Abstract
Purpose of Review
This review aims to discuss the unique challenges that adult congenital heart disease (ACHD) patients present in the intensive care unit.
Recent Findings
Recent studies suggest that ACHD patients make up an increasing number of ICU admissions, and that their care greatly improves in centers with specialized ACHD care. Common reasons for admission include arrhythmia, hemorrhage, heart failure, and pulmonary disease.
Summary
It is critical that the modern intensivist understand not only the congenital anatomy and subsequent repairs an ACHD patient has undergone, but also how that anatomy can predispose the patient to critical illness. Additionally, intensivists should rely on a multidisciplinary team, which includes an ACHD specialist, in the care of these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to advances in the recognition and management of congenital heart disease (CHD), the survival of patients in the pediatric population has dramatically increased. Survival into adulthood is now expected for 90% of children diagnosed with CHD, and more adults are estimated to be living with CHD than children [1,2,3,4]. As the adult congenital heart disease (ACHD) population continues to grow, the prevalence of hospitalization and intensive care unit admission for these patients has also increased [5]. One Critical Care Cardiology Trials Network study showed that ACHD patients make up approximately 2% of all cardiac intensive care unit (CICU) admissions [6]. Despite their relatively small number, these patients present unique anatomic and physiologic challenges in the adult ICU that the contemporary intensivist should be familiar with. In a single-center study of 138 ACHD ICU admissions, the most common reasons for admission were arrhythmia, hemorrhage, heart failure, and pulmonary disease [7•]. This review aims to discuss practical disease-specific management strategies and general ICU considerations for the ACHD patient.
General Principles
Successfully caring for the critically ill ACHD patient depends on the practicing intensivist knowing their patient and adjusting their management for personalized care depending on the underlying CHD. Understanding the initial congenital anatomy, as well as the subsequent surgical and transcatheter repairs, is a crucial first step. Reviewing surgical or catheterization reports can lead to key insights on potential triggers for decompensation. If these reports are unavailable, providers must be able to reverse engineer this history from available imaging (whether it be echocardiographic or cross-sectional). In addition to characterizing the cardiac substrate, the baseline end-organ function should be determined; several ACHD patients, particularly those with Fontan circulations, have concomitant pulmonary, renal, hepatologic, and hematologic dysfunction that can further complicate critical illness. Reviewing objective data is necessary, as ACHD patients may not be able to provide the details of their prior history and, at times were misinformed that they were “cured” following childhood surgery [8].
Given the highly multifaceted nature of managing the critically ill ACHD patient, it is imperative that intensivists seek the insight and guidance of a multidisciplinary team, especially the ACHD specialist. Depending on the underlying anatomy and illness, this can include specialists in cardiac surgery, interventional cardiology, electrophysiology, imaging, advanced heart failure, and non-cardiac specialists such as hepatology, nephrology, and pulmonology. In all cases, intensivists should seek the input and collaboration of a provider with specific expertise in adult congenital heart disease [9, 10]. ACHD patients cared for in centers with ACHD expertise have better outcomes than those patients in centers without this expertise, including improved mortality [11]. If a given center is unable to provide this level of expertise, patient transfer to a more appropriately equipped center should be explored if the patient can be safely transported [12].
Whether ACHD patients are best cared for in a pediatric or adult intensive care unit is controversial. While providers in a pediatric setting are likely more familiar with the underlying anatomic underpinnings of CHD, those in an adult setting may have more experience in managing the multiple comorbidities often associated with adulthood. This decision should be made on a case-by-case basis, as whichever setting has the resources that best match the patient’s needs is likely most appropriate.
Hemodynamic Assessment
An accurate and thorough hemodynamic assessment can be vital in identifying etiologies of critical illness and monitoring response to therapy in ACHD patients. An assessment of blood pressure, peripheral oxygenation, cardiac output, systemic resistance, and pulmonary resistance should be obtained, and compared to baseline “well” evaluations; while a systolic blood pressure less than 90 mmHg or oxygenation saturation of less than 88% may identify critical illness in some patients, these values could represent baseline conditions in some ACHD anatomies [13]. Furthermore, complex congenital anatomy can present several challenges in otherwise routine hemodynamic monitoring. This is particularly true in measuring the blood pressure, as both non-invasive and invasive blood pressure readings can be falsely low in the setting of a prior classic Blalock-Thomas-Taussig (BTT) shunt due to anastomosis of the subclavian and pulmonary arteries [14]. If an invasive arterial line is needed, the radial artery of the arm not affected by the shunt or a femoral artery should be used. A similar situation may be encountered in patients with severe coarctation, where the initial coarctation site and the subsequent repairs can affect accurate blood pressure assessment. In patients with a shunt, such as a patent ductus arteriosus (PDA) and Eisenmenger syndrome, care must be given to obtaining saturations pre- and post-shunt, in both upper and lower extremities to assess pre- and post-ductal saturations and estimate shunting.
While invasive real-time hemodynamic monitoring using a pulmonary artery catheter is returning to prominence in the CICU, this can be challenging and potentially contra-indicated in certain congenital anatomies [15]. In some scenarios, it can be misleading; in patients with pulmonary atresia with multi-level branch pulmonary stenosis (PS), a wedge pressure may be inaccurately elevated at the site of PS, and a direct left ventricular (LV) end-diastolic pressure (EDP) is the more accurate assessment of LV preload. Furthermore, in severe right ventricular (RV) to pulmonary artery (PA) conduit stenosis, an elevated RV systolic pressure is not indicative of pulmonary hypertension, and crossing a critically stenotic conduit may be both difficult and lead to further reduction in pulmonary blood flow or hemodynamic compromise. Given the higher risk of thrombosis, patients with Fontan conduits should not have an indwelling central venous or pulmonary artery catheter placed that remains in the Fontan conduit; if one is left in situ, one should strongly consider systemic anticoagulation [16]. Given the importance of maintaining adequate preload in the Fontan circulation, a simple central venous catheter that terminates in the SVC may be considered for a short period of time when large fluid shifts are expected, such as during a large-volume paracentesis or aggressive diuresis [17]. If needed, right heart catheterization should be fluoroscopically guided with removal of the catheter at the conclusion of the procedure.
