Abstract
Metformin is the most prescribed oral hypoglycemic drug and is considered by many health practitioners as the first-line treatment for non-insulin-dependent diabetes mellitus (T2DM). It is used either as a monotherapy or adjuvant to other anti-hyperglycemic agents. Most of its side effects are usually mild and self-limiting. However, several studies have shown an association between the use of metformin and low vitamin B12 levels in diabetic patients. The current review aimed to provide a literature review of the current published reports on the association, the possible mechanisms, and the related individualized risk factors that might lead to this incidence. The most accepted mechanism of the effect of metformin on vitamin B12 level is related to the absorption process where metformin antagonism of the calcium cation and interference with the calcium-dependent IF-vitamin B12 complex binding to the ileal cubilin receptor. In addition, many risk factors have been associated with the impact of metformin on vitamin B12 levels in diabetic patients such as dose and duration where longer durations showed a greater prevalence of developing vitamin B12 deficiency. Male patients showed lower levels of vitamin B12 compared to females. Black race showed a lower prevalence of vitamin B12 deficiency in metformin-treated patients. Moreover, chronic diseases including T2DM, hyperlipidemia, coronary artery disease, polycystic ovary disease (PCOD), obesity, and metformin therapy were significantly associated with increased risk of vitamin B12 deficiency.
Graphical abstract
Metformin impacts vitamin B12 by (A) inhibiting calcium-dependent IF-B12 binding. (B) Prolonged use raises deficiency risk. (C) Males have lower B12 levels than females. (D) Black individuals show lower deficiency rates. (E) Conditions like T2DM, hyperlipidemia, coronary artery disease, PCOD, obesity, and metformin use heighten deficiency risk.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is a complex metabolic disorder. The major clinical manifestation is chronic hyperglycemia which results from impaired insulin secretion or/and impaired insulin action. Diabetes mellitus classifications include type 1 insulin-dependent, type 2 insulin-independent, gestational diabetes, and other less common types (e.g., MODY) [1]. In addition, certain criteria for the diagnosis of diabetes mellitus are shown in Table 1 [2]. Generally, type 2 diabetes mellitus (T2DM) is a global health concern that is steadily rising [3]. For instance, an estimated 422 million adults with diabetes worldwide was reported in 2014 [4]. Diabetes prevalence expanded from 4.7% in 1980 to 8.5% in 2014 in adults, with the greatest increase in low and middle-income countries compared to high-income nations [5]. Additionally, 1.1 million children and adolescents aged 14–19 years have T1DM, as estimated by the International Diabetes Federation (IDF), and without interventions to stop the rise in diabetes, by 2045, there will be at least 629 million diabetic patients [6]. Type 2 diabetes mellitus is one of the leading causes of morbidity and mortality worldwide, and it is associated with many systemic vascular complications, which can reduce the quality of life and result in social and economic burdens [7,8,9,10]. Moreover, the financial cost of the healthcare of diabetes mellitus is another economic burden. For. Instance, in many countries, around 5–10% of the healthcare budget is assigned for the treatment of diabetes mellitus [11].
Vitamin B12 deficiency is a significant concern in diabetic patients, particularly those treated with metformin. Several studies have highlighted the association between metformin use and vitamin B12 deficiency in individuals with type 2 diabetes mellitus [13,14,15,16,17,18,19,20,21,22]. The prevalence of vitamin B12 deficiency in diabetic patients on metformin has been reported to be as high as 93% [13]. Furthermore, the impact of vitamin B12 deficiency on peripheral neuropathy in diabetic patients has been a subject of investigation, with studies demonstrating an association between vitamin B12 deficiency and peripheral neuropathy in individuals with type 2 diabetes mellitus [14, 18, 19, 23]. Additionally, the prevalence of vitamin B12 deficiency has been found to be higher in diabetic patients compared to the general population [24]. This deficiency has also been linked to gastroparesis in patients with type 2 diabetes [25]. Moreover, the prevalence of vitamin B12 deficiency has been reported to be higher in individuals with pre-diabetes and diabetes compared to those without these conditions [26]. These findings underscore the importance of routine screening for vitamin B12 deficiency and the potential need for supplementation among diabetic patients, especially those on metformin therapy [27, 28]. In recent years, there has been increasing interest in the association between metformin use and vitamin B12 deficiency in patients with type 2 diabetes mellitus (T2DM)[15, 18]. Several studies have investigated the prevalence of vitamin B12 deficiency and its associated factors among patients with T2DM who are on metformin [20, 29,30,31]. Some studies have indicated a correlation between longer duration of metformin use and increased risk of vitamin B12 deficiency [15, 32, 33]. Additionally, there is evidence suggesting a link between metformin use and diabetic neuropathy [18, 19, 21, 30]. The American Diabetes Association guidelines now recommend routine evaluation for vitamin B12 deficiency in patients taking metformin [19, 29]. It has been suggested that physicians should consider screening for vitamin B12 deficiency in diabetic patients before starting metformin therapy, and periodic monitoring of vitamin B12 levels has been recommended for all patients using metformin, particularly for those using the medication long-term [21, 34]. Moreover, the potential role of vitamin B12 deficiency in exacerbating conditions such as diabetic neuropathy and gastroparesis in patients with T2DM has been highlighted, emphasizing the importance of addressing this issue in clinical management [25]. The research on vitamin B12 deficiency in diabetic patients treated with metformin underscores the need for increased awareness and monitoring of vitamin B12 levels in this patient population. The evidence suggests a potential association between metformin use and vitamin B12 deficiency, with implications for the management of diabetic patients. Hence, this review provides additional insights into the mechanisms underlying this association and guides the development of targeted interventions to mitigate the risk of vitamin B12 deficiency in diabetic patients using metformin.
