Abstract
Purpose of Review
Recent large clinical trials have failed to show that triglyceride-rich lipoprotein-lowering therapies decrease the risk of atherosclerotic cardiovascular disease (ASCVD). In this review, we reconcile these findings with evidence showing that elevated levels of triglyceride-rich lipoproteins and the cholesterol they contain, remnant cholesterol, cause ASCVD alongside low-density lipoprotein (LDL) cholesterol.
Recent Findings
Results from observational epidemiology, genetic epidemiology, and randomized controlled trials indicate that lowering of remnant cholesterol and LDL cholesterol decrease ASCVD risk by a similar magnitude per 1 mmol/L (39 mg/dL) lower non-high-density lipoprotein cholesterol (remnant cholesterol+LDL cholesterol). Indeed, recent guidelines for ASCVD prevention recommend the use of non-high-density lipoprotein cholesterol instead of LDL cholesterol.
Summary
Current consensus is moving towards recognizing remnant cholesterol and LDL cholesterols as equals per 1 mmol/L (39 mg/dL) higher levels in the risk assessment of ASCVD; hence, triglyceride-rich lipoprotein-lowering therapies should also lower levels of non-HDL cholesterol to reduce ASCVD risk.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010.
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P, et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395:795–808. https://doi.org/10.1016/S0140-6736(19)32008-2.
Boren J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2020;41:2313–30. https://doi.org/10.1093/eurheartj/ehz962.
Nordestgaard BG. Triglyceride-rich lipoproteins and atherosclerotic cardiovascular disease: new insights from epidemiology, genetics, and biology. Circ Res. 2016;118:547–63. https://doi.org/10.1161/CIRCRESAHA.115.306249.
•• Nicholls SJ, Lincoff AM, Garcia M, Bash D, Ballantyne CM, Barter PJ, et al. Effect of high-dose omega-3 fatty acids vs corn oil on major adverse cardiovascular events in patients at high cardiovascular risk: the STRENGTH randomized clinical trial. JAMA. 2020;324:2268–80. https://doi.org/10.1001/jama.2020.22258. A large randomized controlled trial showing that treatment with high-dose omega-3 fatty acids did not decrease incidence of cardiovascular events compared to placebo.
Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380:11–22. https://doi.org/10.1056/NEJMoa1812792.
•• Das Pradhan A, Glynn RJ, Fruchart JC, MacFadyen JG, Zaharris ES, Everett BM, et al. Triglyceride lowering with pemafibrate to reduce cardiovascular risk. N Engl J Med. 2022;387:1923–34. https://doi.org/10.1056/NEJMoa2210645. A large randomized controlled trial showing that treatment with a new fibrate did not decrease incidence of cardiovascular events compared to placebo.
Sabatine MS, Giugliano RP, Keech AC, Honarpour N, Wiviott SD, Murphy SA, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713–22. https://doi.org/10.1056/NEJMoa1615664.
Schwartz GG, Steg PG, Szarek M, Bhatt DL, Bittner VA, Diaz R, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097–107. https://doi.org/10.1056/NEJMoa1801174.
Nordestgaard BG, Tybjaerg-Hansen A, Lewis B. Influx in vivo of low density, intermediate density, and very low density lipoproteins into aortic intimas of genetically hyperlipidemic rabbits. Roles of plasma concentrations, extent of aortic lesion, and lipoprotein particle size as determinants. Arterioscler Thromb. 1992;12:6–18. https://doi.org/10.1161/01.atv.12.1.6.
Nordestgaard BG, Wootton R, Lewis B. Selective retention of VLDL, IDL, and LDL in the arterial intima of genetically hyperlipidemic rabbits in vivo. Arterioscler Thromb Vasc Biol. 1995;15:534–42. https://doi.org/10.1161/01.ATV.15.4.534.
Stender S, Zilversmit DB. Transfer of plasma lipoprotein components and of plasma proteins into aortas of cholesterol-fed rabbits. Molecular size as a determinant of plasma lipoprotein influx. Arteriosclerosis. 1981;1:38–49. https://doi.org/10.1161/01.atv.1.1.38.