Cardiopulmonary Resuscitation
Special note should be paid to the challenges in performing CPR in patients with Fontan circulations. In these patients, due to the lack of a sub-pulmonic ventricle, during chest compression, blood can flow backward in the Fontan conduit, limiting the effectiveness of CPR. This often leads to inadequate pulmonary blood flow during chest compressions, leading to decreased oxygenation and preload to the systemic ventricle, and subsequently decreased cardiac output and end-organ perfusion. Central venous pressure rises significantly, worsening cerebrovascular congestion and increasing the risk of neurological injury. These considerations do not mean that CPR should not be performed or shortened in these patients, but rather that the transition from CPR to emergent mechanical support may need to be expedited. Patients with dextrocardia may also have a more rightward point of optimal chest compressions and defibrillation than those with levocardia [18].
Pulmonary Disease and Mechanical Ventilatory Support
ACHD patients often have underlying pulmonary disease, such as restrictive lung disease from multiple prior cardiac surgeries or cardiomegaly, diaphragmatic paralysis due to phrenic nerve injury, and airway disease from multiple intubations [19]. Additionally, pulmonary hypertension can be present in up to one-third of patients with ACHD. Due to low pulmonary reserve, concomitant pulmonary hypertension, and alterations in pulmonary vascular blood flow, ACHD patients are often uniquely susceptible to pulmonary insults [20]. In patients with Fontan conduits dependent on passive blood flow through the pulmonary vascular bed, conditions in which pulmonary vascular resistance acutely rises can lead to a dramatic drop in preload of the single ventricle and subsequent hemodynamic collapse [21, 22]. This includes pneumonia, pulmonary embolism, pneumothorax, and excessive positive end-expiratory pressure (PEEP) in the setting of mechanical ventilation. Diagnosis of pulmonary embolism can be particularly nuanced in Fontan patients, as differential distribution of contrast through the Fontan and Glenn conduits can lead to false positive diagnosis; this can be ameliorated by dual contrast injections via the upper and lower limbs or by protocoling the imaging to allow adequate contrast circulation for complete opacification through the pulmonary vasculature. At times invasive pulmonary angiography is indicated to definitively diagnose and potentially intervene in pulmonary emboli [23].
Tailoring oxygenation support can be challenging in ACHD patients with cyanosis or residual shunts, as a peripheral oxygenation saturation of less than 90% may represent their baseline. Worsening oxygen saturation below baseline, worsening respiratory rate, or lactic acidosis can all signal relative hypoxemia necessitating supplemental oxygenation. Conversely, intensivists should recognize that targeting a “normal” oxygenation in these patients before de-escalating support is detrimental and should instead individualize O2 goals to the individual patient.
Just as the number of ACHD patients admitted to the ICU has increased over recent years, so, too, has the number of ACHD patients requiring mechanical ventilation [24]. Intubation can have severe detrimental hemodynamic effects on congenital anatomies; an acute drop in preload associated with induction can cause hemodynamic collapse in patients with Fontan circulation. Excessive PEEP, which reduces preload and increases afterload, can worsen failing sub-pulmonic ventricles in the setting of pulmonary hypertension or Tetralogy of Fallot (ToF). The increase in pulmonary afterload from mechanical ventilation could acutely worsen an intra-atrial right to left shunt, causing profound hypoxia, which in turn can further exacerbate pulmonary vascular constriction [25]. Conversely, the decrease in LV afterload and preload associated with PEEP can be beneficial in patients with predominantly systemic ventricular failure. Consequently, intubation of ACHD patients should be performed by providers familiar with congenital anatomy and cardiac anesthesia. Interestingly, one single-center study showed that ACHD patients have a relatively low incidence of difficult endotracheal intubation when compared to non-ACHD patients, possibly due to a different age and weight profile compared to the general population [26] .
Hepatic Disease
Patients with congenital heart disease often have comorbid liver dysfunction due to venous congestion, decreased cardiac output, hypoxemia, or ischemic injury to the hepatic parenchyma. This is especially common in patients with right-sided lesions (such as ToF or Ebstein anomaly), or in single ventricle physiology palliated with Fontan circulation [27]. For patients who underwent surgery before 1992, viral hepatitis infection from a blood transfusion should also be considered an etiology of liver disease [28]. As ACHD patients age and develop, the comorbidities of adulthood, cirrhosis due to alcohol use, or non-alcoholic fatty liver disease has also been observed in this population. Regardless of the etiology, patients with ACHD and liver disease suffer from coagulopathies and aberrant hemodynamics that can further complicate their care in the ICU. Fontan-associated liver disease can be particularly challenging to recognize, as these patients do not exhibit the elevation in transaminases or transhepatic gradient seen in other forms of liver disease [29]. However, the presence of FALD can often complicate an advanced therapy evaluation for a critically ill Fontan patient, and candidacy for both liver and heart transplantation would need to be evaluated [30]. Another consideration in critically ill patients with failing Fontan physiology is severe protein-calorie malnutrition secondary to protein losing enteropathy (PLE), characterized by hypoalbuminemia, enteric protein loss, diarrhea, and edema. Several pathophysiological mechanisms have been proposed to explain this phenomenon, including chronic inflammation and chronic central venous congestion. It is associated with significant morbidity and mortality in this population, and is an indication for transplant evaluation.