Methods
We searched Google Scholar and PubMed using the keywords metformin, diabetes, vitamin B12, deficiency, metabolism, mechanism, risk factors, and side effects. We excluded articles that were not related to our research and the ones that did not have sufficient data. In the end, 25 articles were included from the years 2009 to 2021. Out of the 25 articles, 21 showed an association between the use of metformin and vitamin B12 deficiency, while 4 did not. All clinical trials included the use of metformin. However, not always the participants were diabetics. Vitamin B12 deficiency percentage was calculated in some of the studies and others were not. Table 2 summarizes the main data.
Result
Metformin
Metformin belongs to a group of oral hypoglycemic drugs called biguanides. Some aspects of metformin’s mechanism of action are still not fully understood [57]. It is suggested that metformin primarily achieves its glucose-lowering effects through the inhibition of gluconeogenesis in the liver, therefore lowering the production of glucose. Other mechanisms include increased insulin sensitivity [58] and inhibiting lipogenesis [59] as well as increasing the uptake of glucose in the intestine [60] and muscles. In addition, metformin delays gastric emptying which contributes to a decrease in appetite [61]. Figure 1 illustrates metformin’s mechanism of action. A summary of metformin’s mechanism of action is shown in Fig. 1.
Metformin is routinely prescribed to 120 million patients around the world, as it is the first-line treatment for individuals with diabetes mellitus (T2DM) and normal kidney function [62, 63]. It is currently the most prescribed oral anti-diabetic agent and recommended as first-line therapy for type 2 diabetes because of its safety, effectiveness, and possibility for use in combination with other anti-diabetic medications [23]. Both the American Diabetes Association and the European Association for the Study of Diabetes recommend the use of metformin as the first therapeutic choice in the management of type 2 diabetes mellitus (T2DM). Metformin enhances peripheral insulin sensitivity and cardiovascular mortality risk and contributes to weight loss. Medical situations that may require the prescription of metformin, as well as the precautions of its use, are shown in Table 2. The majority of the side effects associated with metformin are mild. One or more episodes of nausea, vomiting, or diarrhea are experienced in 30–45% of patients [64]. Other less common side effects include headache, diaphoresis, weakness, and rhinitis[58].
Vitamin B12
Vitamin B12 also called cobalamin is the largest and most complex vitamin known. It is a water-soluble vitamin with a molecular weight of 1355.4 [65, 66]. It is found mainly in animal sources such as meat, milk, egg, fish, and shellfish, explaining why strict vegetarians are highly prone to developing vitamin B12 deficiency [67]. However, it can also be found in large quantities in some plants like edible algae or blue-green algae [68].
Cobalamin is introduced to the body through the oral cavity, where it binds to its first carrier protein known as transcobalamin I or R-protein. R-protein protects cobalamin from gastric acidity and low pH in the stomach. Gastric parietal cells secret the intrinsic factor IF, the second carrier of cobalamin. In the small intestine, the R-protein is hydrolyzed releasing cobalamin which then binds to intrinsic factors. The cobalamin-IF complex is then absorbed in the distal ileum [65, 69]. An illustration of vitamin B12 metabolism is shown in Fig. 2. There are many ways to diagnose vitamin B12 deficiency such as identification of macrocytic anemia and findings of hyper-segmented (more than 5 lobes) neutrophils on a blood smear. Nevertheless, the most sensitive and diagnostic criteria are low levels of serum cobalamin (< 148 pmol/L)[70]. Mild vitamin B12 deficiency can result in fatigue, weakness, and memory loss. Severe deficiency can result in macrocytic anemia, peripheral neuropathy, and mental psychiatric changes [71,72,73]. The prevalence of deficiency varies by age group. In the US, 3% of those aged 20–39, 4% of those aged 40–59, and 6% of those aged 70 have vitamin B12 deficiency [74]. On the other hand, it is estimated that the subclinical deficiency of vitamin B12 in the US ranges from 10–15% among those > 60 years old to 23–35% in > 80 years old [75]. In Asian and African countries, the prevalence is much higher; for example, in India, 70% of adults are deficient [74].