Nordestgaard BG, Tybjaerg-Hansen A. IDL, VLDL, chylomicrons and atherosclerosis. Eur J Epidemiol. 1992;8(Suppl 1):92–8. https://doi.org/10.1007/BF00145358.
Castaner O, Pinto X, Subirana I, Amor AJ, Ros E, Hernaez A, et al. Remnant cholesterol, not LDL cholesterol, is associated with incident cardiovascular disease. J Am Coll Cardiol. 2020;76:2712–24. https://doi.org/10.1016/j.jacc.2020.10.008.
Varbo A, Nordestgaard BG. Remnant cholesterol and risk of ischemic stroke in 112,512 individuals from the general population. Ann Neurol. 2019;85:550–9. https://doi.org/10.1002/ana.25432.
Wadstrom BN, Wulff AB, Pedersen KM, Jensen GB, Nordestgaard BG. Elevated remnant cholesterol increases the risk of peripheral artery disease, myocardial infarction, and ischaemic stroke: a cohort-based study. Eur Heart J. 2022;43:3258–69. https://doi.org/10.1093/eurheartj/ehab705.
• Varbo A, Nordestgaard BG. Directly measured vs. calculated remnant cholesterol identifies additional overlooked individuals in the general population at higher risk of myocardial infarction. Eur Heart J. 2021;00 https://doi.org/10.1093/eurheartj/ehab293. A cohort study showing that the association between elevated remnant cholesterol and increased risk of myocardial infarction is explained by measured remnant choelsterol rather than remnant cholesterol calculated from plasma triglycerides.
Duran EK, Aday AW, Cook NR, Buring JE, Ridker PM, Pradhan AD. Triglyceride-rich lipoprotein cholesterol, small dense ldl cholesterol, and incident cardiovascular disease. J Am Coll Cardiol. 2020;75:2122–35. https://doi.org/10.1016/j.jacc.2020.02.059.
Balling M, Afzal S, Varbo A, Langsted A, Davey Smith G, Nordestgaard BG. VLDL Cholesterol accounts for one-half of the risk of myocardial infarction associated with apoB-containing lipoproteins. J Am Coll Cardiol. 2020;76:2725–35. https://doi.org/10.1016/j.jacc.2020.09.610.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Martin SS, Blaha MJ, Elshazly MB, Toth PP, Kwiterovich PO, Blumenthal RS, et al. Comparison of a novel method vs the Friedewald equation for estimating low-density lipoprotein cholesterol levels from the standard lipid profile. JAMA. 2013;310:2061–8. https://doi.org/10.1001/jama.2013.280532.
•• Sampson M, Ling C, Sun Q, Harb R, Ashmaig M, Warnick R, et al. A new equation for calculation of low-density lipoprotein cholesterol in patients with normolipidemia and/or hypertriglyceridemia. JAMA Cardiol. 2020;5:540–8. https://doi.org/10.1001/jamacardio.2020.0013. A new easily implementable equation outperforms the Friedewald equation for calculation of LDL cholesterol in individuals with low non-HDL cholesterol and/or high plasma triglycerides.
• Doi T, Langsted A, Nordestgaard BG. Elevated remnant cholesterol reclassifies risk of ischemic heart disease and myocardial infarction. J Am Coll Cardiol. 2022;79:2383–97. https://doi.org/10.1016/j.jacc.2022.03.384. Remnant cholesterol improves risk classification when added to a model of conventional risk factors.
Pedersen SB, Langsted A, Nordestgaard BG. Nonfasting mild-to-moderate hypertriglyceridemia and risk of acute pancreatitis. JAMA Intern Med. 2016;176:1834–42. https://doi.org/10.1001/jamainternmed.2016.6875.
Hansen SEJ, Madsen CM, Varbo A, Nordestgaard BG. Body mass index, triglycerides, and risk of acute pancreatitis: a population-based study of 118 000 individuals. J Clin Endocrinol Metab. 2020:105. https://doi.org/10.1210/clinem/dgz059.