Renal Disease
Chronic kidney disease is common in the ACHD population and is associated with an increased risk of adverse outcomes [31]. This is especially true in ACHD patients with cyanosis, as more than 65% of these patients have some degree or renal dysfunction [32]. Quantification of glomerular filtration rate should ideally be done using a cystatin C–based method, as this has been shown to more accurately predict clinical events than creatinine-based methods in ACHD patients [33]. Management of renal dysfunction and acute kidney injury is largely similar in ACHD patients to that in non-ACHD cardiac patients, on optimizing pre-load and perfusion, decreasing renovascular congestion, and if needed, initiation of continuous renal replacement therapy. Notably, patients with a single ventricle physiology often do not tolerate the large volume shifts associated with hemodialysis, complicating the transition from continuous to intermittent dialysis.
Hematological Disease
ACHD patients are uniquely prone to both clotting and hemorrhagic complications, depending on their underlying anatomy. Patients with cyanotic heart disease and Eisenmenger syndrome exhibit secondary erythrocytosis, platelet dysfunction, decreased fibrinogen, hemostatic abnormalities, and endothelial dysfunction. This constellation of risk factors uniquely predispose Eisenmenger patients to both spontaneous bleeding events (the most dire being hemoptysis and intrapulmonary hemorrhage) and thromboembolic events, which can lead to cerebrovascular injury due to right to left shunting [34]. Therapeutic phlebotomy should only be pursued in the presence of severe hyper-viscosity symptoms (such as acute thrombosis and neurological injury) despite adequate hydration. Fontan patients are also at increased risk of thrombus formation due to sluggish circulation throughout the passive sub-pulmonic conduit; this can lead not only to Fontan failure but also paradoxical emboli and stroke with residual fenestrations or venovenous collaterals.
Acute blood loss anemia in patients with baseline erythrocytosis can also be difficult to recognize, as a significant drop in hemoglobin or hematocrit could still fall in the “normal” lab range. Screening for iron deficiency and repleting iron stores improves oxygen-carrying capacity. Assessing for changes in the hemodynamics or end-organ perfusion can help guide resuscitation with blood products in these patients.
Primary Cardiac Disease
Arrhythmia
Both tachyarrhythmia and bradyarrhythmia are commonly encountered in the ACHD population and can often lead to ICU admission. Intra-atrial reentry tachycardia (IART), in which the scarred atria promote the development of macro re-entry pathways independent of the cavo-tricuspid isthmus, is the most commonly encountered atrial arrhythmia in ACHD patients (though atrial fibrillation and typical flutter are also common) [35]. Atrioventricular reentrant tachycardia and Wolff-Parkinson-White syndrome should also be considered in patients with Ebstein anomaly, Ebstein-like tricuspid valves, or congenitally corrected transposition of the great arteries (ccTGA) ebstinoid valves [36]. As the loss of AV synchrony and the atrial kick can cause hemodynamic collapse in an already tenuous congenital anatomy (such as cyanotic disease or single ventricle physiology), atrial arrhythmias should be treated expeditiously with a rhythm control strategy (either medically or through electrical cardioversion). Notably, CHA2DS2-VASc scores do not accurately predict the risk of thromboembolism in ACHD patients, and ACHD patients with atrial arrhythmia are typically anticoagulated [37]. Ventricular tachycardias are commonly seen in patients with ToF, either due to underlying myopathic processes or isthmus defined by surgical scar and patch material. While ToF patients may have implanted cardiac defibrillators (ICDs), they also have a high burden of inappropriate shocks due to atrial arrhythmias [38]. A careful device interrogation should be performed before incorrectly diagnosing such a patient with electrical storm. In the setting of incessant tachyarrhythmia refractory to medical therapy, catheter-based ablation procedures can be considered; these should be performed by electrophysiologists with expertise in congenital anatomy.
Bradyarrhythmias in congenital heart disease can be categorized into congenital abnormalities of the conduction system, acquired bradyarrhythmias following surgical or percutaneous intervention, or mixed causes [39]. Patients with ccTGA are at high risk of progressive heart block due to anatomic distortion of the conduction system, with mean age of heart block occurrence of 18 years old. Additionally, many surgical repairs of CHD can lead to sinus node dysfunction, including atrial switch procedures in D-transposition of the great arteries (i.e., Mustard and Senning surgeries) and repair of sinus venosus ASDs. Infrequently, transcatheter membranous VSD device closure can lead to heart block. Depending on the presence of a sub-pulmonic ventricle and adequate venous access, placement of an emergent temporary transvenous pacemaker may not be possible in the ICU setting (though emergent placement of a transvenous pacemaker in a Fontan baffle has been reported) [40]. In these cases, pharmacologic methods to increase chronotropy and even transcutaneous pacing may need to be pursued to bridge the patient to definitive surgical epicardial pacemaker placement.
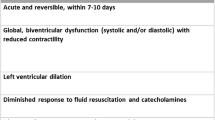
Heart Failure
Acute decompensated heart failure (ADHF) is a leading cause of death in ACHD patients and represents a significant burden of ACHD ICU admissions [7•, 41]. Early stages of decompensation can sometimes be difficult to identify in ACHD patients who have lived with a limited functional capacity since childhood; consequently some patients may not present to care until they are in extremis. Medical heart failure therapy in a biventricular circulation with a morphological systemic left ventricle does not differ much from that in the acquired heart failure population. Guideline-directed medical therapy (including beta blockers, ACEi/ARB/ARNI, SGLT2 inhibitors, and mineralocorticoid antagonists) should be pursued [42•]. However, patients with single ventricle physiology and systemic right ventricles may not respond the same to heart failure medications and there has been inconclusive evidence of benefit.