The deficiency of vitamin B12 can arise from its lack in one’s diet or a defect in gastrointestinal absorption [76]. Some genetic studies reported an association between certain genetic variants and the deficiency of vitamin B12 [77, 78]. Other risk factors that have been suggested to be related to the development of vitamin B12 deficiency include pernicious anemia and the long-term use of certain drugs such as acid-suppressing medications [79] and metformin [52].
Metformin and vitamin B12 deficiency
Metformin-induced vitamin B12 deficiency was reported as early as 1971 when Tomkin et al. recommended that all patients on long-term metformin therapy should be tested for serum B12 deficiency annually [80]. In a randomized placebo-controlled trial, metformin treatment was associated with a mean decrease in vitamin B12 concentration by 19% and an increase in homocysteine concentration by 5% [52]. Former studies have reported that the prevalence of vitamin B12 deficiency among metformin-treated patients varied greatly and ranged between 5.8% and 52% [43, 46,47,48,49, 52, 81,82,83]. A recent meta-analysis that included thirty-one studies reported that patients who received metformin had a significantly higher risk of vitamin B12 deficiency in comparison with diabetic patients not taking metformin, and significantly lower serum vitamin B12 concentrations which depended on dose and duration of treatment [84]. In a retrospective study, it was observed that subjects receiving doses of metformin higher than 2000 mg/day or for more than 4 years had low levels of vitamin B12 [18]. In another review of patients with type 2 diabetes taking metformin after up to 4 months, they showed a decrease in B12 level by 57 pmol/L, which would be predicted to lead to a frank deficiency in a significant proportion of patients based on European data for B12 status [85].
Contrary to the increase in homocysteine levels that is stated above, a cross-sectional study that concluded 1111 patients with type 2 diabetes who took metformin for at least 6 months reported that homocysteine levels were negatively correlated with vitamin B12 levels, and suggested a hypothesis that B12 deficiency due to the use of metformin occurred at the tissue level [40]. While numerous studies reported an association between vitamin B12 deficiency and metformin treatment, in 2017, Rodríguez-Gutiérrez et al., found no variation in vitamin B12 levels between participants receiving metformin and those naive to therapy [53].
Suggested mechanisms
Absorption
Different mechanisms have been suggested clarifying how metformin interposes with vitamin B12 absorption. In 1977, Caspary and Creutzfeldt proposed a mechanism that was how bacterial overgrowth in the intestine resulted in bacterial binding with IF-B12 complex instead of the latter getting absorbed [86]. Another mechanism that was suggested is the alteration of metformin on intestinal motility, thereby reducing the absorption of vitamin B12 [87]. The process of B12-intrinsic factor complex uptake is known to be dependent on calcium availability. Therefore, out of the many mechanisms that were suggested of how metformin interferes with the absorption of vitamin B12, metformin antagonism of the calcium cation and interference with the calcium-dependent IF-vitamin B12 complex binding to the ileal cubilin receptor was the most accepted one. Bauman et al. suggested that the protonated metformin molecule directs itself towards the hydrocarbon core of the ileal cell membrane, displacing the divalent calcium cations by giving a positive charge to the membrane surface. An effect that can be reversed by increasing calcium intake, consequently greatly supporting the mechanism [88].
Dose and duration
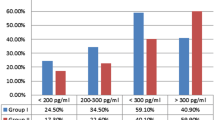
Many studies stated that serum vitamin B12 concentrations are inversely related to long-term therapy and/or higher doses of metformin use [50, 52, 80, 89]. In addition, a meta-analysis of four clinical trials demonstrated that after three to 6 months of metformin use it significantly reduced vitamin B12 levels [85]. Several studies found an association between metformin dose and B12 deficiency, while there was no correlation with its duration. Higher doses of metformin were associated with lower levels of vitamin B12. Hence, it is important to consider metformin dose in recommendations for screening for cobalamin deficiency [19, 35, 40, 43]. Nevertheless, other research demonstrated a relationship between metformin usage, with higher doses, and longer durations, showing a greater prevalence of developing vitamin B12 deficiency [18, 41, 84].