Yang AL, McNabb-Baltar J. Hypertriglyceridemia and acute pancreatitis. Pancreatology. 2020;20:795–800. https://doi.org/10.1016/j.pan.2020.06.005.
Kawano Y, Cohen DE. Mechanisms of hepatic triglyceride accumulation in non-alcoholic fatty liver disease. J Gastroenterol. 2013;48:434–41. https://doi.org/10.1007/s00535-013-0758-5.
Hansen SEJ, Varbo A, Nordestgaard BG, Langsted A. Hypertriglyceridemia-associated pancreatitis: new concepts and potential mechanisms. Clin Chem. 2023; https://doi.org/10.1093/clinchem/hvad094.
Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32:1–22. https://doi.org/10.1093/ije/dyg070.
Davies NM, Holmes MV, Davey SG. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601. https://doi.org/10.1136/bmj.k601.
Jørgensen AB, Frikke-Schmidt R, West AS, Grande P, Nordestgaard BG, Tybjærg-Hansen A. Genetically elevated non-fasting triglycerides and calculated remnant cholesterol as causal risk factors for myocardial infarction. Eur Heart J. 2013;34:1826–33. https://doi.org/10.1093/eurheartj/ehs431.
Kaltoft M, Langsted A, Nordestgaard BG. Triglycerides and remnant cholesterol associated with risk of aortic valve stenosis: Mendelian randomization in the Copenhagen General Population Study. Eur Heart J. 2020;41:2288–99. https://doi.org/10.1093/eurheartj/ehaa172.
Varbo A, Benn M, Tybjaerg-Hansen A, Jorgensen AB, Frikke-Schmidt R, Nordestgaard BG. Remnant cholesterol as a causal risk factor for ischemic heart disease. J Am Coll Cardiol. 2013;61:427–36. https://doi.org/10.1016/j.jacc.2012.08.1026.
Varbo A, Benn M, Tybjaerg-Hansen A, Nordestgaard BG. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation. 2013;128:1298–309. https://doi.org/10.1161/CIRCULATIONAHA.113.003008.
• Wang Q, Oliver-Williams C, Raitakari OT, Viikari J, Lehtimaki T, Kahonen M, et al. Metabolic profiling of angiopoietin-like protein 3 and 4 inhibition: a drug-target Mendelian randomization analysis. Eur Heart J. 2021;42:1160–9. https://doi.org/10.1093/eurheartj/ehaa972. Curiously, different drug targets for triglyceride-lowering have differential associations with metabolic profiles and risk of ischemic heart disease per 1 mmol/L (39 mg/dL) plasma triglyceride-lowering in the UK Biobank.
Tikkanen E, Minicocci I, Hallfors J, Di Costanzo A, D'Erasmo L, Poggiogalle E, et al. Metabolomic signature of angiopoietin-like protein 3 deficiency in fasting and postprandial state. Arterioscler Thromb Vasc Biol. 2019;39:665–74. https://doi.org/10.1161/ATVBAHA.118.312021.
• Richardson TG, Leyden GM, Wang Q, Bell JA, Elsworth B, Davey Smith G, et al. Characterising metabolomic signatures of lipid-modifying therapies through drug target mendelian randomisation. PLoS Biol. 2022;20:e3001547. https://doi.org/10.1371/journal.pbio.3001547. A second study to confirm that different triglyceride-lowering drug targets have differential associations with metabolic profiles and risk of ischemic heart disease per 1 mmol/L (39 mg/dL) plasma triglyceride-lowering in the UK Biobank.
Ference BA, Kastelein JJP, Ray KK, Ginsberg HN, Chapman MJ, Packard CJ, et al. Association of triglyceride-lowering LPL variants and LDL-C-lowering LDLR variants with risk of coronary heart disease. JAMA. 2019;321:364–73. https://doi.org/10.1001/jama.2018.20045.