When assessing the ACHD patient in ADHF, identifying potentially correctible lesions can be crucial in guiding care and delaying the need for advanced therapies; these include pulmonary valve regurgitation in tetralogy of fallot, baffle obstruction or leak in d-TGA with atrial switch, systemic tricuspid valve regurgitation in ccTGA and patients with Norwood corrections, and Fontan conduit obstructions [13, 43]. Transcatheter interventions can sometimes correct these lesions, and reverse the underlying shock state [44, 45]. As ACHD patients age and accrue risk factors for atherosclerosis, acute coronary syndromes should also be considered correctable triggers for ADHF in the ACHD population [46, 47]. Anomalous coronary arteries, myocardial bridges, and coronary compression from an aneurysmal pulmonary artery or oversized prosthetic pulmonary valve can also lead to myocardial ischemia and, ultimately, shock in certain ACHD patients [48, 49].
Advanced heart failure is a common end point in patients with an underlying myopathic process, such as those with systemic right ventricles, severe pulmonary hypertension with failure of the sub-pulmonic ventricle, tetralogy of fallot, and single-ventricle physiologies with Fontan palliation. As with acute decompensated heart failure-cardiogenic shock (ADHF-CS) in the non-ACHD population, initial medical therapy focuses on optimizing volume status and supporting blood pressure. In right heart failure lesions, attention should be made to maintain adequate preload without over-distending a failing RV, as well as reducing the RV afterload with PVR reduction and maintaining adequate SVR for renal perfusion. In Fontan circulations, a higher central venous pressure should be targeted as filling of the single ventricle is particularly preload sensitive [50]. Vasoactive medications should be selected based on the underlying hemodynamic profile and insult; norepinephrine or epinephrine is generally a reasonable starting choice; however, both can increase PVR and promote arrhythmias. Vasopressin could be considered in patients with pulmonary hypertension given selective effects on peripheral vasoconstriction without significantly affecting PVR [51]. In select patients with single-ventricle physiology, a combination of an inotropic agent (such as milrinone or dobutamine) to improve single-ventricular function plus a pulmonary vasodilator (such as inhaled nitric oxide, iloprost, or epoprostenol) to improve flow through the “bottle neck” of the pulmonary vascular bed can improve cardiac output. While potentially effective, consideration should be made to hypotension with this combination.
In patients with worsening ADHF-CS refractory to medical therapy, temporary mechanical circulatory support (tMCS) should be considered. From 2004–2014, the use of tMCS in ACHD patients has increased by over 250%; however, this has not been accompanied by improved in-hospital mortality, which can be as high as 58–60% [52]. When deploying tMCS in ACHD patients, determining which ventricles need to be supported and the vascular access for delivering the chosen devices are both key considerations. As these patients have often undergone several vascular access procedures throughout their lifetimes, scarring around access sites, or chronic occlusions of vessels, can complicate deployment of tMCS. Univentricular systemic ventricle support devices (such as the intra-aortic balloon pump or impella percutaneous ventricular assist device) have both been deployed in patients with congenital heart disease [53,54,55]. The use of right (or sub-pulmonic) ventricular support devices is still growing in the general ICU population, though it may have particular utility in the ACHD population that often suffers from sub-pulmonic ventricular failure [56,57,58]. In situations where biventricular support and oxygenation support is needed, veno-arterial extracorporeal membrane oxygenation (VA-ECMO) should be considered. One retrospective study showed that patients with ACHD who required ECMO had longer lengths of stay and suffered more complications than those without ACHD [59]. When deploying VA-ECMO, reviewing the congenital anatomy to understand aortic and cavo-atrial connections is key to ensuring that arterial and venous cannula are well positioned. Patients with a Fontan undergoing peripheral VA-ECMO cannulation require drainage cannulae in both the SVC and IVC (VVA-ECMO) [60]. However, this approach may lead to stasis in the Fontan conduit. Another potential strategy is a VAV configuration with oxygenated blood return to the upper part of the body, ensuring adequate oxygenation and promoting more flow in the Fontan conduit.
Prior to deploying tMCS in all critically ill ACHD patients, a potential exit strategy should be identified. This can include bridge to intervention (in the setting of a potentially reversible valvular or coronary insults), bridge to recovery (in the setting of decompensated heart failure expected to improve with medical therapies), or bridge to durable mechanical support or transplant.
Advanced Heart Failure Therapies
The decision to pursue advanced heart failure therapies (such as durable mechanical circulatory support or organ transplant) in the critically ill ACHD patient should be made in with the multidisciplinary input of specialists in congenital heart disease, critical care, advanced heart failure, and congenital cardiac surgery. Patients with CHD can be disadvantaged by the United Network for Organ Sharing (UNOS) heart transplant allocation criteria, and on average stay longer on the transplant waitlist and experience higher waitlist mortality [61,62,63]. Notably since the 2018 UNOS allocation revision for transplantation, there has been an increase in the use of tMCS to shorten the wait time for organ transplant. Durable mechanical support, in the form of a durable ventricular assist device (VAD) or total artificial heart (TAH), can be considered an exit strategy from temporary mechanical support [64]. Again, device choice is determined by the underlying anatomy and physiology. VADs have been implanted to support systemic right ventricles, though this often requires an adequately RV volume, the resection of trabeculae, and alternative positioning of the inflow cannula [65]. VADs have also been implanted to support those with Fontan palliations, both as a bridge to transplant and as a destination therapy [66]. A study of the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) showed that ACHD patients with LVADs have similar survival to non-ACHD patients. In contrast, those with TAH or biventricular assist devices had worse outcomes [67]. Cavo-pulmonary assist devices specifically designed for Fontan circulations are currently under development, though they are currently in the in-vitro and in-vivo model phase [68].
