Abstract
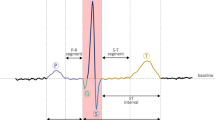
Cardiac health of the human heart is an intriguing issue for many decades as cardiovascular diseases (CVDs) are the leading cause of death worldwide. Electrocardiogram (ECG) signal is a powerful complete non-invasive tool for analyzing cardiac health. ECG signal is the primary choice of various health practitioners to determine vital information about the human heart. In the literature, the ECG signals are studied to diagnose and detect heart abnormalities such as enlargement of a heart chamber, detect cardiovascular diseases, detect ischemia, measure heart rate, biometric identification, and name a few. ECG signal being feeble suffers from the different kinds of noises, which might damage the ECG signal's morphological features, leading to wrong information and improper treatment. Removal of the noises from the ECG signal is an essential part of ECG signal processing. The denoised ECG signal facilitates the correct detection of the morphological features, which provides appropriate information about the cardiac health of the human heart. Detection of morphological features typically includes detecting QRS complex, R peak, and other ECG signal characteristics. These detected features are used to predict CVDs and other heart abnormalities. Earlier and accurate detection of CVDs involves two main steps: denoising and detection of a morphological feature. The increasing mortality rate due to CVDs compelled researchers to invent efficient computational techniques that automatically detect abnormalities in the heart. In the past few decades, various researchers have been proposed many computational methods to denoise and detect the ECG signal. This paper presents a comparative study of various existing state-of-the-art techniques used to analyze the ECG signal. Various noises influence the performance of the existing computational methods; hence, a summary of the different noises presented in the ECG signal is also included. The advantages and drawbacks of each method for ECG signal denoising and detection are discussed briefly. The efficiency of denoising and detection techniques was evaluated by testing the proposed algorithms using different standard databases like MIT-BIH, AHA, PTB, MIT-BIH noise stress test, Apnea-ECG. Details of these standard databases are provided in the paper. The performance of existing ECG signal denoising and detection algorithms is compared using parameters like signal-to-noise ratio improvement, percentage root mean square difference, root mean square error, sensitivity, positive predictivity, error, and accuracy. Finally, the challenges and gaps of the existing state-of-the-art techniques to analyze the ECG signal for automatic detection of CVDs are discussed.














Similar content being viewed by others
References
https://www.who.int/en/newsroom/factsheets/detail/cardiovascular-diseases-(CVD). Accessed 7 May 2021
Li P, Wang Yu, He J, Lihua Wang Yu, Tian T-S, Li T, Li J-S (2016) High-performance personalized heartbeat classification model for long-term ECG signal. IEEE Trans Biomed Eng 64(1):78–86. https://doi.org/10.1109/TBME.2016.2539421
da Luz EJS, Schwartz WR, Cámara-Chávez G, Menotti D (2016) ECG-based heartbeat classification for arrhythmia detection: a survey. Comput Methods Prog Biomed 127:144–164. https://doi.org/10.1016/CMPB.2015.12.008
Goldberger AL, Goldberger E (1981) Clinical electrocardiography, a simplified approach. Crit Care Med 9(12):891–892
Sörnmo L, Laguna P (2005) Bioelectrical signal processing in cardiac and neurological applications. Academic Press, Cambridge
Biel L, Pettersson O, Philipson L, Wide P (2001) ECG analysis: a new approach in human identification. IEEE Trans Instrum Meas 50(3):808–812. https://doi.org/10.1109/19.930458
Li Z, Li X, Zhu Z, Zeng S, Wang Y, Wang Y, Li A (2019) Signal analysis of electrocardiogram and statistical evaluation of myocardial enzyme in the diagnosis and treatment of patients with pneumonia. IEEE Access 7:113751–113759. https://doi.org/10.1109/ACCESS.2018.2889354
Bailón R, Sornmo L, Laguna P (2006) A robust method for ECG-based estimation of the respiratory frequency during stress testing. IEEE Trans Biomed Eng 53(7):1273–1285. https://doi.org/10.1109/TBME.2006.871888
https://ecgwaves.com/reference-values-for-ecg-electrocardiography/(last. Accessed 7 May 2021
Kumar A, Ranganatham R, Kumar M, Komaragiri R (2020) Hardware emulation of a biorthogonal wavelet transform-based heart rate monitoring device. IEEE Sens J 21(4):5271–5281. https://doi.org/10.1109/JSEN.2020.3034742