Richardson TG, Sanderson E, Palmer TM, Ala-Korpela M, Ference BA, Davey Smith G, et al. Evaluating the relationship between circulating lipoprotein lipids and apolipoproteins with risk of coronary heart disease: a multivariable Mendelian randomisation analysis. PLoS Med. 2020;17:e1003062. https://doi.org/10.1371/journal.pmed.1003062.
• Bjornson E, Adiels M, Taskinen MR, Burgess S, Rawshani A, Boren J, et al. Triglyceride-rich lipoprotein remnants, low-density lipoproteins, and risk of coronary heart disease: a UK Biobank study. Eur Heart J. 2023; https://doi.org/10.1093/eurheartj/ehad337. Another curious finding from the UK Biobank that genetic variants associated with a relatively larger increase in levels of triglyceride-rich lipoproteins than levels of LDL are associated with a higher increased risk of coronary heart disease per 1 mg/dL increase in apolipoprotein B or 1 mmol/L (39 mg/dL) increase in the cholesterol content of apolipoprotein B containing lipoproteins.
Tybjaerg-Hansen A, Nordestgaard BG, Christoffersen M. Triglyceride-rich remnant lipoproteins are more atherogenic than LDL per particle: is this important? Eur Heart J. 2023; https://doi.org/10.1093/eurheartj/ehad419.
Prohaska TA, Alexander VJ, Karwatowska-Prokopczuk E, Tami J, Xia S, Witztum JL, et al. APOC3 inhibition with volanesorsen reduces hepatic steatosis in patients with severe hypertriglyceridemia. J Clin Lipidol. 2023;17:406–11. https://doi.org/10.1016/j.jacl.2023.04.007.
Kersten S. Angiopoietin-like 3 in lipoprotein metabolism. Nat Rev Endocrinol. 2017;13:731–9. https://doi.org/10.1038/nrendo.2017.119.
• Li Z, Zhang B, Liu Q, Tao Z, Ding L, Guo B, et al. Genetic association of lipids and lipid-lowering drug target genes with non-alcoholic fatty liver disease. EBioMedicine. 2023;90:104543. https://doi.org/10.1016/j.ebiom.2023.104543. Genetic variants close to the LPL locus are associated with non-alcoholic fatty liver disease risk, while genetic variants close to other genes involved in triglyceride-rich lipoprotein metabolism are not.
Duell PB, Welty FK, Miller M, Chait A, Hammond G, Ahmad Z, et al. Nonalcoholic fatty liver disease and cardiovascular risk: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2022;42:e168–e85. https://doi.org/10.1161/ATV.0000000000000153.
Marston NA, Giugliano RP, Im K, Silverman MG, O'Donoghue ML, Wiviott SD, et al. Association between triglyceride lowering and reduction of cardiovascular risk across multiple lipid-lowering therapeutic classes: a systematic review and meta-regression analysis of randomized controlled trials. Circulation. 2019;140:1308–17. https://doi.org/10.1161/CIRCULATIONAHA.119.041998.
• Doi T, Langsted A, Nordestgaard BG. A possible explanation for the contrasting results of REDUCE-IT vs. STRENGTH: cohort study mimicking trial designs. Eur Heart J. 2021;42:4807–17. https://doi.org/10.1093/eurheartj/ehab555. Different placebos may explain part of why treatment with omega-3 fatty acids led to decreased incidence of cardiovascular disease in the REDUCE-IT trial but not in the STRENGTH trial.
Ostadal P, Steg PG, Poulouin Y, Bhatt DL, Bittner VA, Chua T, et al. Metabolic risk factors and effect of alirocumab on cardiovascular events after acute coronary syndrome: a post-hoc analysis of the ODYSSEY OUTCOMES randomised controlled trial. Lancet Diabetes Endocrinol. 2022;10:330–40. https://doi.org/10.1016/S2213-8587(22)00043-2.
Koren MJ, Kereiakes D, Pourfarzib R, Winegar D, Banerjee P, Hamon S, et al. Effect of PCSK9 inhibition by alirocumab on lipoprotein particle concentrations determined by nuclear magnetic resonance spectroscopy. J Am Heart Assoc. 2015:4. https://doi.org/10.1161/JAHA.115.002224.