The long heart transplant waitlist times for ACHD patients are multifactorial, including high rates of sensitizations from prior surgeries and blood transfusions and lower urgency listings. [69] In order to prioritize ACHD patients, UNOS has published guidance on exception requests for ACHD patients [70]. While ACHD patients who undergo heart transplant have twice the 30-day mortality of non-ACHD patients, the patients who survive past one year have superior survival to non-ACHD patients [71, 72•].
Neuropsychiatric Considerations
ACHD patients are at high risk of neuropsychiatric pathology that is often exacerbated in the critical care setting [73]. Both structural neurologic disease (such as prior stroke and frontal lobe injury) and psychiatric disease (such as depression and anxiety) have been observed at high rates in this population [74]. This can complicate sedation in the context of mechanical ventilation as well as complex goals of care decision-making. Involving a patient’s family and support system can be beneficial in these settings. Importantly, ACHD patients are also at risk of acute neurological insult due to increased risk of stroke and systemic thromboembolism [75]. This is particularly true in patients with right to left shunts and in cyanotics; in these patients, the use of bubble filters on peripheral IVs can mitigate the risk of paradoxical embolism.
Conclusions
The care of the critically ill adult congenital heart disease patient is complex and requires the input of a multidisciplinary team. As this population continues to grow and age, it is incumbent on intensivists to recognize the unique challenges in caring for this population, and work with congenital heart disease specialists to support these patients through critical illness.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Moons P, Bovijn L, Budts W, Belmans A, Gewillig M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation. 2010;122(22):2264–72. https://doi.org/10.1161/CIRCULATIONAHA.110.946343.
Gilboa SM, Salemi JL, Nembhard WN, Fixler DE, Correa A. Mortality resulting from congenital heart disease among children and adults in the United States, 1999 to 2006. Circulation. 2010;122(22):2254–63. https://doi.org/10.1161/CIRCULATIONAHA.110.947002.
Van Der Bom T, Bouma BJ, Meijboom FJ, Zwinderman AH, Mulder BJM. The prevalence of adult congenital heart disease, results from a systematic review and evidence based calculation. Am Heart J. 2012;164(4):568–75. https://doi.org/10.1016/j.ahj.2012.07.023.
Gilboa SM, Devine OJ, Kucik JE, et al. Congenital heart defects in the United States: estimating the magnitude of the affected population in 2010. Circulation. 2016;134(2):101–9. https://doi.org/10.1161/CIRCULATIONAHA.115.019307.
Allan CK. Intensive care of the adult patient with congenital heart disease. Prog Cardiovasc Dis. 2011;53(4):274–80. https://doi.org/10.1016/j.pcad.2010.11.002.
Keane RR, Kendersky P, Park JG, et al. Characteristics and outcomes of adults with congenital heart disease in the cardiac intensive care unit: insights from the critical care cardiology trials network registry. J Am Coll Cardiol. 2022;79(9):1389. https://doi.org/10.1016/S0735-1097(22)02380-4.
• Ramlakhan KP, Van Der Bie M, Den Uil CA, Dubois EA, Roos-Hesselink JW. Adult patients with congenital heart disease in the intensive care unit. Heart. 2022;108(18):1452–60. https://doi.org/10.1136/heartjnl-2021-320676. Findings from this study show that the most common reason for ACHD patients to be admitted to the ICU are arrhythmia, hemorrhage, heart failure, and pulmonary disease.
Saidi AS, Paolillo J, Fricker FJ, Sears SF, Kovacs AH. Biomedical and psychosocial evaluation of “cured” adults with congenital heart disease. Congenit Heart Dis. 2007;2(1):44–54. https://doi.org/10.1111/j.1747-0803.2007.00071.x.
Stout KK, Daniels CJ, Aboulhosn JA, et al. AHA/ACC guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018. https://doi.org/10.1161/CIR.0000000000000603.
Baumgartner H, De Backer J, Babu-Narayan SV, et al. 2020 ESC guidelines for the management of adult congenital heart disease. Eur Heart J. 2021;42(6):563–645. https://doi.org/10.1093/eurheartj/ehaa554.
Mylotte D, Pilote L, Ionescu-Ittu R, et al. Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation. 2014;129(18):1804–12. https://doi.org/10.1161/CIRCULATIONAHA.113.005817.
Ochiai R, Kato H, Akiyama N, et al. Nationwide survey of the transfer of adults with congenital heart disease from pediatric cardiology departments to adult congenital heart disease centers in Japan. Circ J. 2016;80(5):1242–50. https://doi.org/10.1253/circj.CJ-15-0937.
Buber J, Valle C, Valente AM. Common congenital heart problems in acute and intensive care. Eur Heart J Acute Cardiovasc Care. 2023;12(4):267–79. https://doi.org/10.1093/ehjacc/zuad030.
Petrov V, Fedoryshyn I, Tsvigun H. Peculiarities of the arm blood flow after classical Blalock taussig shunt clinical case description. Exp Clin Physiol Biochem. 2017;78(2):50–5. https://doi.org/10.25040/ecpb2017.02.050.
Kadosh BS, Berg DD, Bohula EA, et al. Pulmonary artery catheter use and mortality in the cardiac intensive care unit. JACC Heart Fail. 2023;11(8):903–14. https://doi.org/10.1016/j.jchf.2023.04.007.