Cromwell L, Weibell FJ, Pfeiffer EA (1980) Biomedical instrumentation and measurements, 2nd edn. Prentice-Hall Inc., New Jersey
Rajankar SO, Talbar SN (2019) An electrocardiogram signal compression techniques: a comprehensive review. Analog Integr Circ Sig Process 98(1):59–74. https://doi.org/10.1007/s10470-018-1323-1
Pan J, Tompkins WJ (1985) A real-time QRS detection algorithm. IEEE Trans Biomed Eng 3:230–236. https://doi.org/10.1109/TBME.1985.325532
Friesen GM, Jannett TC, Jadallah MA, Yates SL, Quint SR, Nagle HT (1990) A comparison of the noise sensitivity of nine QRS detection algorithms. IEEE Trans Biomed Eng 37(1):85–98. https://doi.org/10.1109/10.43620
Satija U, Ramkumar B, Manikandan MS (2018) A review of signal processing techniques for electrocardiogram signal quality assessment. IEEE Rev Biomed Eng 11:36–52. https://doi.org/10.1109/RBME.2018.2810957
Clifford GD, Azuaje F, Mcsharry P (2006) ECG statistics, noise, artifacts, and missing data. Adv Methods Tools ECG Data Anal 6:18
Kligfield P, Gettes LS, Bailey JJ, Childers R, Deal BJ, William Hancock E, Van Herpen G et al (2007) Recommendations for the standardization and interpretation of the electrocardiogram: part I: the electrocardiogram and its technology a scientific statement from the American heart association electrocardiography and arrhythmias committee, council on clinical cardiology; the American college of cardiology foundation; and the heart rhythm society endorsed by the international society for computerized electrocardiology. J Am Coll Cardiol 49(10):1109–1127. https://doi.org/10.1016/JACC.2007.01.024
Luo S, Johnston P (2010) A review of electrocardiogram filtering. J Electrocardiol 43(6):486–496. https://doi.org/10.1016/JELECTROCARD.2010.07.007
https://www.analog.com/media/en/training-seminars/design-handbooks/Basic-Linear-Design/Chapter8.pdf. Accessed 09 May 2021
Kumar A, Komaragiri R, Kumar M (2019) Design of efficient fractional operator for ECG signal detection in implantable cardiac pacemaker systems. Int J Circuit Theory Appl 47(9):1459–1476. https://doi.org/10.1002/cta.2667
Acharya UR, Krishnan SM, Spaan JAE, Suri JS (eds) (2007) Advances in cardiac signal processing. Springer, Berlin
Jagtap SK, Uplane MD (2013) Digital filter approach for ECG in signal processing. In: Proceedings of international conference on advances in computing. Springer, New Delhi, pp. 1075–1082
Wang K, Ma S, Feng J, Zhang W, Fan M, Zhao D (2012) Design of ECG signal acquisition system based on DSP. Proc Eng 29:3763–3767. https://doi.org/10.1016/PROENG.2012.01.567
Lee Y, Hwang D (2018) Periodicity-based nonlocal-means denoising method for electrocardiography in low SNR non-white noisy conditions. Biomed Signal Process Control 39:284–293. https://doi.org/10.1016/BSPC.2017.08.006
Wang X, Zhou Y, Shu M, Wang Y, Dong A (2019) ECG baseline wander correction and denoising based on sparsity. IEEE Access 7:31573–31585. https://doi.org/10.1109/ACCESS.2019.2902616
Wang J, Ye Y, Pan X, Gao X (2015) Parallel-type fractional zero-phase filtering for ECG signal denoising. Biomed Signal Process Control 18:36–41. https://doi.org/10.1016/BSPC.2014.10.012
Cuomo S, De Pietro G, Farina R, Galletti A, Sannino G (2016) A revised scheme for real time ecg signal denoising based on recursive filtering. Biomed Signal Process Control 27:134–144. https://doi.org/10.1016/BSPC.2016.02.007
Mourad N (2019) ECG denoising algorithm based on group sparsity and singular spectrum analysis. Biomed Signal Process Control 50:62–71. https://doi.org/10.1016/BSPC.2019.01.018
Cuomo, S, De Pietro G, Farina R, Galletti A, Sannino G (2015) A novel O (n) numerical scheme for ECG signal denoising. In: ICCS, pp. 775–784
Panigrahy D, Sahu PK (2016) Extended Kalman smoother with differential evolution technique for denoising of ECG signal. Australas Phys Eng Sci Med 39(3):783–795. https://doi.org/10.1007/s13246-016-0468-4
Jenkal W, Latif R, Toumanari A, Dliou A, El Bcharri O, Maoulainine FMR (2016) An efficient algorithm of ECG signal denoising using the adaptive dual threshold filter and the discrete wavelet transform. Biocybern Biomed Eng 36(3):499–508. https://doi.org/10.1016/BBE.2016.04.001
Singh P, Pradhan G, Shahnawazuddin S (2017) Denoising of ECG signal by non-local estimation of approximation coefficients in DWT. Biocybern Biomed Eng 37(3):599–610. https://doi.org/10.1016/BBE.2017.06.001
Lin H-Y, Liang S-Y, Ho Y-L, Lin Y-H, Ma H-P (2014) Discrete-wavelet-transform-based noise removal and feature extraction for ECG signals. Irbm 35(6):351–361. https://doi.org/10.1016/IRBM.2014.10.004