Other risk factors
Alvarez et al. found that male patients had lower levels of vitamin B12 in comparison to females [19]. Black race was found to be a protective factor for vitamin B12 deficiency in metformin-treated patients [14]. A meta-analysis by Niafar et al. found that patients with T2DM, hyperlipidemia, coronary artery disease, polycystic ovary disease (PCOD), or obesity, and on metformin therapy were significantly associated with increased risk of vitamin B12 deficiency and lower serum vitamin B12 concentrations [9]. Increased metformin exposure was hypothesized to be associated with lower levels of B12 and more severe peripheral neuropathy [51]. Impaired vibration sensation and proprioception and paresthesia are unfortunately similar in both diabetic neuropathy and vitamin B12 deficiency [71]. Consequently, it has been suggested that serum B12 levels should be screened routinely in long-term metformin users [82].
In a comparison between T2DM patients having neuropathy, and those who do not, it was found that the first group had higher levels of B12 deficiency than the other group [35]. Moreover, in a dose-dependent manner, both borderline and low levels of vitamin B12 occurred to be associated with the presence of distinct neuropathies and macrocytic anemia [41]. T2DM patients with neuropathy treated with MET 1000 mg/d manifested lower levels of vitamin B12 [35]. Diabetic neuropathy relationship with vitamin B12 deficiency has prominent importance considering vitamin B12 deficiency is profoundly common, especially among patients with diabetic neuropathy. Furthermore, diabetic or pre-diabetic patients diagnosed with diabetic neuropathy may have neuropathy due to vitamin B12 deficiency. Therefore, before initiating the treatment of diabetic neuropathy, the other condition should be excluded [19]. A cross-sectional study stated that patients possibly get diagnosed with diabetic neuropathy instead of vitamin B12 deficiency induced by metformin which leads to neurologic damage with symptoms of peripheral neuropathy [39].
On the other hand, a cross-sectional study by Ahmed et al. found that there was no difference among those with normal and decreased vitamin B12 levels and the presence of neuropathy [14]. Smoking was reported to be associated with lower vitamin B12 levels than in non-smokers (Table 3) [42].
Cognitive impairment
A meta-analysis reported that cognitive impairment prevalence happened to be less significant in people with diabetes treated with metformin. Additionally, six studies showed that dementia incidence also had a reduced risk. Campbell et al. reported that there is no available evidence supporting the use of metformin by non-diabetic individuals in an attempt to prevent dementia. Nevertheless, in patients at risk of developing dementia or Alzheimer’s disease, metformin should continue to be used as first-line therapy for diabetes [90]. A contradicted study, by Moore et al., reported a significant finding of impaired cognitive performance in diabetic patients treated with metformin, which might be alleviated by vitamin B12 and calcium supplements [91].
Multivitamins
Individuals who are receiving supplementation of multivitamins may potentially have protection against B12 deficiency in comparison to those not receiving any [40, 42].
PPIs and/or H2RAs
In consideration of the expanding prevalence of obesity, T2DM, and GORD, there is now more potential for the use of acid-suppressing medications and anti-diabetics concomitantly. Considering that the solitary use of either metformin, PPIs, or H2RAs, has been shown to considerably deplete vitamin B12, co-prescription of metformin with either PPIs or H2RAs can have additional adverse effects on vitamin B12 status [92]. The production of stomach acid by the gastric parietal cells is needed for the conversion of pepsinogen to pepsin, which releases vitamin B12 from ingested proteins. PPIs and H2RAs inhibit this acid production. PPIs block gastric H+K+-ATPase, which is responsible for pumping H+ ions from within gastric parietal cells into the gastric lumen, where they interact with Cl− ions to form HCl. On the other hand, H2RAs inhibit the interaction of histamine with the parietal cell histamine H2 receptor. This blocks the cAMP-dependent pathway that promotes H+K+-ATPase function, thus reducing gastric acid production. A reduction or lack of gastric acid and pepsin diminishes the release of vitamin B12 from food and hence decreases its availability for absorption in the ileum [93]. Long et al. observed that the association of vitamin B12 deficiency along with the concomitant use of metformin and proton pump inhibitors was significantly greater than those on monotherapy. 34.15% of patients with co-prescription were vitamin B12 deficient; in contrast, those on metformin (21.91%) or PPIs (25.58%) monotherapy had lesser deficiency suggesting an additional impact [94]. Nevertheless, there is no clear indication that biochemical or functional vitamin B12 deficiency would occur due to decreased serum vitamin B12 that is caused by these medications, as indicated by circulating homocysteine and methylmalonic acid concentrations, or to the hematologic and neurological manifestations of clinical deficiency [93]. Until other studies are done, Miller recommends those who are co-prescribed to these drugs to observe vitamin B12 status and take vitamin B12 supplements if needed [93]. However, Romero and Lozano found that there was no notable variation in plasma vitamin B12 levels among those receiving and not receiving PPIs [47].