Kaipa S, Mastropietro CW, Bhai H, Lutfi R, Friedman ML, Yabrodi M. Upper body peripherally inserted central catheter in pediatric single ventricle patients. World J Cardiol. 2020;12(10):484–91. https://doi.org/10.4330/wjc.v12.i10.484.
Rajpal S, Opotowsky AR, Rutherford A, Wu F. Hemodynamic effects of paracentesis in a patient with a Fontan circulation. World J Pediatr Congenit Heart Surg. 2019;10(3):357–9. https://doi.org/10.1177/2150135118779351.
Marino BS, Tabbutt S, MacLaren G, et al. Cardiopulmonary resuscitation in infants and children with cardiac disease: a scientific statement from the American Heart Association. Circulation. 2018. https://doi.org/10.1161/CIR.0000000000000524.
Lui GK, Saidi A, Bhatt AB, et al. Diagnosis and management of noncardiac complications in adults with congenital heart disease a scientific statement from the American Heart Association. Circulation. 2017. https://doi.org/10.1161/CIR.0000000000000535.
Kratzert WB, Boyd EK, Schwarzenberger JC. Management of the critically ill adult with congenital heart disease. J Cardiothorac Vasc Anesth. 2018;32(4):1682–700. https://doi.org/10.1053/j.jvca.2017.11.025.
Dasi LP, KrishnankuttyRema R, Kitajima HD, et al. Fontan hemodynamics: Importance of pulmonary artery diameter. J Thorac Cardiovasc Surg. 2009;137(3):560–4. https://doi.org/10.1016/j.jtcvs.2008.04.036.
Gewillig M, Brown SC, Eyskens B, et al. The Fontan circulation: who controls cardiac output? Interact Cardiovasc Thorac Surg. 2010;10(3):428–33. https://doi.org/10.1510/icvts.2009.218594.
Torok RD, Fleming GA, Hill KD. Transcatheter pulmonary embolectomy after fontan: Fontan transcatheter pulmonary embolectomy. Catheter Cardiovasc Interv. 2016;87(5):939–44. https://doi.org/10.1002/ccd.26096.
Ho K, Bare I, Sy E, Singh J, Opotowsky AR, Dehghani P. Trends in patient characteristic, cost, and mortality among mechanically ventilated adult patients with congenital heart disease in the United States. CJC Open. 2022;4(2):197–205. https://doi.org/10.1016/j.cjco.2021.09.024.
Chimot L, Mascle S, Chabanne C, et al. Acute severe hypoxaemia after mechanical ventilation in a patient with an Ebstein anomaly requiring extracorporeal membrane oxygenation. Br J Anaesth. 2011;107(6):1010–2. https://doi.org/10.1093/bja/aer360.
Siddiqui ZA, Chandrakantan A, Hills EE, Nguyen CN, Todd BM, Adler AC. Incidence of difficult laryngoscopy in adult congenital heart disease patients: a retrospective cohort study. J Cardiothorac Vasc Anesth. 2021;35(12):3659–64. https://doi.org/10.1053/j.jvca.2021.07.018.
Reiter FP, Hadjamu NJ, Nagdyman N, et al. Congenital heart disease-associated liver disease: a narrative review. Cardiovasc Diagn Ther. 2021;11(2):577–90. https://doi.org/10.21037/cdt-20-595.
Wang A, Book WM, McConnell M, Lyle T, Rodby K, Mahle WT. Prevalence of hepatitis C infection in adult patients who underwent congenital heart surgery prior to screening in 1992. Am J Cardiol. 2007;100(8):1307–9. https://doi.org/10.1016/j.amjcard.2007.05.059.
Emamaullee J, Zaidi AN, Schiano T, et al. Fontan-associated liver disease: screening, management, and transplant considerations. Circulation. 2020;142(6):591–604. https://doi.org/10.1161/CIRCULATIONAHA.120.045597.
Reardon LC, DePasquale EC, Tarabay J, et al. Heart and heart-liver transplantation in adults with failing Fontan physiology. Clin Transplant. 2018;32(8): e13329. https://doi.org/10.1111/ctr.13329.
Krishnathasan K, Dimopoulos K, Duncan N, et al. Advanced heart failure in adult congenital heart disease: the role of renal dysfunction in management and outcomes. Eur J Prev Cardiol. 2023. https://doi.org/10.1093/eurjpc/zwad094.
Dimopoulos K, Diller GP, Koltsida E, et al. Prevalence, predictors, and prognostic value of renal dysfunction in adults with congenital heart disease. Circulation. 2008;117(18):2320–8. https://doi.org/10.1161/CIRCULATIONAHA.107.734921.
Opotowsky AR, Carazo M, Singh MN, et al. Creatinine versus cystatin C to estimate glomerular filtration rate in adults with congenital heart disease: results of the Boston Adult Congenital Heart Disease Biobank. Am Heart J. 2019;214:142–55. https://doi.org/10.1016/j.ahj.2019.04.018.
Arvanitaki A, Gatzoulis MA, Opotowsky AR, et al. Eisenmenger syndrome. J Am Coll Cardiol. 2022;79(12):1183–98. https://doi.org/10.1016/j.jacc.2022.01.022.
Karbassi A, Nair K, Harris L, Wald RM, Roche SL. Atrial tachyarrhythmia in adult congenital heart disease. World J Cardiol. 2017;9(6):496. https://doi.org/10.4330/wjc.v9.i6.496.
Fuchs MM, Connolly HM. Ebstein anomaly in the adult patient. Cardiol Clin. 2020;38(3):353–63. https://doi.org/10.1016/j.ccl.2020.04.004.