Wang F, Ji Z (2014) Application of the dual-tree complex wavelet transform in biomedical signal denoising. Bio-Med Mater Eng 24(1):109–115
El Bcharri O, Latif R, Elmansouri K, Abenaou A, Jenkal W (2017) ECG signal performance de-noising assessment based on threshold tuning of dual-tree wavelet transform. Biomed Eng Online 16(1):26. https://doi.org/10.1186/s12938-017-0315-1
Zhang S, Gao J, Yang J, Yu S (2013) A Mallat based wavelet ECG de-noising algorithm. In: Applied mechanics and materials, vol. 263. Trans Tech Publications Ltd, Freienbach, pp. 2267–2270. https://doi.org/10.4028/www.scientific.net/AMM.263-266.2267
Peng Z, Wang G (2017) Study on optimal selection of wavelet vanishing moments for ECG denoising. Sci Rep 7(1):1–11. https://doi.org/10.1038/s41598-017-04837-9
Han G, Zhijun Xu (2016) Electrocardiogram signal denoising based on a new improved wavelet thresholding. Rev Sci Instrum 87(8):084303. https://doi.org/10.1063/1.4960411
Hong HE, Yonghong TAN (2018) A novel adaptive wavelet thresholding with identical correlation shrinkage function for ECG noise removal. Chin J Electron 27(3):507–513. https://doi.org/10.1049/CJE.2018.02.006
Kumar A, Komaragiri R, Kumar M (2018) Heart rate monitoring and therapeutic devices: a wavelet transform based approach for the modeling and classification of congestive heart failure. ISA Trans 79:239–250. https://doi.org/10.1016/ISATRA.2018.05.003
Kumar A, Komaragiri R, Kumar M (2018) Design of wavelet transform based electrocardiogram monitoring system. ISA Trans 80:381–398. https://doi.org/10.1016/ISATRA.2018.08.003
Smital L, Vitek M, Kozumplík J, Provaznik I (2012) Adaptive wavelet wiener filtering of ECG signals. IEEE Trans Biomed Eng 60(2):437–445. https://doi.org/10.1109/TBME.2012.2228482
Hao H, Wang H, Rehman NU, Chen L, Tian H (2017) An improved multivariate wavelet denoising method using subspace projection. IEICE Trans Fundam Electron, Commun Comput Sci 100(3):769–775. https://doi.org/10.1587/TRANSFUNE100.A.769
Kumar A, Komaragiri R, Kumar M (2019) Time–frequency localization using three-tap biorthogonal wavelet filter bank for electrocardiogram compressions. Biomed Eng Lett 9(3):407–411. https://doi.org/10.1007/s13534-019-00117-9
Yadav SK, Sinha R, Bora PK (2015) Electrocardiogram signal denoising using non-local wavelet transform domain filtering. IET Signal Process 9(1):88–96. https://doi.org/10.1049/IET-SPR.2014.0005
Tracey BH, Miller EL (2012) Nonlocal means denoising of ECG signals. IEEE Trans Biomed Eng 59(9):2383–2386. https://doi.org/10.1109/TBME.2012.2208964
Qian C, Honghong Su, Helong Yu (2019) Local means denoising of ECG signal. Biomed Signal Process Control 53:101571. https://doi.org/10.1016/BSPC.2019.101571
Anapagamini SA, Rajavel R (2016) Hardware implementation of ECG denoising system using TMS320C6713 DSP processor. Int J Biomed Eng Technol 21(1):95–108. https://doi.org/10.1504/IJBET.2016.076735
Jain S, Bajaj V, Kumar A (2017) Riemann Liouvelle fractional integral based empirical mode decomposition for ECG denoising. IEEE J Biomed Health Inform 22(4):1133–1139. https://doi.org/10.1109/JBHI.2017.2753321
Kumar S, Panigrahy D, Sahu PK (2018) Denoising of electrocardiogram (ECG) signal by using empirical mode decomposition (EMD) with non-local mean (NLM) technique. Biocybern Biomed Eng 38(2):297–312. https://doi.org/10.1016/BBE.2018.01.005
Rakshit M, Das S (2018) An efficient ECG denoising methodology using empirical mode decomposition and adaptive switching mean filter. Biomed Signal Process Control 40:140–148. https://doi.org/10.1016/BSPC.2017.09.020
Kabir MDA, Shahnaz C (2012) Denoising of ECG signals based on noise reduction algorithms in EMD and wavelet domains. Biomed Signal Process Control 7(5):481–489. https://doi.org/10.1016/BSPC.2011.11.003
Singh P, Shahnawazuddin S, Pradhan G (2018) An efficient ECG denoising technique based on non-local means estimation and modified empirical mode decomposition. Circuits Syst Signal Process 37(10):4527–4547. https://doi.org/10.1007/s00034-018-0777-9
Jain S, Bajaj V, Kumar A (2018) Effective de-noising of ECG by optimised adaptive thresholding on noisy modes. IET Sci Meas Technol 12(5):640–644. https://doi.org/10.1049/IET-SMT.2017.0203
Wang M, Zhou Z, Li Z, Zeng Y (2019) An adaptive denoising algorithm for chaotic signals based on improved empirical mode decomposition. Circuits Syst Signal Process 38(6):2471–2488. https://doi.org/10.1007/s00034-018-0973-7
Das MK, Ari S (2013) Analysis of ECG signal denoising method based on S-transform. Irbm 34(6):362–370. https://doi.org/10.1016/IRBM.2013.07.012
