Abstract
There is only limited scientific evidence with varying results on the association between hospital admissions and low ambient temperatures. Furthermore, there has been no research in Northern Europe on cold-associated morbidity. Therefore, this study investigated the associations of daily wintertime temperature and cold spells with cardiorespiratory hospital admissions in the Helsinki metropolitan area, Finland. Daily number of non-elective hospital admissions for 2001–2017 was obtained from the national hospital discharge register and meteorological data from the Finnish Meteorological Institute. Quasi-Poisson regression models were fitted, controlling for potential confounders such as time trend, weekday, holidays, air pollution, barometric pressure, and influenza. The associations of cold season daily mean ambient temperature and cold spells with hospital admissions were estimated using a penalized distributed lag linear models with 21 lag days. Decreased wintertime ambient temperature was associated with an increased risk of hospitalization for myocardial infarction in the whole population (relative risk [RR] per 1 °C decrease in temperature: 1.017, 95% confidence interval [CI]: 1.002–1.032). An increased risk of hospital admission for respiratory diseases (RR: 1.012, 95% CI: 1.002, 1.022) and chronic obstructive pulmonary disease (RR: 1.031, 95% CI: 1.006, 1.056) was observed only in the ≥ 75 years age group. There was an independent effect of cold spell days only for asthma admissions (RR: 2.348, 95% CI: 1.026, 5.372) in the all-ages group. Cold temperature increases the need for acute hospital care due to myocardial infarction and respiratory causes during winter in a northern climate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extremes in weather, including air temperature, can have a profound effect on human health. Both low and high temperatures are associated with morbidity and mortality worldwide (Basu and Samet 2002; Ye et al. 2012). The Intergovernmental Panel on Climate Change projects that though the global mean temperature is increasing globally, occasional cold winter extremes will continue to occur in the future (Collins et al. 2013). At the same time, adaptation to warmer climates may turn populations more susceptible to cold extremes (Arbuthnott et al. 2016). Hence, low temperatures will remain a public health threat in susceptible geographic areas. Therefore, it is essential to understand better the association of low temperatures with human health.
Most of the epidemiological research on low temperatures has focused on the mortality effects (Conlon et al. 2011; Song et al. 2017). Scientific evidence on the effects of cold exposure on cardiovascular morbidity is limited and results have been varying. A recent study from Spain found an increased risk of hospitalizations for cardiovascular diseases with cold exposure (Martinez-Solanas and Basagana 2019). However, a meta-analysis reported no clear effects of cold exposure on the risk of cardiovascular or cerebrovascular morbidity (Bunker et al. 2016). Concerning myocardial infarction risk in association with cold, a systematic review reported that 8 out of 12 studies reported an increased risk (Bhaskaran et al. 2009).
Results on the association of cold exposure with respiratory admissions are also scarce and inconsistent. A systematic review found an increased risk for cold-induced respiratory and pneumonia morbidity (Bunker et al. 2016). In a study conducted in Denmark, Wichmann et al. (2011) found an association between low temperature and respiratory admissions only in people above 80 years of age (Wichmann et al. 2011). All in all, given the limited scientific evidence available, there is a need for further research to understand better the effect of low wintertime temperatures on cardiorespiratory morbidity.
Studies on association of cold spells with cardiorespiratory hospital admissions are limited. These studies have reported an increased risk of morbidity during cold spell days in comparison to non-cold spell days. For example, a study from Lithuania found increased risk for acute myocardial infarction during cold spell days (Vaičiulis et al. 2011). Likewise, another study found increased risk of asthma admissions during cold spells in China (Chen et al. 2021). However, to our knowledge, no studies have investigated the association of cold spells with cardiorespiratory hospital admissions in Northern Europe.
Even though ambient temperatures will increase worldwide, the climate in Northern Europe will generally stay cold. Exposure–response functions may vary between more and less cold climatic regions. Studies have reported that most of the temperature-related deaths in Northern European countries, like Sweden and Finland, are due to cold temperatures (Åström et al. 2018; Ruuhela et al. 2018). However, limited knowledge exists on the association of cold temperatures with morbidity in Northern Europe. Thus, the main aim of this study is to investigate the associations of low temperatures and cold spells with cause-specific morbidity in the Helsinki metropolitan area, Finland. Finland is a Nordic country with extremely low wintertime temperatures. Additionally, this study also evaluated difference in the relationship for the older age group (≥ 75 years).
