;7:64. Pentoxifylline reduced proteinuria and improved glucose control and insulin resistance without significant change of serum TNF-α in patients with type 2 diabetic nephropathy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Drs. Leehey and Bhanot declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Therapeutic Trials
Rights and permissions
About this article
Cite this article
Bhanot, S., Leehey, D.J. Pentoxifylline for Diabetic Nephropathy: an Important Opportunity to Re-purpose an Old Drug?. Curr Hypertens Rep 18, 8 (2016). https://doi.org/10.1007/s11906-015-0612-7
Published:
DOI: https://doi.org/10.1007/s11906-015-0612-7