Singhal A, Singh P, Fatimah B, Pachori RB (2020) An efficient removal of power-line interference and baseline wander from ECG signals by employing Fourier decomposition technique. Biomed Signal Process Control 57:101741. https://doi.org/10.1016/BSPC.2019.101741
Tan C, Zhang L, Hau-tieng Wu (2018) A novel blaschke unwinding adaptive-Fourier-decomposition-based signal compression algorithm with application on ECG signals. IEEE J Biomed Health Inform 23(2):672–682. https://doi.org/10.1109/JBHI.2018.2817192
Sharma RR, Pachori RB (2018) Baseline wander and power line interference removal from ECG signals using eigenvalue decomposition. Biomed Signal Process Control 45:33–49. https://doi.org/10.1016/BSPC.2018.05.002
Kumar A, Tomar H, Mehla VK, Komaragiri R, Kumar M (2021) Stationary wavelet transform based ECG signal denoising method. ISA Trans 114:251–262. https://doi.org/10.1016/ISATRA.2020.12.029
Prashar N, Sood M, Jain S (2021) Design and implementation of a robust noise removal system in ECG signals using dual-tree complex wavelet transform. Biomed Signal Process Control 63:102212. https://doi.org/10.1016/BSPC.2020.102212
Dotsinsky I, Christov I, Daskalov I (1996) Assessment of metrological characteristics of digital electrocardiographs. J Clin Eng 21(2):156
García-Niebla J, Serra-Autonell G (2009) Effects of inadequate low-pass filter application. J Electrocardiol 42(4):303–304. https://doi.org/10.1016/JELECTROCARD.2009.03.002
Mikiko N, Tsunemitsu C, Katoh S, Kamiyama Y, Sano N, Ezaki K, Miyazaki H et al (2014) Effect of ECG filter settings on J-waves. J Electrocardiol 47(1):7–11. https://doi.org/10.1016/JELECTROCARD.2013.10.001
Christov I, Neycheva T, Schmid R, Stoyanov T, Abächerli R (2017) Pseudo-real-time low-pass filter in ECG, self-adjustable to the frequency spectra of the waves. Med Biol Eng Compu 55(9):1579–1588. https://doi.org/10.1007/s11517-017-1625-y
Watford C (2014) Understanding ECG Filtering, EMS 12-Lead, EMS-Topics. https://www.rigacci.org/wiki/lib/exe/fetch.php/tecnica/misc/ecg90a/understanding-ecg-filtering.pdf. Accessed 11 Sept 2021
Tantawi MM, Revett K, Salem A, Tolba MF (2013) Fiducial feature reduction analysis for electrocardiogram (ECG) based biometric recognition. J Intell Inf Syst 40(1):17–39. https://doi.org/10.1007/s10844-012-0214-7
Coutinho DP, Silva H, Gamboa H, Fred A, Figueiredo M (2013) Novel fiducial and non-fiducial approaches to electrocardiogram-based biometric systems. IET Biom 2(2):64–75. https://doi.org/10.1049/IET-BMT.2012.0055
Chua TW, Tan WW (2011) Non-singleton genetic fuzzy logic system for arrhythmias classification. Eng Appl Artif Intell 24(2):251–259. https://doi.org/10.1016/ENGAPPAI.2010.10.003
Haseena HH, Mathew AT, Paul JK (2011) Fuzzy clustered probabilistic and multi layered feed forward neural networks for electrocardiogram arrhythmia classification. J Med Syst 35(2):179–188. https://doi.org/10.1007/s10916-009-9355-9
Burguera A (2018) Fast QRS detection and ECG compression based on signal structural analysis. IEEE J Biomed Health Inform 23(1):123–131. https://doi.org/10.1109/JBHI.2018.2792404
Vullings R, De Vries B, Bergmans JWM (2010) An adaptive Kalman filter for ECG signal enhancement. IEEE Trans Biomed Eng 58(4):1094–1103. https://doi.org/10.1109/TBME.2010.2099229
Berkaya SK, Uysal AK, Gunal ES, Ergin S, Gunal S, Gulmezoglu MB (2018) A survey on ECG analysis. Biomed Signal Process Control 43:216–235. https://doi.org/10.1016/BSPC.2018.03.003
Hiasat AA, Al-Ibrahim MM, Gharaibeh KM (1999) Design and implementation of a new efficient median filtering algorithm. IEE Proceedings-Vision, Image Signal Process 146(5):273–278. https://doi.org/10.1049/IP-VIS:19990444
Acharya D, Rani A, Agarwal S, Singh V (2016) Application of adaptive Savitzky-Golay filter for EEG signal processing. Perspect Sci 8:677–679. https://doi.org/10.1016/PISC.2016.06.056
Widrow B, Glover JR, McCool JM, Kaunitz J, Williams CS, Hearn RH, Zeidler JR, Dong JRE, Goodlin RC (1975) Adaptive noise cancelling: principles and applications. Proc IEEE 63(12):1692–1716. https://doi.org/10.1109/PROC.1975.10036
Thakor NV, Zhu Y-S (1991) Applications of adaptive filtering to ECG analysis: noise cancellation and arrhythmia detection. IEEE Trans Biomed Eng 38(8):785–794. https://doi.org/10.1109/10.83591
Haykin SS (2008) Adaptive filter theory. Pearson Education India, Delhi
Soria-Olivas E, Martinez-Sober M, Calpe-Maravilla J, Guerrero-Martinez JF, Chorro-Gascó J, Espí-López J (1998) Application of adaptive signal processing for determining the limits of P and T waves in an ECG. IEEE Trans Biomed Eng 45(8):1077–1080