Methodology
Study population and setting
This study investigated the associations of low temperatures and cold spells with cardiorespiratory hospital admissions in the Helsinki metropolitan area, during cold season (October–March), 2001–2017. The Helsinki metropolitan area includes the cities of Helsinki, Vantaa, Espoo, and Kauniainen and has a population size of approximately one million (2001–2017) Key Figures on Population by Area, Information and Year-Tilastokeskuksen Px-Web Tietokannat (n.d.).
Data source
We obtained health data from a national health register having information on daily hospital admissions. Data was coded according to the International Classification of Diseases 10th Revision (World Health Organization 2015). The obtained data contained daily non-elective hospital admissions for all cardiovascular diseases (CVD; ICD-10 codes: I00–I99), all respiratory diseases (J00–J99), myocardial infarction (MI; I21–I22), ischemic heart disease (IHD; I20–I25), cerebrovascular diseases (I60–I61, I63–I64), arrhythmia (I46.0, I46.9, I47–I49), asthma (J45, J46), chronic obstructive pulmonary disease (COPD; J41, J44), and pneumonia (J12–J15, J16.8, J18) for all ages, and stratified by age groups (18–64, 65–74, and ≥ 75). The daily number of cases was low in all age groups except for ≥ 75 years; thus, the focus was on this age group.
Key exposure variables in the study were daily mean temperature and cold spells. There is no standard definition for cold spells, but different combinations of intensity and length have been used previously. In this study, we defined cold spells as periods during which daily mean temperature was lower than 10th or 5th percentile of the temperature distribution (during October–March 2001–2017) for four consecutive days or longer. All the days within a cold spell got the value 1, all other days 0. We obtained the meteorological data from the Finnish Meteorological Institute; a fixed weather station at the Helsinki-Vantaa airport was used to collect the data. Data on nitrogen dioxide (NO2), ozone (O3), inhalable particulate matter (PM10; aerodynamic diameter ≤ 10 μm), and fine particulate matter (PM2.5; aerodynamic diameter ≤ 2.5 μm) was obtained from the Helsinki Region Environmental Services Authority. We calculated daily averages of NO2, PM10, and PM2.5 from hourly data of Kallio urban background station. If there were less than 18 hourly values available per day, the daily average was defined as missing. Information on ozone (O3) was collected by calculating an 8-h moving average from hourly data of the Luukki measurement site (areal background station). For daily pollen count, the University of Turku, Aerobiology Unit, provided the data.
Statistical analyses
We used a quasi-Poisson regression because this type of hospital admissions data is known to lead to problems with overdispersion in data analyses. Distributed lag non-linear models (DLNM) were used to investigate the lagged (delayed) and cumulative lagged effects of (a) daily mean temperature and (b) cold spells on the daily number of hospital admissions in colder months. The DLNM modeling framework can simultaneously depict delayed effects (lags) and non-linear exposure–response dependencies. Based on the definition of a “cross-basis,” a bidimensional space of functions that simultaneously describes the shape of the relationship along the predictor space and lag dimension of its occurrence; this methodology explains the relationship along both dimensions. It is possible to visualize cross-basis as a bi-dimensional space of functions that simultaneously describe the pattern of the relationship along predictor x and its distributed lag effects. The process of selecting a cross-basis entails selecting two sets of basis functions that will be merged to produce the cross-basis functions (Gasparrini et al. 2010).
In the first stage of the analyses, DLNM models with temperature lags up to 21 days were used to investigate the cumulative association of daily mean temperature with hospitalizations. Longer lag period was selected to capture the delayed overall effect of cold exposure, which is line with previous literature (Xie et al. 2013; Zhou et al. 2014). However, we also tested alternative lag periods in the sensitivity analyses. In cross-basis matrix, temperature effect was treated as linear because shape of association was approximately linear between temperature and outcomes. Lagged effects were calculated with penalized thing regression splines having an upper limit of 9 degrees of freedom (df) for basis function. The upper limit of degrees of freedom as well as penalization of spline functions was set to avoid unrealistically detailed lag structure.