Sliz E, Kettunen J, Holmes MV, Williams CO, Boachie C, Wang Q, et al. Metabolomic consequences of genetic inhibition of PCSK9 compared with statin treatment. Circulation. 2018;138:2499–512. https://doi.org/10.1161/CIRCULATIONAHA.118.034942.
Hilvo M, Simolin H, Metso J, Ruuth M, Oorni K, Jauhiainen M, et al. PCSK9 inhibition alters the lipidome of plasma and lipoprotein fractions. Atherosclerosis. 2018;269:159–65. https://doi.org/10.1016/j.atherosclerosis.2018.01.004.
Toth PP, Hamon SC, Jones SR, Martin SS, Joshi PH, Kulkarni KR, et al. Effect of alirocumab on specific lipoprotein non-high-density lipoprotein cholesterol and subfractions as measured by the vertical auto profile method: analysis of 3 randomized trials versus placebo. Lipids Health Dis. 2016;15:28. https://doi.org/10.1186/s12944-016-0197-4.
Ahmad Z, Banerjee P, Hamon S, Chan KC, Bouzelmat A, Sasiela WJ, et al. Inhibition of angiopoietin-like protein 3 with a monoclonal antibody reduces triglycerides in hypertriglyceridemia. Circulation. 2019;140:470–86. https://doi.org/10.1161/CIRCULATIONAHA.118.039107.
Ference BA, Ray KK, Catapano AL, Ference TB, Burgess S, Neff DR, et al. Mendelian randomization study of ACLY and cardiovascular disease. N Engl J Med. 2019;380:1033–42. https://doi.org/10.1056/NEJMoa1806747.
Witztum JL, Gaudet D, Freedman SD, Alexander VJ, Digenio A, Williams KR, et al. Volanesorsen and triglyceride levels in familial chylomicronemia syndrome. N Engl J Med. 2019;381:531–42. https://doi.org/10.1056/NEJMoa1715944.
• Tardif JC, Karwatowska-Prokopczuk E, Amour ES, Ballantyne CM, Shapiro MD, Moriarty PM, et al. Apolipoprotein C-III reduction in subjects with moderate hypertriglyceridaemia and at high cardiovascular risk. Eur Heart J. 2022;43:1401–12. https://doi.org/10.1093/eurheartj/ehab820. Novel drugs silencing the APOC3 gene, now being tested in clinical trials, offer a stronger triglyceride-lowering effect compared to previous drugs.
Preiss D, Tikkanen MJ, Welsh P, Ford I, Lovato LC, Elam MB, et al. Lipid-modifying therapies and risk of pancreatitis: a meta-analysis. JAMA. 2012;308:804–11. https://doi.org/10.1001/jama.2012.8439.
Gaudet D, Alexander VJ, Baker BF, Brisson D, Tremblay K, Singleton W, et al. Antisense inhibition of apolipoprotein C-III in patients with hypertriglyceridemia. N Engl J Med. 2015;373:438–47. https://doi.org/10.1056/NEJMoa1400283.
Gouni-Berthold I, Alexander VJ, Yang Q, Hurh E, Steinhagen-Thiessen E, Moriarty PM, et al. Efficacy and safety of volanesorsen in patients with multifactorial chylomicronaemia (COMPASS): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Diabetes Endocrinol. 2021;9:264–75. https://doi.org/10.1016/S2213-8587(21)00046-2.
Jones A, Peers K, Wierzbicki AS, Ramachandran R, Mansfield M, Dawson C, et al. Long-term effects of volanesorsen on triglycerides and pancreatitis in patients with familial chylomicronaemia syndrome (FCS) in the UK Early Access to Medicines Scheme (EAMS). Atherosclerosis. 2023;375:67–74. https://doi.org/10.1016/j.atherosclerosis.2023.05.008.