Sulfonylurea and/or insulin
In a cross-sectional study by Kang et al., it was demonstrated that T2DM patients need to monitor their vitamin B12 deficiency and keep an ordinary regulation of their vitamin B12 levels especially those who were prescribed metformin in combination with sulfonylurea. in contrast to insulin metformin and sulfonylurea, co-prescription has been shown to decrease the mean blood vitamin B12 level and the prevalence of vitamin B12 deficiency was significantly increased. Moreover, even after modifications for the daily dosage and duration of metformin among the patients taking the maximal dosage of sulfonylurea, this finding persisted to be significant [83].
Rosiglitazone
In a 6-week study to find the impacts of treatment with metformin or rosiglitazone on serum concentrations of homocysteine, folate, and vitamin B12 in patients with recently diagnosed T2DM where 165 patients have been tested, Sahin et al. observed that metformin use was associated with an increase in homocysteine levels, but vitamin B12 did not vary significantly. Whereas management with rosiglitazone showed a decrease in homocysteine levels, with no significant change in vitamin B1 levels [95].
Conclusion
Until this day, some of the aspects of metformin’s mechanism of action are still not fully understood. We found in our review that there is an undeniable association between the use of metformin and the progression of vitamin B12 deficiency in some diabetic patients. However, the benefits outweigh the risks. When spotted early, vitamin B12 deficiency is easily treated. We recommend further studies to achieve a better understanding of the possible mechanisms, risk factors, and relation of vitamin B12 deficiency to the dose and duration of metformin use. In addition, we advise physicians and health practitioners to always be aware of these side effects. Routine monitoring of vitamin B12 for patients on long-term metformin was also suggested by other studies. These recommendations were associated with higher dosages and longer durations of usage. Some of these studies recommended the regular check for doses ranging more than 1000 to 2000 mg/day, while others did not specify a certain dose or duration. Screening was mostly advised to be annual [14, 18, 19, 36, 39, 41, 43,44,45, 49, 52, 83, 93, 96]. On the contrary, a recommendation for screening by Rodríguez-Gutiérrez et al. could not be made [53].
Data availability
The data that supports the findings in this study are available from the corresponding authors upon reasonable request.
References
Kerner W, Brückel J (2014) Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes 122(07):384–386
A. D. Association (2020) 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes—2020. Diabetes Care 43(Supplement 1):S14–S31
Susan van D et al (2010) The global burden of diabetes and its complications: an emerging pandemic. Eur J Cardiovasc Prev Rehabil 17(1_suppl):s3–s8
W. H. Organization (2019) Classification of diabetes mellitus
W. H. Organization (2016) Global report on diabetes. World Health Organization, Geneva, p 2016
Suvi K et al (2017) IDF diabetes atlas, 8th edn 2017. Brussels, Belgium, International Diabetes Federation
Ahmed MA (2016) Metformin and vitamin B12 deficiency: where do we stand? J Pharm Pharm Sci 19(3):382–398
Rabbia Rana MF, Iftikhar T, Makki MU (2017) Metformin use and vitamin B12 deficiency in patients with type-2 diabetes mellitus. JMH S 11(3):1–3
Niafar M et al (2015) The role of metformin on vitamin B12 deficiency: a meta-analysis review. Intern Emerg Med 10(1):93–102
Alwan A (2011) Global status report on noncommunicable diseases 2010. World Health Organization
Lin Y, Sun Z (2010) Current views on type 2 diabetes. J Endocrinol 204(1):1
Baerlocher MO, Asch M, Myers A (2013) Metformin and intravenous contrast. CMAJ 185(1):E78–E78
Abu Jama’ah WJ et al (2016) Studying the association of metformin dose with peripheral neuropathy in diabetic patients at Jordanian Royal Medical Services. Eur Sci J 12(6)
Ahmed MA, Muntingh G, Rheeder P (2016) Vitamin B12 deficiency in metformin-treated type-2 diabetes patients, prevalence and association with peripheral neuropathy. BMC Pharmacol Toxicol 17(1):44