Smith SW (1997) The scientist and engineer’s guide to digital signal processing. California Technical Publication, San Diego
Li T, Wen P, Jayamaha S (2014) Anaesthetic EEG signal denoise using improved nonlocal mean methods. Australas Phys Eng Sci Med 37(2):431–437. https://doi.org/10.1007/s13246-014-0263-z
Edmonson W, Palacios JC, Lai CA, Latchman H (1999) A global optimization method for continuous-time adaptive recursive filters. IEEE Signal Process Lett 6(8):199–201. https://doi.org/10.1109/97.774864
Sameni R, Shamsollahi MB, Jutten C, Clifford GD (2007) A nonlinear Bayesian filtering framework for ECG denoising. IEEE Trans Biomed Eng 54(12):2172–2185. https://doi.org/10.1109/TBME.2007.897817
Milchevski A, Gusev M (2016) Performance evaluation of FIR and IIR filtering of ECG signals. In: International conference on ICT innovations. Springer, Cham. pp. 103–112. https://doi.org/10.1007/978-3-319-68855-8_10
Srivastva R, Singh YN (2019) ECG analysis for human recognition using non-fiducial methods. IET Biom 8(5):295–305. https://doi.org/10.1049/IET-BMT.2018.5093
Krishnan S, Athavale Y (2018) Trends in biomedical signal feature extraction. Biomed Signal Process Control 43:41–63. https://doi.org/10.1016/BSPC.2018.02.008
Pandya UT, Desai UB (2012) A novel algorithm for bluetooth ECG. IEEE Trans Biomed Eng 59(11):3148–3154. https://doi.org/10.1109/TBME.2012.2217494
Kumar A, Ranganatham R, Komaragiri R, Kumar M (2019) Efficient QRS complex detection algorithm based on Fast Fourier Transform. Biomed Eng Lett 9(1):145–151. https://doi.org/10.1007/s13534-018-0087-y
Noor SM, John E, Panday M (2018) Design and implementation of an ultralow-energy FFT ASIC for processing ECG in cardiac pacemakers. IEEE Trans Very Large Scale Integr Syst 27(4):983–987
Bendifallah A, Benzid R, Boulemden M (2011) Improved ECG compression method using discrete cosine transform. Electron Lett 47(2):87–89. https://doi.org/10.1049/EL.2010.3191
Benzid R, Messaoudi A, Boussaad A (2008) Constrained ECG compression algorithm using the block-based discrete cosine transform. Dig Signal Process 18(1):56–64. https://doi.org/10.1016/DSP.2007.08.003
Raj S, Ray KC (2017) ECG signal analysis using DCT-based DOST and PSO optimized SVM. IEEE Trans Instrum Measurement 66(3):470–478. https://doi.org/10.1109/TIM.2016.2642758
https://cs.stanford.edu/people/eroberts/courses/soco/projects/data-compression/lossy/jpeg/dct.htm. Accessed 7 May 2021
Shaik BS, Naganjaneyulu GVSSKR, Chandrasheker T, Narasimhadhan AV (2015) A method for QRS delineation based on STFT using adaptive threshold. Proc Comput Sci 54:646–653. https://doi.org/10.1016/PROCS.2015.06.075
Quatieri SNT, Lim J (1983) Signal reconstruction from short-time Fourier transform magnitude. IEEE Trans Acoust, Speech, Signal Process 31(4):986–998. https://doi.org/10.1109/TASSP.1983.1164162
Xie Q, Shikui Tu, Wang G, Lian Y, Lei Xu (2019) Feature enrichment based convolutional neural network for heartbeat classification from electrocardiogram. IEEE Access 7:153751–153760. https://doi.org/10.1109/ACCESS.2019.2948857
Singh BN, Tiwari AK (2006) Optimal selection of wavelet basis function applied to ECG signal denoising. Digital Signal Process 16(3):275–287. https://doi.org/10.1016/DSP.2005.12.003
Sabherwal P, Agrawal M, Singh L (2017) Automatic detection of the R peaks in single-lead ECG signal. Circuits Syst Signal Process 36(11):4637–4652. https://doi.org/10.1007/s00034-017-0537-2
Sahoo S, Biswal P, Das T, Sabut S (2016) De-noising of ECG signal and QRS detection using Hilbert transform and adaptive thresholding. Proc Technol 25:68–75. https://doi.org/10.1016/PROTCY.2016.08.082
Banerjee S, Gupta R, Mitra M (2012) Delineation of ECG characteristic features using multiresolution wavelet analysis method. Measurement 45(3):474–487. https://doi.org/10.1016/MEASUREMENT.2011.10.025
Rakshit M, Das S (2017) An efficient wavelet-based automated R-peaks detection method using Hilbert transform. Biocybern Biomed Eng 37(3):566–577. https://doi.org/10.1016/BBE.2017.02.002
Park J-S, Lee S-W, Park U (2017) R peak detection method using wavelet transform and modified Shannon energy envelope. J Healthc Eng. https://doi.org/10.1155/2017/4901017
Li C, Zheng C, Tai C (1995) Detection of ECG characteristic points using wavelet transforms. IEEE Trans Biomed Eng 42(1):21–28. https://doi.org/10.1109/10.362922
Li P, Zhang Xu, Liu M, Xiaohui Hu, Pang Bo, Yao Z, Jiang H, Chen H (2017) A 410-nW efficient QRS processor for mobile ECG monitoring in 0.18-μm CMOS. IEEE Trans Biomed Circuits Syst 11(6):1356–1365. https://doi.org/10.1109/TBCAS.2017.2731797