In the second stage of the analyses, we investigated the effect of cold spells. The analysis was conducted by separately adding a cross-basis term for cold spells in the DLNM models. Finally, we introduced daily temperature and cold spells together in the same model to estimate the possible added effect of prolonged cold, i.e., whether during cold spells the effect of low temperatures was stronger than during isolated days of cold.
All models were adjusted for potential confounders, i.e., variables that may correlate with both exposure and outcome in time. Time and seasonal trends were controlled using natural cubic splines with six degrees of freedom (df) per year, and indicator terms for the day of the week and holidays. Influenza, air pollutants (NO2, O3, PM10, and PM2.5), relative humidity (RH), and barometric pressure (BP) were introduced as potential confounders (selected a priori) in the models. Influenza was defined as a categorical covariate with three categories: 0–49, 50–149, or 150 + diagnosed influenza cases per week in the study area (week refers to all days of that week). We used 2-day averages (lags 0–1) for air pollutants, relative humidity, and barometric pressure. Thin plate regression splines in the mgcv package were used to check the shape of association for the continuous covariates (Wood 2006). Moreover, models were adjusted for pollen count (a sum of alder, birch, mug wort, and grasses) using an indicator showing the sum of the counts on two days (lags 0 and 1), categorized dichotomously using 100grains/m3 as a cutoff.
For the analyses, we used R studio for statistical computing (version: 3.6.0) with the “mgcv” and “dlnm” packages (Gasparrini et al. 2010; Wood 2006). Effect estimates were reported as risk ratios with 95% confidence intervals. We performed analyses separately for the all-ages and ≥ 75 years age groups.
Sensitivity analyses
In the sensitivity analyses, we changed the lag periods for daily mean temperature. The models were run using both relatively short (14 days) and long (28-day) lag periods. Moreover, we used windchill (the degree of the cold as perceived by the human body, which gets worse by high wind speed) as an exposure indicator to check if it is a better predictor of cold effects than temperature alone. Wind chill was defined using the formula from Osczevski et al. (Osczevski and Bluestein 2005) and modified for Finland’s weather conditions by the Finnish Meteorological Institute as follows:
where T is air temperature in degree Celsius and V is windspeed in m/s.
Results
Tables 1 and 2 show the descriptive statistics for daily hospital admissions, meteorological variables, and air pollutants between 1st October and 31st March in 2001–2017. The maximum number of daily hospital admissions was highest for all respiratory diseases and lowest for COPD, i.e., 92 and 13, respectively. The average daily temperature during the study period was − 1.0 °C. Daily mean concentrations of ozone, PM10, PM2.5, and NO2 were 58.5, 8.3, 13.9, and 23.5 µg/m3, respectively.
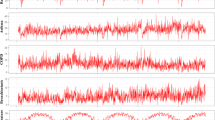
Figure 1a and b show the overall cumulative association of low daily mean temperature with hospital admissions due to cardiorespiratory diseases for a lag period of 21 days. An increased risk of myocardial infarction (RR: 1.017, 95% CI: 1.002, 1.032) was observed among all ages. We also found an increased risk for all respiratory diseases (RR: 1.012, 95% CI: 1.002, 1.022) and COPD (RR: 1.031, 95% CI: 1.006, 1.056) among elderly people, i.e., in the ≥ 75 years age group. These associations were not sensitive to further adjustment for cold spells: confidence intervals got slightly wider, but the effect estimates for daily temperature remained essentially the same (Table S1 in supplements).
The association of cold spell days with cardiorespiratory admissions is shown in Table S2 (supplement attachment). Cold spell days, where the 10th percentile of the temperature distribution was used as a cutoff point, showed no association with cardiorespiratory hospitalizations in the all-ages group. However, an increased risk was found for COPD admissions (RR: 1.569, 95% CI: 1.013, 2.432) in the ≥ 75 years age group.
For the more intense cold spell days, where the 5th percentile (Table S3) of the temperature distribution was used as a cutoff point, we found no positive association for any of the disease categories. However, after adjustment for daily mean temperature, intense cold spells showed an association for asthma admissions in the all-ages group (RR: 2.348, 95% CI: 1.026, 5.372) (Fig. 2a and b).
We tested the robustness of our results by running the sensitivity analyses as described in the “Sensitivity analyses” section. All results remained stable except for the 28-day lag period which showed increased risk for ischemia and myocardial infarction admissions (Table S4 and S5 in supplements).