Koppad AK et al (2017) Evaluation of serum vitamin B12 levels in type 2 diabetes patients on metformin therapy attending a tertiary care hospital. J Evid Based Med Healthc 4(90):5399–5404
Raizada N et al (2017) Serum vitamin B12 levels in type 2 diabetes patients on metformin compared to those never on metformin: a cross-sectional study. Indian J Endocrinol Metab 21(3):424–428
Verma VK et al (2017) Vitamin B12 deficiency among vegetarian and non-vegetarian diabetic population receiving prolonged metformin based oral hypoglycemic agents therapy. Int J Adv Med 4(4)
Alharbi TJ et al (2018) The association of metformin use with vitamin B12 deficiency and peripheral neuropathy in Saudi individuals with type 2 diabetes mellitus. PLoS ONE 13(10):e0204420
Alvarez M et al (2019) Vitamin B12 deficiency and diabetic neuropathy in patients taking metformin: a cross-sectional study. Endocr Connect 8(10):1324–1329
Al Saeed RR, Baraja MA (2021) Vitamin B12 deficiency in patients with type 2 diabetes mellitus using metformin and the associated factors in Saudi Arabia. Saudi Med J 42(2):161–165
Khan TU, Arshad R, Adhami SUZ (2021) Prevalence of vitamin B12 deficiency in type II diabetic patients using metformin. Prof Med J 28(09):1322–1325
Malla D et al (2021) Prevalence of vitamin B12 deficiency in patients with type II diabetes mellitus on metformin. J Diabetes Endocrinol Assoc Nepal 5(1):39–43
Bell DS (2010) Metformin-induced vitamin B12 deficiency presenting as a peripheral neuropathy. South Med J 103(3):265–267
Satyanarayana A et al (2011) Status of B-vitamins and homocysteine in diabetic retinopathy: association with vitamin-B12 deficiency and hyperhomocysteinemia. PLoS ONE 6(11):e26747
Ahmed SS et al (2023) Is vitamin B12 deficiency a risk factor for gastroparesis in patients with type 2 diabetes? Diabetol Metab Syndr 15(1):33
Singla R et al (2019) Vitamin B12 deficiency is endemic in Indian population: a perspective from North India. Indian J Endocrinol Metab 23(2):211–214
Kibirige D, Mwebaze R (2013) Vitamin B12 deficiency among patients with diabetes mellitus: is routine screening and supplementation justified? J Diabetes Metab Disord 12(1):17
Alshammari AN, Iqbal R, Baksh IP (2019) Vitamin B12 deficiency and the knowledge and practice of physicians regarding screening for vitamin B12 deficiency among type 2 diabetic patients on metformin in selected hospitals in Riyadh, Saudi Arabia. J Family Med Prim Care 8(7):2306–2311
Alhaji JH (2022) Vitamin B12 deficiency in patients with diabetes on metformin: Arab countries. Nutrients 14(10)
Nand L et al (2020) Vitamin B12 deficiency in patients of type 2 diabetes mellitus treated with metformin: a cross section observational study from a tertiary care centre in Sub-Himalayan region of North India. Int J Res Med Sci 8(4)
Krishnan GD, Zakaria MH, Yahaya N (2020) Prevalence of vitamin B12 deficiency and its associated factors among patients with type 2 diabetes mellitus on metformin from a district in Malaysia. J ASEAN Fed Endocr Soc 35(2):163–168
Gao L et al (2023) The effects of daily dose and treatment duration of metformin on the prevalence of vitamin B12 deficiency and peripheral neuropathy in Chinese patients with type 2 diabetes mellitus: a multicenter cross-sectional study. J Diabetes 15(9):765–776
Lala K, Lala D, Duggad S (2020) Serum vitamin B12 and homocysteine levels in type 2 diabetes patients on metformin. Int J Adv Med 7(9)
Sekhri T et al (2019) Vitamin B12 deficiency in patients with type 2 diabetes. Int J Adv Med 6(3)
Soutelo J et al (2020) Relationship between dose of metformin and vitamin B12 deficiency. CurR Res Diabetes Obes J 12(5):117–124
Ali K et al (2020) Association of vitamin B12 deficiency and metformin use in patients presenting with type ii diabetes mellitus. Pak Armed Forces Med J 70(5):1495–1498
Sakyi S et al (2020) Profiling immuno-metabolic mediators of vitamin B12 deficiency among metformin-treated type II diabetes patients in Ghana
Miyan Z, Waris N (2020) Association of vitamin B12 deficiency in people with type 2 diabetes on metformin and without metformin: a multicenter study, Karachi, Pakistan. BMJ Open Diabetes Res Care 8(1):e001151
Lata Kanyal M, Mujawar A (2019) Status of vitamin b12 in type 2 diabetes mellitus patients taking metformin based oral hypoglycemic agent-a cross sectional study. IJBAMR 1(9):18–26