Yochum M, Renaud C, Jacquir S (2016) Automatic detection of P, QRS and T patterns in 12 leads ECG signal based on CWT. Biomed Signal Process Control. https://doi.org/10.1016/BSPC.2015.10.011
Sabherwal P, Singh L, Agrawal M (2018) Aiding the detection of QRS complex in ECG signals by detecting S peaks independently. Cardiovasc Eng Technol 9(3):469–481. https://doi.org/10.1007/s13239-018-0355-0
Huang NE, Shen Z, Long SR, Wu MC, Shih EH, Zheng Q, Tung CC, Liu HH (1998) The empirical mode decomposition method and the Hilbert spectrum for non-stationary time series analysis. Proc Roy Soc London 454A:903–995. https://doi.org/10.1098/RSPA.1998.0193
Labate D, Foresta FL, Occhiuto G, Morabito FC, Lay-Ekuakille A, Vergallo P (2013) Empirical mode decomposition vs. wavelet decomposition for the extraction of respiratory signal from single-channel ECG: a comparison. IEEE Sens J 13(7):2666–2674. https://doi.org/10.1109/JSEN.2013.2257742
Karagiannis A, Constantinou P (2010) Noise-assisted data processing with empirical mode decomposition in biomedical signals. IEEE Trans Inf Technol Biomed 15(1):11–18. https://doi.org/10.1109/TITB.2010.2091648
Chang K-M (2010) Arrhythmia ECG noise reduction by ensemble empirical mode decomposition. Sensors 10(6):6063–6080. https://doi.org/10.3390/s100606063
Wu Z, Huang NE (2009) Ensemble empirical mode decomposition: a noise-assisted data analysis method. Adv Adapt Data Anal 1(01):1–41. https://doi.org/10.1142/S1793536909000047
Gaci S (2016) A new ensemble empirical mode decomposition (EEMD) denoising method for seismic signals. Energy Proc 97:84–91
Fosso, OB., Molinas M (2017) Method for mode mixing separation in empirical mode decomposition." arXiv preprint
Rajesh KNVPS, Dhuli R (2017) Classification of ECG heartbeats using nonlinear decomposition methods and support vector machine. Comput Biol Med 87:271–284. https://doi.org/10.1016/COMPBIOMED.2017.06.006
Jebaraj J, Arumugam R (2016) Ensemble empirical mode decomposition-based optimised power line interference removal algorithm for electrocardiogram signal. IET Signal Proc 10(6):583–591. https://doi.org/10.1049/IET-SPR.2015.0292
Maji U, Mitra M, Pal S (2015) Detection and characterisation of QRS complex in VMD domain pp. 101–5. https://doi.org/10.1049/CP.2015.1697
Goovaerts G, Padhy S, Vandenberk B, Varon C, Willems R, Huffel SV (2018) A machine-learning approach for detection and quantification of QRS fragmentation. IEEE J Biomed Health Inform 23(5):1980–1989. https://doi.org/10.1109/JBHI.2018.2878492
Gupta V, Mittal M, Mittal V (2019) R-peak detection using chaos analysis in standard and real time ECG databases. IRBM 40(6):341–354. https://doi.org/10.1016/IRBM.2019.10.001
Chawla MPS (2011) PCA and ICA processing methods for removal of artifacts and noise in electrocardiograms: a survey and comparison. Appl Soft Comput 11(2):2216–2226. https://doi.org/10.1016/ASOC.2010.08.001
Sharma T, Sharma KK (2017) QRS complex detection in ECG signals using locally adaptive weighted total variation denoising. Comput Biol Med 87:187–199. https://doi.org/10.1016/COMPBIOMED.2017.05.027
Gutiérrez-Rivas R, García JJ, Marnane WP, Hernández A (2015) Novel real-time low-complexity QRS complex detector based on adaptive thresholding. IEEE Sens J 15(10):6036–6043. https://doi.org/10.1109/JSEN.2015.2450773
Christov II (2004) Real time electrocardiogram QRS detection using combined adaptive threshold. Biomed Eng Online 3(1):28. https://doi.org/10.1186/1475-925X-3-28
Castells-Rufas D, Carrabina J (2015) Simple real-time QRS detector with the MaMeMi filter. Biomed Signal Process Control 21:137–145. https://doi.org/10.1016/BSPC.2015.06.001
Rekik S, Ellouze N (2017) Enhanced and optimal algorithm for QRS detection. Irbm 38(1):56–61. https://doi.org/10.1016/IRBM.2016.11.004
Farashi S (2016) A multiresolution time-dependent entropy method for QRS complex detection. Biomed Signal Process Control 24:63–71. https://doi.org/10.1016/BSPC.2015.09.008
Hou Z, Dong Y, Xiang J, Li X, Yang B (2018) A real-time QRS detection method based on phase portraits and box-scoring calculation. IEEE Sens J 18(9):3694–3702. https://doi.org/10.1109/JSEN.2018.2812792
Modak S, Taha LY, Abdel-Raheem E (2021) A novel method of QRS detection using time and amplitude thresholds with statistical false peak elimination. IEEE Access 9:46079–46092. https://doi.org/10.1109/ACCESS.2021.3067179
Morshedlou F, Ravanshad N, Rezaee-Dehsorkh H (2021) An ultra-low power analog QRS-detection circuit for ambulatory ECG monitoring. AEU-Int J Electron Commun 129:153551. https://doi.org/10.1016/AEUE.2020.153551