Discussions
This study examined the associations of daily mean temperature in the cold season and cold spells with cardiorespiratory hospital admissions in the Helsinki metropolitan area, Finland. Low daily mean temperatures were associated with an elevated cumulative risk (over 21 days) for myocardial infarction, all respiratory diseases, and COPD admissions. Cold spells (10th percentile cutoff point) presented an increased risk for COPD admissions, only in the models unadjusted for daily mean temperature. After adjustment for daily mean temperature, intense cold spells (5th percentile cutoff) showed an elevated risk for asthma admissions.
Hospitalizations due to cardiovascular diseases in general showed no association with low winter temperatures or cold spells. Previously, a meta-analysis (including locations such as Italy, California, UK, Brazil, and Hong Kong) restricted to elderly people suggested a reduction in the risk for most CVD morbidity outcomes with decreasing temperature (Bunker et al. 2016). A study in Spain reported that cold exposure increased hospital admissions for cardiovascular diseases in warmer regions but not in colder ones (Martinez-Solanas and Basagana 2019). Findings from studies on cold and mortality also suggest that variation in the effects may be related to differences between geographical areas (Moghadamnia et al. 2017). People and societies in colder climates are already acclimatized to very low wintertime temperatures, and cold countries, such as Finland, have efficient heating systems in private and nursing homes. During extremely cold winter, people may then just stay indoors which would protect especially vulnerable people.
The associations of daily wintertime temperatures with acute exacerbations of cardiovascular diseases may vary depending on the type of cardiovascular disease. Our results showed that lower daily mean temperatures were only associated with an increased risk of myocardial infarction in the all-ages group. These results align with studies from England and Wales and Beijing, China, showing that low temperatures were associated with an increased risk of myocardial infarction morbidity (Bhaskaran et al. 2010; Liu et al. 2018). Our sensitivity analysis indicated a risk not only for myocardial infarction but also for ischemia when lagged effect up to 28 days was considered. Several plausible physiological mechanisms may explain an increased risk of myocardial infarction or ischemic heart disease in general, at low temperatures. Clinical studies have shown that cold exposure increases arterial pressure and blood viscosity (Keatinge et al. 1984), which leads to an additional need for oxygen causing an increase in cardiac workload (Raven et al. 1970) and may lead ischemia and consequently to myocardial infarction.
Our findings also showed an increased risk of respiratory diseases and COPD admissions in the oldest age category (≥ 75 years old) in association with low daily mean temperatures. There are a limited number of studies available on the association of cold with respiratory morbidity. However, a meta-analysis of studies on elderly people also reported that a decrease in daily mean temperature was associated with the risk for respiratory morbidity (Bunker et al. 2016). One plausible explanation for the adverse respiratory effects is that exposure to low temperature can cause bronchoconstriction and congestion of the airways which may lead to exacerbation of respiratory diseases such as COPD (Giesbrecht 1995). This biological mechanism as well as the greater vulnerability of the elderly in general could explain the strong association of low temperature with respiratory morbidity in our study. However, further research is needed to investigate the etiological mechanisms associated with adverse respiratory outcomes in the elderly.
Cold spells did not show an increased risk for any of the diseases except for COPD admission in models unadjusted for daily mean temperature. However, we found an added effect of cold spells only for asthma admissions in the oldest age category (≥ 75 years of age), and only using the stricter criteria (5th percentile cutoff point). Previously, a study from China found no evidence of an added effect of cold spells in relation to respiratory emergency department visits (Song et al. 2018). Similarly, a systematic review of mortality studies also found no additional effect of prolonged exposure to extreme cold temperatures (Ryti et al. 2016). This may suggest that cold days during prolonged cold periods are not generally associated with a greater risk of adverse health effects than isolated cold days. However, there is limited scientific evidence concerning the additional effect of cold spells on different morbidity outcomes which demands further studies in the future.
Finland is a North European country with extremely low wintertime temperatures and the Finnish population has acclimatized to the cold climate. On the other hand, we analyzed effects in the Helsinki region, which is one of the warmest regions in Finland. Nevertheless, our results suggest that low daily mean temperatures during wintertime still pose a threat to the health of the population in the Helsinki region. It is also possible that changing weather conditions in the region are making people more acclimatized to warm weather, resulting in increased vulnerability for cold temperatures.