Hegele RA. APOC3 Interference for familial chylomicronaemia syndrome. touchREV. Endocrinol. 2022;18:82–3. https://doi.org/10.17925/EE.2022.18.2.82.
Digenio A, Dunbar RL, Alexander VJ, Hompesch M, Morrow L, Lee RG, et al. Antisense-mediated lowering of plasma apolipoprotein C-III by volanesorsen improves dyslipidemia and insulin sensitivity in type 2 diabetes. Diabetes Care. 2016;39:1408–15. https://doi.org/10.2337/dc16-0126.
Nakajima A, Eguchi Y, Yoneda M, Imajo K, Tamaki N, Suganami H, et al. Randomised clinical trial: pemafibrate, a novel selective peroxisome proliferator-activated receptor alpha modulator (SPPARMalpha), versus placebo in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 2021;54:1263–77. https://doi.org/10.1111/apt.16596.
• Francque SM, Bedossa P, Ratziu V, Anstee QM, Bugianesi E, Sanyal AJ, et al. A randomized, controlled trial of the Pan-PPAR Agonist Lanifibranor in NASH. N Engl J Med. 2021;385:1547–58. https://doi.org/10.1056/NEJMoa2036205. A new fibrate shows promising results in the treatment of non-alcoholic steatohepatitis.
Dufour JF, Anstee QM, Bugianesi E, Harrison S, Loomba R, Paradis V, et al. Current therapies and new developments in NASH. Gut. 2022;71:2123–34. https://doi.org/10.1136/gutjnl-2021-326874.
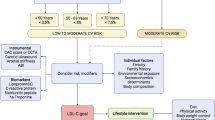
• Pearson GJ, Thanassoulis G, Anderson TJ, Barry AR, Couture P, Dayan N, et al. Canadian Cardiovascular Society Guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in adults. Can J Cardiol. 2021;37:1129–50. https://doi.org/10.1016/j.cjca.2021.03.016. The new Canadian dyslipidemia guidelines recommend the use of non-HDL cholesterol and apolipoprotein B as primary treatment targets alongside, or instead of, LDL cholesterol.
Wadstrom BN, Pedersen KM, Wulff AB, Nordestgaard BG. Elevated remnant cholesterol, plasma triglycerides, and cardiovascular and non-cardiovascular mortality. Eur Heart J. 2023;44:1432–45. https://doi.org/10.1093/eurheartj/ehac822.
• Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2019;41:111–88. https://doi.org/10.1093/eurheartj/ehz455. The latest European dyslipidemia guidelines recommend use of non-HDL cholesterol and apolipoprotein B as secondary targets in all individuals after LDL cholesterol goals have been met.
Acknowledgements
We thank the staff and participants from the Copenhagen General Population Study for their valuable contributions.
Employment
Recent, present, and anticipated employment is The Capital Region (Danish: Region Hovedstaden) in Denmark for all authors, all paid through tax-generated money without any influence from private companies.
Funding
Independent Research Fund Denmark (grant 1030-00168B), Novo Nordisk Foundation (grant NNF21OC0071977), Johan and Lise Boserup Fund, Aase and Ejnar Danielsen Fund, and Herlev and Gentofte Hospital provided funding. The funders had no role in the design of the study or in the collection, analysis, interpretation of data, writing the manuscript, or the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
BNW performed literature search and wrote the first draft of the manuscript. ABW, KMP, and BGN revised the manuscript for critical scientific content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
BGN reports consultancies and talks sponsored by AstraZeneca, Sanofi, Regeneron, Akcea, Ionis, Amgen, Kowa, Denka, Amarin, Novartis, Novo Nordisk, Esperion, Abbott, Silence Therapeutics, and Mankind. BNW, ABW, and KMP do not have any financial competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wadström, B.N., Wulff, A.B., Pedersen, K.M. et al. Do Triglyceride-Rich Lipoproteins Equal Low-Density Lipoproteins in Risk of ASCVD?. Curr Atheroscler Rep 25, 795–803 (2023). https://doi.org/10.1007/s11883-023-01153-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-023-01153-8