Kumar A, Ranganatham R, Singh S, Komaragiri R, Kumar M (2021) A robust digital ECG signal watermarking and compression using biorthogonal wavelet transform. Res Biomed Eng 37(1):79–85. https://doi.org/10.1007/s42600-020-00108-1
Kumar A, Komaragiri R, Kumar M (2018) From pacemaker to wearable: techniques for ECG detection systems. J Med Syst 42(2):1–17. https://doi.org/10.1007/s10916-017-0886-1
Kumar A, Kumar M, Komaragiri R (2018) Design of a biorthogonal wavelet transform based R-peak detection and data compression scheme for implantable cardiac pacemaker systems. J Med Syst 42(6):1–12. https://doi.org/10.1007/s10916-018-0953-2
Kumar A, Mehla VK, Tomar H, Kumar M, Komaragiri R (2020) Classification of normal and abnormal ECG signals using support vector machine and Fourier decomposition method. In: 2020 IEEE International symposium on smart electronic systems (iSES)(Formerly iNiS), pp. 161–166. IEEE, 2020. https://doi.org/10.1109/iSES50453.2020.00044
Saadi DB, Tanev G, Flintrup M, Osmanagic A, Egstrup K, Hoppe K, Jennum P, Jeppesen JL, Iversen HK, Sorensen HBD (2015) Automatic real-time embedded QRS complex detection for a novel patch-type electrocardiogram recorder. IEEE J Transl Eng Health Med 3:1–12. https://doi.org/10.1109/JTEHM.2015.2421901
Kim J, Shin H (2016) Simple and robust realtime QRS detection algorithm based on spatiotemporal characteristic of the QRS complex. PLoS ONE 11(3):e0150144. https://doi.org/10.1371/JOURNAL.PONE.0150144
Yakut Ö, Bolat ED (2018) An improved QRS complex detection method having low computational load. Biomed Signal Process Control 42:230–241. https://doi.org/10.1016/BSPC.2018.02.004
Ferdi Y, Herbeuval JP, Charef A, Boucheham B (2003) R wave detection using fractional digital differentiation. ITBM-RBM 24(5–6):273–280. https://doi.org/10.1016/RBMRET.2003.08.002
Benmalek M, Charef A (2009) Digital fractional order operators for R-wave detection in electrocardiogram signal. IET Signal Proc 3(5):381–391. https://doi.org/10.1049/IET-SPR.2008.0094
Nayak C, Saha SK, Kar R, Mandal D (2018) Automated QRS complex detection using MFO-based DFOD. IET Signal Process 12(9):1172–1184. https://doi.org/10.1049/IET-SPR.2018.5230
Nayak C, Saha SK, Kar R, Mandal D (2019) An efficient QRS complex detection using optimally designed digital differentiator. Circuits, Syst, Signal Process 38(2):716–749. https://doi.org/10.1007/s00034-018-0880-y
Bashar SK, Noh Y, Walkey AJ, McManus DD, Chon KH (2019) VERB: VFCDM-based electrocardiogram reconstruction and beat detection algorithm. IEEE Access 7:13856–13866
Chin W-L, Chang C-C, Tseng C-L, Huang Y-Z, Jiang T (2019) Bayesian real-time QRS complex detector for healthcare system. IEEE Internet Things J 6(3):5540–5549. https://doi.org/10.1109/JIOT.2019.2903530
Nayak C, Saha SK, Kar R, Mandal D (2019) An efficient and robust digital fractional order differentiator-based ECG Pre-processor design for QRS detection. IEEE Trans Biomed Circuits Syst 13(4):682–696. https://doi.org/10.1109/TBCAS.2019.2916676
Nayak C, Saha SK, Kar R, Mandal D (2019) An optimally designed digital differentiator based preprocessor for R-peak detection in electrocardiogram signal. Biomed Signal Process Control 49:440–464. https://doi.org/10.1016/BSPC.2018.09.005
Yazdani S, Vesin J-M (2016) Extraction of QRS fiducial points from the ECG using adaptive mathematical morphology. Dig Signal Process 56:100–109. https://doi.org/10.1016/DSP.2016.06.010
Jain S, Kumar A, Bajaj V (2016) Technique for QRS complex detection using particle swarm optimisation. IET Sci Meas Technol 10(6):626–636. https://doi.org/10.1049/IET-SMT.2016.0023
Pandit D, Zhang L, Liu C, Chattopadhyay S, Aslam N, Lim CP (2017) A lightweight QRS detector for single lead ECG signals using a max-min difference algorithm. Comput Methods Prog Biomed 144:61–75. https://doi.org/10.1016/CMPB.2017.02.028
Lee M, Park D, Dong S-Y, Youn I (2018) A novel R peak detection method for mobile environments. IEEE Access 6:51227–51237. https://doi.org/10.1109/ACCESS.2018.2867329
Sharma LD, Sunkaria RK (2016) A robust QRS detection using novel pre-processing techniques and kurtosis based enhanced efficiency. Measurement 87:194–204. https://doi.org/10.1016/MEASUREMENT.2016.03.015
Jain S, Ahirwal MK, Kumar A, Bajaj V, Singh GK (2017) QRS detection using adaptive filters: a comparative study. ISA Trans 66:362–375. https://doi.org/10.1016/ISATRA.2016.09.023
Elgendi M, Mohamed A, Ward R (2017) Efficient ECG compression and QRS detection for e-health applications. Sci Rep 7(1):1–16. https://doi.org/10.1038/s41598-017-00540-x