Kim J et al (2019) Association between metformin dose and vitamin B12 deficiency in patients with type 2 diabetes. Medicine (Baltimore) 98(46):e17918
Zalaket J, Wehbe T, Abou Jaoude E (2018) Vitamin B12 deficiency in diabetic subjects taking metformin: a cross sectional study in a Lebanese cohort. J Nutr Intermed Metab 11:9–13
Khan A, Shafiq I, Hassan Shah M (2017) Prevalence of vitamin B12 deficiency in patients with type II diabetes mellitus on metformin: a study from Khyber Pakhtunkhwa. Cureus 9(8):e1577
Beulens JW et al (2015) Influence of duration and dose of metformin on cobalamin deficiency in type 2 diabetes patients using metformin. Acta Diabetol 52(1):47–53
Ko S-H et al (2014) Association of vitamin B12 deficiency and metformin use in patients with type 2 diabetes. J Korean Med Sci 29(7):965–972
Sato Y et al (2013) Relationship between metformin use, vitamin B12 deficiency, hyperhomocysteinemia and vascular complications in patients with type 2 diabetes. Endocr J E13-0332
de Groot-Kamphuis D et al (2013) Vitamin B12 deficiency and the lack of its consequences in type 2 diabetes patients using metformin. Neth J Med 71(7):386
Romero JMC, Lozano JMR (2012) Vitamin B12 in type 2 diabetic patients treated with metformin. Endocrinología y Nutrición (English Edition) 59(8):487–490
Reinstatler L et al (2012) Association of biochemical B12 deficiency with metformin therapy and vitamin B12 supplements: the National Health and Nutrition Examination Survey, 1999–2006. Diabetes Care 35(2):327–333
Liu K et al (2011) Metformin-associated vitamin B12 deficiency in the elderly. Asian J Gerontol Geriatr 6(2):82–87
Kancherla V et al (2017) Long-term metformin therapy and monitoring for vitamin B12 deficiency among older veterans. J Am Geriatr Soc 65(5):1061–1066
Wile DJ, Toth C (2010) Association of metformin, elevated homocysteine, and methylmalonic acid levels and clinically worsened diabetic peripheral neuropathy. Diabetes Care 33(1):156–161
de Jager J et al (2010) Long term treatment with metformin in patients with type 2 diabetes and risk of vitamin B-12 deficiency: randomised placebo controlled trial. BMJ 340:c2181
Rodríguez-Gutiérrez R et al (2017) Metformin use and vitamin B12 deficiency: untangling the association. Am J Med Sci 354(2):165–171
Raizada N et al (2017) Serum vitamin B12 levels in type 2 diabetes patients on metformin compared to those never on metformin: a cross-sectional study. Indian J Endocrinol Metab 21(3):424
Adetunji O et al (2009) Metformin and anaemia: myth or reality? Pract Diabetes Int 26(7):265–266
Elhadd T et al (2018) Metformin use is not associated with B12 deficiency or neuropathy in patients with type 2 diabetes mellitus in Qatar. Front Endocrinol 9:248
Flory J, Lipska K (2019) Metformin in 2019. JAMA 321(19):1926–1927
Corcoran C, Jacobs TF (2021) Metformin. StatPearls [Internet]
Rena G, Hardie DG, Pearson ER (2017) The mechanisms of action of metformin. Diabetologia 60(9):1577–1585
Bailey C, Wilcock C, Scarpello J (2008) Metformin and the intestine. Diabetologia 51(8):1552–1553
LaMoia TE, Shulman GI (2021) Cellular and molecular mechanisms of metformin action. Endocr Rev 42(1):77–96
Viollet B et al (2012) Cellular and molecular mechanisms of metformin: an overview. Clin Sci 122(6):253–270
Sinclair A, Dunning T, Colagiuri S (2013) Managing older people with type 2 diabetes: global guideline. International Diabetes Federation
Nathan D et al (2006) Management of hyperglycaemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. Diabetologia 49(8):1711–1721
Rizzo G, Laganà AS (2020) A review of vitamin B12. Mol Nutr 105–129
Watanabe F (2007) Vitamin B12 sources and bioavailability. Exp Biol Med 232(10):1266–1274
Allen LH (2008) Causes of vitamin B12 and folate deficiency. Food Nutr Bull 29(2_suppl1):S20–S34
Watanabe F et al (2002) Characterization and bioavailability of vitamin B12-compounds from edible algae. J Nutr Sci Vitaminol 48(5):325–331
Shane B (2008) Folate and vitamin B12 metabolism: overview and interaction with riboflavin, vitamin B6, and polymorphisms. Food Nutr Bull 29(2_suppl1):S5–S16
Shipton MJ, Thachil J (2015) Vitamin B12 deficiency - a 21st century perspective. Clin Med (Lond) 15(2):145–150
Lindenbaum J et al (1988) Neuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosis. N Engl J Med 318(26):1720–1728