Our study has several strengths. To the best of our knowledge, this is the first study to investigate the effects of cold on cardiorespiratory hospital admissions in Northern Europe. Long time-series data with practically a hundred percent coverage of hospital admissions was used to provide reliable population-level estimates. Moreover, we investigated associations of temperature with cause-specific diagnosis rather than broad disease categories. The effects of potential confounders, such as influenza and air pollution, were controlled. However, there are some limitations in our study as well. The number of hospital admissions was low in younger age groups. Hence, we were only able to include people older than 75 years in the age-stratified analysis. Furthermore, only cardiovascular and respiratory admissions were considered. There is a need to investigate the effect of exposure to low temperature also on hospital admissions due to other diseases such as diabetes or kidney function.
Conclusion
Low temperatures during cold days are associated with increased morbidity also in a northern climate. Cold days increase the need for acute hospital care due to myocardial infarction and respiratory causes. We did not find any evidence of an added effect of cold spells, except for asthma.
Data Availability
If needed, data and material can be requested from corresponding author.
References
Arbuthnott K, Hajat S, Heaviside C, Vardoulakis S (2016) Changes in population susceptibility to heat and cold over time: assessing adaptation to climate change. Environ Health 15:S33. https://doi.org/10.1186/s12940-016-0102-7
Åström DO, Ebi KL, Vicedo-Cabrera AM, Gasparrini A (2018) Investigating changes in mortality attributable to heat and cold in Stockholm. Sweden Int J Biometeorol 62:1777–1780. https://doi.org/10.1007/s00484-018-1556-9
Basu R, Samet JM (2002) Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev 24:190–202
Bhaskaran K, Hajat S, Haines A, Herrett E, Wilkinson P, Smeeth L (2009) Effects of ambient temperature on the incidence of myocardial infarction. Heart 95:1760–1769
Bhaskaran K, Hajat S, Haines A, Herrett E, Wilkinson P, Smeeth L (2010) Short term effects of temperature on risk of myocardial infarction in England and Wales: time series regression analysis of the Myocardial Ischaemia National Audit Project (MINAP) registry. BMJ 341:3823
Bunker A, Wildenhain J, Vandenbergh A, Henschke N, Rocklöv J, Hajat S et al (2016) Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; a systematic review and meta-analysis of epidemiological evidence. EBioMedicine 6:258–68
Chen Yuxiong, Kong Dehui, Jia Fu, Zhang Yongqiao, Zhao Yakun, Liu Yanbo et al (2021) Increased hospital admissions for asthma from short-term exposure to cold spells in Beijing, China. Int J Hyg Environ Health 238:113839. https://doi.org/10.1016/j.ijheh.2021.113839
Collins M, Knutti R, Arblaster J, Dufresne J-L, Fichefet T, Friedlingstein P, et al (2013) Long-term Climate Change: Projections, Commitments and Irreversibility. In: Climate Change: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Available at: https://www.ipcc.ch/site/assets/uploads/2018/02/WG1AR5_Chapter12_FINAL.pdf
Conlon KC, Rajkovich NB, White-Newsome JL, Larsen L, O’Neill MS (2011) Preventing cold-related morbidity and mortality in a changing climate. Maturitas 69(3):197–202. https://doi.org/10.1016/j.maturitas.2011.04.004
Gasparrini A, Armstrong B, Kenward MG (2010) Distributed lag non-linear models. Stat Med 29:2224–2234
Giesbrecht GG (1995) The respiratory system in a cold environment. Aviat Space Environ Med 66:890–902
Keatinge WR, Coleshaw SR, Cotter F, Mattock M, Chelliah R (1984) Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: factors in mortality from coronary and cerebral thrombosis in winter. BMJ (Clin Res Ed) 289:1405–1408
Key Figures on Population by Area, Information and Year-Tilastokeskuksen Px-Web Tietokannat (n.d.) [(accessed on 3 June 2020)]; Available online: http://pxnet2.stat.fi/PXWeb/pxweb/en/StatFin/StatFin__vrm__vaerak/statfin_vaerak_pxt_11ra.px/
Liu X, Kong D, Fu J, Zhang Y, Liu Y, Zhao Y et al (2018) Association between extreme temperature and acute myocardial infarction hospital admissions in Beijing, China: 2013–2016. PLOS One 13(10):e0204706. https://doi.org/10.1371/journal.pone.0204706