Khairy P, Aboulhosn J, Broberg CS, et al. Thromboprophylaxis for atrial arrhythmias in congenital heart disease: a multicenter study. Int J Cardiol. 2016;223:729–35. https://doi.org/10.1016/j.ijcard.2016.08.223.
Goldenthal I, Rosenbaum MS, Lewis M, Sciacca RR, Garan H, Biviano AB. Inappropriate implantable cardioverter-defibrillator shocks in repaired tetralogy of fallot patients: prevalence and electrophysiological mechanisms. IJC Heart Vasc. 2020. https://doi.org/10.1016/j.ijcha.2020.100543.
Carlson SK, Patel AR, Chang PM. Bradyarrhythmias in congenital heart disease. Card Electrophysiol Clin. 2017;9(2):177–87. https://doi.org/10.1016/j.ccep.2017.02.002.
Tankut S, Yoruk A, Vinocur J. Emergency temporary transbaffle pacing for complete heart block after Fontan palliation. J Am Coll Cardiol. 2020;75(11):2843. https://doi.org/10.1016/S0735-1097(20)33470-7.
Verheugt CL, Uiterwaal CSPM, Van Der Velde ET, et al. Mortality in adult congenital heart disease. Eur Heart J. 2010;31(10):1220–9. https://doi.org/10.1093/eurheartj/ehq032.
• Egbe AC, Miranda WR, Pellikka PA, DeSimone CV, Connolly HM. Prevalence and prognostic implications of left ventricular systolic dysfunction in adults with congenital heart disease. J Am Coll Cardiol. 2022;79(14):1356–65. https://doi.org/10.1016/j.jacc.2022.01.040. Findings from this study showed that left ventricular systolic dysfunction is associated with major adverse cardiovascular events in ACHD patients.
Saef JM, Ghobrial J. Valvular heart disease in congenital heart disease: a narrative review. Cardiovasc Diagn Ther. 2021;11(3):818–39. https://doi.org/10.21037/cdt-19-693-b.
Sabbak N, Ghobrial J. Case report: successful emergent transcatheter pulmonary valve replacement within failing pulmonary artery conduit in the setting of cardiogenic shock with extracorporeal membrane oxygenation support. Al-Hijji M, Sinning C, Javier Olsen F, Tardo D, Ahmed N, eds. Eur Heart J Case Rep. 2021. https://doi.org/10.1093/ehjcr/ytab301
Tan W, Stefanescu Schmidt AC, Horlick E, Aboulhosn J. Transcatheter interventions in patients with adult congenital heart disease. J Soc Cardiovasc Angiogr Interv. 2022;1(6): 100438. https://doi.org/10.1016/j.jscai.2022.100438.
Lui GK, Rogers IS, Ding VY, et al. Risk estimates for atherosclerotic cardiovascular disease in adults with congenital heart disease. Am J Cardiol. 2017;119(1):112–8. https://doi.org/10.1016/j.amjcard.2016.09.023.
Tutarel O, Kempny A, Alonso-Gonzalez R, et al. Congenital heart disease beyond the age of 60: emergence of a new population with high resource utilization, high morbidity, and high mortality. Eur Heart J. 2014;35(11):725–32. https://doi.org/10.1093/eurheartj/eht257.
Jiang MX, Brinza EK, Ghobrial J, et al. Coronary artery disease in adults with anomalous aortic origin of a coronary artery. JTCVS Open. 2022;10:205–21. https://doi.org/10.1016/j.xjon.2022.04.022.
Molossi S, Doan T, Sachdeva S. Anomalous coronary arteries. Cardiol Clin. 2023;41(1):51–69. https://doi.org/10.1016/j.ccl.2022.08.005.
Rychik J, Atz AM, Celermajer DS, et al. Evaluation and management of the child and adult with Fontan circulation: a scientific statement from the American Heart Association. Circulation. 2019. https://doi.org/10.1161/CIR.0000000000000696.
Smith AM. The role of vasopressin in cardiorespiratory arrest and pulmonary hypertension. QJM. 2006;99(3):127–33. https://doi.org/10.1093/qjmed/hcl009.
Nguyen VP, Dolgner S, Stout KK. National trends in the use of temporary mechanical circulatory support in patients with adult congenital heart disease. J Am Coll Cardiol. 2020;75(11):578. https://doi.org/10.1016/S0735-1097(20)31205-5.
Chowdhury UK, Kothari SS, Subramaniam GK. Intra-aortic balloon counterpulsation in a patient with the failing Fontan circulation. Cardiol Young. 2007;17(01):102. https://doi.org/10.1017/S1047951106001235.
Moran AM, Blume ED, Quinn R. Intra-aortic balloon pump use in the failing Fontan circulation: intra-aortic balloon pump use in Fontan circulation. Congenit Heart Dis. 2008;3(1):60–2. https://doi.org/10.1111/j.1747-0803.2007.00143.x.
Morray BH, Dimas VV, Lim S, et al. Circulatory support using the impella device in fontan patients with systemic ventricular dysfunction: a multicenter experience. Catheter Cardiovasc Interv. 2017;90(1):118–23. https://doi.org/10.1002/ccd.26885.
Cabezón G, Stephanenko A, Redondo A, Amat-Santos IJ. Impella RP in Ebstein disease as a bridge to heart transplant. JACC Cardiovasc Interv. 2021;14(6):e57–60. https://doi.org/10.1016/j.jcin.2020.12.013.