Devalia V et al (2014) Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br J Haematol 166(4):496–513
Quadros EV (2010) Advances in the understanding of cobalamin assimilation and metabolism. Br J Haematol 148(2):195–204
Allen LH (2009) How common is vitamin B-12 deficiency? Am J Clin Nutr 89(2):693S–696S
Green R et al (2017) Vitamin B 12 deficiency. Nat Rev Dis Primers 3(1):1–20
da Silva L, McCray S (2009) Vitamin B12: no one should be without it. Pract Gastroenterol 33(34):39–42
Al-Batayneh KM et al (2018) Association between MTHFR 677C> T polymorphism and vitamin B12 deficiency: a case-control study. J Med Biochem 37(2):141
Al-Batayneh KM et al (2019) Homologous G776G variant of transcobalamin-II gene is linked to vitamin B12 deficiency. Int J Vitam Nutr Res
Lam JR et al (2013) Proton pump inhibitor and histamine 2 receptor antagonist use and vitamin B12 deficiency. JAMA 310(22):2435–2442
Tomkin G et al (1971) Vitamin-B12 status of patients on long-term metformin therapy. Br Med J 2(5763):685–687
Sparre Hermann L, Nilsson B, Wettre S (2004) Vitamin B12 status of patients treated with metformin: a cross-sectional cohort study. Br J Diabetes Vasc Dis 4(6):401–406
Singh A et al (2013) Association of B12 deficiency and clinical neuropathy with metformin use in type 2 diabetes patients. J Postgrad Med 59(4):253
Kang D et al (2014) Higher prevalence of metformin-induced vitamin B 12 deficiency in sulfonylurea combination compared with insulin combination in patients with type 2 diabetes: a cross-sectional study. PLoS ONE 9(10):e109878
Yang W et al (2019) Associations between metformin use and vitamin B(12) levels, anemia, and neuropathy in patients with diabetes: a meta-analysis. J Diabetes 11(9):729–743
Chapman LE, Darling AL, Brown JE (2016) Association between metformin and vitamin B(12) deficiency in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Metab 42(5):316–327
Caspary W, Creutzfeldt W (1971) Analysis of the inhibitory effect of biguanides on glucose absorption: inhibition of active sugar transport. Diabetologia 7(5):379–385
Buvat D (2004) Use of metformin is a cause of vitamin B12 deficiency. Am Fam Physician 69(2):264
Bauman WA et al (2000) Increased intake of calcium reverses vitamin B12 malabsorption induced by metformin. Diabetes Care 23(9):1227–1231
Ting RZ et al (2006) Risk factors of vitamin B(12) deficiency in patients receiving metformin. Arch Intern Med 166(18):1975–1979
Campbell JM et al (2018) Metformin use associated with reduced risk of dementia in patients with diabetes: a systematic review and meta-analysis. J Alzheimers Dis 65(4):1225–1236
Moore EM et al (2013) Increased risk of cognitive impairment in patients with diabetes is associated with metformin. Diabetes Care 36(10):2981–2987
Wakeman M, Archer DT (2020) Metformin and micronutrient status in type 2 diabetes: does polypharmacy involving acid-suppressing medications affect vitamin B12 levels? Diabetes Metab Syndr Obes 13:2093–2108
Miller JW (2018) Proton pump inhibitors, H2-receptor antagonists, metformin, and vitamin B-12 deficiency: clinical implications. Adv Nutr 9(4):511s–518s
Long AN et al (2012) Vitamin B12 deficiency associated with concomitant metformin and proton pump inhibitor use. Diabetes Care 35(12):e84–e84
Sahin M et al (2007) Effects of metformin or rosiglitazone on serum concentrations of homocysteine, folate, and vitamin B12 in patients with type 2 diabetes mellitus. J Diabetes Complications 21(2):118–123
Aroda VR et al (2016) Long-term metformin use and vitamin B12 deficiency in the diabetes prevention program outcomes study. J Clin Endocrinol Metab 101(4):1754–1761
Funding
Open Access funding provided by the Qatar National Library. The publication of this article was funded by the Qatar National Library.
Author information
Authors and Affiliations
Contributions
All authors contributed toward writing the initial draft and reviewing the manuscript. All agreed on the published version of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Al Zoubi, M.S., Al Kreasha, R., Aqel, S. et al. Vitamin B12 deficiency in diabetic patients treated with metformin: A narrative review. Ir J Med Sci 193, 1827–1835 (2024). https://doi.org/10.1007/s11845-024-03634-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-024-03634-4