Martinez-Solanas E, Basagana X (2019) Temporal changes in effects of ambient temperatures on hospital admissions in Spain. PLOS ONE 14(6):e0218262. https://doi.org/10.1371/journal.pone.0218262
Moghadamnia MT, Ardalan A, Mesdaghinia A, Keshtkar A, Naddafi K, Yekaninejad MS (2017) Ambient temperature and cardiovascular mortality: a systematic review and meta-analysis. PeerJ 5:e3574. https://doi.org/10.7717/peerj.3574
Osczevski R, Bluestein M (2005) The new windchill equivalent temperature chart. Bull Am Meteorol Soc 86:1453–1458
Raven PB, Niki I, Dahms TE, Horvath SM (1970) Compensatory cardiovascular responses during an environmental cold stress, 5 degrees C. J Appl Physiol 29:417–421
Ruuhela R, Hyvärinen O, Jylhä K, Ruuhela R, Hyvärinen O, Jylhä K (2018) Regional assessment of temperature-related mortality in Finland. Int J Environ Res Public Health 15:406. https://doi.org/10.3390/ijerph15030406
Ryti NR, Guo Y, Jaakkola JK (2016) Global association of cold spells and adverse health effects: a systematic review and meta-analysis. Environ Health Perspect 124:12–22. https://doi.org/10.1289/ehp.1408104
Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y et al (2017) Impact of ambient temperature on morbidity and mortality: an overview of reviews. Sci Total Environ 586:241–254. https://doi.org/10.1016/j.scitotenv.2017.01.212
Song X, Wang S, Li T, Tian J, Ding G, Wang J (2018) The impact of heatwaves and cold spells on respiratory emergency department visits in Beijing. China Sci Total Environ 615:1499–1505. https://doi.org/10.1016/j.scitotenv.2017.09.108
Vaičiulis V, Jaakkola JJK, Radišauskas R, Tamošiūnas A, Lukšienė D, Ryti NRI (2011) Association between winter cold spells and acute myocardial infarction in Lithuania 2000–2015. Sci Rep 11:17062. https://doi.org/10.1038/s41598-021-96366-9
Wichmann J, Andersen Z, Ketzel M, Ellermann T, Loft S (2011) Apparent temperature and cause-specific emergency hospital admissions in Greater Copenhagen. Denmark. PLOS ONE 6(7):e22904. https://doi.org/10.1371/journal.pone.0022904
Wood SN (2006) Low-rank scale-invariant tensor product smooths for generalized additive mixed models. Biometrics 62:1025–1036
World Health Organization (2015) International statistical classification of diseases and related health problems, 10th revision, 5th edn, 2016. World Health Organization. https://apps.who.int/iris/handle/10665/246208
Xie H et al (2013) Short-term effects of the 2008 cold spell on mortality in three subtropical cities in Guangdong Province. China Environ Health Perspect 121:210–216
Ye X, Wolff R, Yu W, Vaneckova P, Pan X, Tong S (2012) Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect 120:19–28. https://doi.org/10.1289/ehp.1003198
Zhou M et al (2014) Health impact of the 2008 cold spell on mortality in subtropical China the climate and health impact national assessment study (CHINAs). Environ Health 13:60
Acknowledgements
The authors are thankful to Finnish Meteorological Institute for providing the weather data, the Aerobiology Unit of the University of Turku for providing the pollen data, and the Helsinki Region Environmental Services Authority HSY for providing the air pollution data.
Funding
This work was supported by intramural funding from University of Eastern Finland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Since this study was a population level study with no personal level data, therefore ethical approval was not required.
Consent for publication
All authors have agreed and given consent for publication of this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Low temperatures during cold days are a serious public health concern in northern climate.
• Individual cold days increase the need for acute hospital care due to myocardial infarction and respiratory causes.
• Cold spells (10th percentile cutoff point) presented an increased risk for COPD admissions.
• No evidence of an added effect of cold spells was found, except for asthma.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sohail, H., Kollanus, V., Tiittanen, P. et al. Low temperature, cold spells, and cardiorespiratory hospital admissions in Helsinki, Finland. Air Qual Atmos Health 16, 213–220 (2023). https://doi.org/10.1007/s11869-022-01259-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-022-01259-z