García Gómez M, Uribarri A, San Román Calvar JA, Stepanenko A. Clinical use of percutaneous mechanical circulatory assistance in a patient with end-stage right-sided heart failure and massive tricuspid insufficiency due to congenital heart disease: first-in-the-world case report. Hassan M, Ahmed AS, Dimitriadis K, Simovic S, Guella E, eds. Eur Heart J - Case Rep. 2021;5(8). https://doi.org/10.1093/ehjcr/ytab269
Vijayakumar N, Badheka A, Chegondi M, Mclennan D. Successful use of Protek Duo cannula to provide veno-venous extra-corporeal membrane oxygenation and right ventricular support for acute respiratory distress syndrome in an adolescent with complex congenital heart disease. Perfusion. 2021;36(2):200–3. https://doi.org/10.1177/0267659120923880.
Kops SA, White SC, Klewer SE, Andrews JG, Seckeler MD. ECMO in adults with congenital heart disease - analysis of a national discharge database. Int J Cardiol Congenit Heart Dis. 2022;8: 100366. https://doi.org/10.1016/j.ijcchd.2022.100366.
Bacon MK, Gray SB, Schwartz SM, Cooper DS. Extracorporeal membrane oxygenation (ECMO) support in special patient populations—the bidirectional Glenn and Fontan circulations. Front Pediatr. 2018;6:299. https://doi.org/10.3389/fped.2018.00299.
Parker WF, Chung K, Anderson AS, Siegler M, Huang ES, Churpek MM. Practice changes at U.S. transplant centers after the new adult heart allocation policy. J Am Coll Cardiol. 2020;75(23):2906–16. https://doi.org/10.1016/j.jacc.2020.01.066.
Alshawabkeh LI, Hu N, Carter KD, et al. Wait-list outcomes for adults with congenital heart disease listed for heart transplantation in the US. J Am Coll Cardiol. 2016;68(9):908–17. https://doi.org/10.1016/j.jacc.2016.05.082.
Karamlou T, Hirsch J, Welke K, et al. A United Network for Organ Sharing analysis of heart transplantation in adults with congenital heart disease: outcomes and factors associated with mortality and retransplantation. J Thorac Cardiovasc Surg. 2010;140(1):161–8. https://doi.org/10.1016/j.jtcvs.2010.03.036.
Saef J, Montgomery R, Cedars A, et al. Durable mechanical circulatory support in adult congenital heart disease: reviewing clinical considerations and experience. J Clin Med. 2022;11(11):3200. https://doi.org/10.3390/jcm11113200.
Brida M, Diller GP, Gatzoulis MA. Systemic right ventricle in adults with congenital heart disease: anatomic and phenotypic spectrum and current approach to management. Circulation. 2018;137(5):508–18. https://doi.org/10.1161/CIRCULATIONAHA.117.031544.
Cedars A, Kutty S, Danford D, et al. Systemic ventricular assist device support in Fontan patients: A report by ACTION. J Heart Lung Transplant. 2021;40(5):368–76. https://doi.org/10.1016/j.healun.2021.01.011.
VanderPluym CJ, Cedars A, Eghtesady P, et al. Outcomes following implantation of mechanical circulatory support in adults with congenital heart disease: an analysis of the Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS). J Heart Lung Transplant. 2018;37(1):89–99. https://doi.org/10.1016/j.healun.2017.03.005.
Escher A, Strauch C, Hubmann EJ, et al. A cavopulmonary assist device for long-term therapy of fontan patients. Semin Thorac Cardiovasc Surg. 2022;34(1):238–48. https://doi.org/10.1053/j.semtcvs.2021.06.016.
Davies RR, Russo MJ, Yang J, Quaegebeur JM, Mosca RS, Chen JM. Listing and transplanting adults with congenital heart disease. Circulation. 2011;123(7):759–67. https://doi.org/10.1161/CIRCULATIONAHA.110.960260.
OPTN/UNOS. Review board guidance for adult congenital heart disease exception requests. https://optn.transplant.hrsa.gov/media/2349/thoracic_guidance_201712.pdf. Accessed Mar 2021.
Shah DK, Deo SV, Althouse AD, et al. Perioperative mortality is the Achilles heel for cardiac transplantation in adults with congenital heart disease: evidence from analysis of the UNOS registry. J Card Surg. 2016;31(12):755–64. https://doi.org/10.1111/jocs.12857.
• Riggs KW, Zafar F, Radzi Y, Yu PJ, Bryant R, Morales DLS. Adult congenital heart disease: current early expectations after cardiac transplantation. Ann Thorac Surg. 2020;109(2):480–6. https://doi.org/10.1016/j.athoracsur.2019.06.067. Findings from this study show that ACHD patients who undergo heart transplant and survive past one year have superior survival to non-ACHD patients.
Ilardi D, Ono KE, McCartney R, Book W, Stringer AY. Neurocognitive functioning in adults with congenital heart disease:Ilardi et al. Congenit Heart Dis. 2017;12(2):166–73. https://doi.org/10.1111/chd.12434.
Mercado AE, Well A, Lamari-Fisher A, et al. Mental health diagnoses in hospitalized adults with congenital heart disease in the state of Texas: a 10-year review. Int J Cardiol Congenit Heart Dis. 2022;7: 100340. https://doi.org/10.1016/j.ijcchd.2022.100340.
Prokšelj K. Stroke and systemic embolism in adult congenital heart disease. Int J Cardiol Congenit Heart Dis. 2023;12:100453. https://doi.org/10.1016/j.ijcchd.2023.100453.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Das, T., Rampersad, P. & Ghobrial, J. Caring for the Critically Ill Adult Congenital Heart Disease Patient. Curr Cardiol Rep 26, 283–291 (2024). https://doi.org/10.1007/s11886-024-02034-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11886-024-02034-5