Zidelmal Z, Amirou A, Ould-Abdeslam D, Moukadem A, Dieterlen A (2014) QRS detection using S-Transform and Shannon energy. Comput Methods Prog Biomed 116(1):1–9. https://doi.org/10.1016/CMPB.2014.04.008
Biswal B (2017) ECG signal analysis using modified S-transform. Healthc Technol Lett 4(2):68–72. https://doi.org/10.1049/HTL.2016.0078
Chen C-L, Chuang C-T (2017) A QRS detection and R point recognition method for wearable single-lead ECG devices. Sensors 17(9):1969. https://doi.org/10.3390/s17091969
Merah M, Abdelmalik TA, Larbi BH (2015) R-peaks detection based on stationary wavelet transform. Comput Methods Progr Biomed 121(3):149–160. https://doi.org/10.1016/CMPB.2015.06.003
Berwal D, Kumar A, Kumar Y (2018) Design of high performance QRS complex detector for wearable healthcare devices using biorthogonal spline wavelet transform. ISA Trans 81:222–230. https://doi.org/10.1016/ISATRA.2018.08.002
Sharma A, Patidar S, Upadhyay A, Acharya UR (2019) Accurate tunable-Q wavelet transform based method for QRS complex detection. Comput Electr Eng 75:101–111. https://doi.org/10.1016/COMPELECENG.2019.01.025
Ravanshad N, Rezaee-Dehsorkh H, Lotfi R, Lian Y (2013) A level-crossing based QRS-detection algorithm for wearable ECG sensors. IEEE J Biomed Health Inform 18(1):183–192. https://doi.org/10.1109/JBHI.2013.2274809
Qin Q, Li J, Yue Y, Liu C (2017) An adaptive and time-efficient ECG R-peak detection algorithm. J Healthc Eng. https://doi.org/10.1155/2017/5980541
Deepu CJ, Lian Y (2014) A joint QRS detection and data compression scheme for wearable sensors. IEEE Trans Biomed Eng 62(1):165–175. https://doi.org/10.1109/TBME.2014.2342879
Tang X, Qisong Hu, Tang W (2018) A real-time QRS detection system with PR/RT interval and ST segment measurements for wearable ECG sensors using parallel delta modulators. IEEE Trans Biomed Circuits Syst 12(4):751–761. https://doi.org/10.1109/TBCAS.2018.2823275
Li Y, Tang X, Zhi Xu, Yan H (2018) A novel approach to phase space reconstruction of single lead ECG for QRS complex detection. Biomed Signal Process Control 39:405–415. https://doi.org/10.1016/BSPC.2017.06.007
Bajaj A, Kumar S (2019) QRS complex detection using fractional Stockwell transform and fractional Stockwell Shannon energy. Biomed Signal Process Control 54:101628. https://doi.org/10.1016/BSPC.2019.101628
Hossain MB, Bashar SK, Walkey AJ, McManus DD, Chon KH (2019) An accurate QRS complex and P-wave detection in ECG signals using complete ensemble empirical mode decomposition with adaptive noise approach. IEEE Access 7:128869–128880. https://doi.org/10.1109/ACCESS.2019.2939943
Jia M, Li F, Jiaquan Wu, Chen Z, Yu Pu (2020) Robust QRS detection using high-resolution wavelet packet decomposition and time-attention convolutional neural network. IEEE Access 8:16979–16988. https://doi.org/10.1109/ACCESS.2020.2967775
Chen H, Maharatna K (2020) An automatic R and T peak detection method based on the combination of hierarchical clustering and discrete wavelet transform. IEEE J Biomed Health Inform 24(10):2825–2832. https://doi.org/10.1109/JBHI.2020.2973982
Fotoohinasab A, Hocking T, Afghah F (2021) A greedy graph search algorithm based on changepoint analysis for automatic QRS complex detection. Comput Biol Med 130:104208. https://doi.org/10.1016/COMPBIOMED.2021.104208
Coast DA, Stern RM, Cano GG, Briller SA (1990) An approach to cardiac arrhythmia analysis using hidden Markov models. IEEE Trans Biomed Eng 37(9):826–836. https://doi.org/10.1109/10.58593
Kohler B-U, Hennig C, Orglmeister R (2002) The principles of software QRS detection. IEEE Eng Med Biol Mag 21(1):42–57. https://doi.org/10.1109/51.993193
Silipo R, Marchesi C (1998) Artificial neural networks for automatic ECG analysis. IEEE Trans Signal Process 46(5):1417–1425. https://doi.org/10.1109/78.668803
Kohler BU, Hennig C, Orglmeister R (2003) QRS detection using zero crossing counts. Appl Genomics Proteomics 2(2):138–145
Nyquist H (1928) Certain topics in telegraph transmission theory. Trans Am Inst Electr Eng 47(2):617–644. https://doi.org/10.1109/T-AIEE.1928.5055024
Ajdaraga E, Gusev M (2017) Analysis of sampling frequency and resolution in ECG signals. In: 2017 25th Telecommunication Forum (TELFOR), pp. 1–4. IEEE. https://doi.org/10.1109/TELFOR.2017.8249438
Bailey JJ, Berson AS, Garson A Jr, Horan LG, Macfarlane PW, Mortara DW, Zywietz C (1990) Recommendations for standardization and specifications in automated electrocardiography: bandwidth and digital signal processing. A report for health professionals by an ad hoc writing group of the committee on electrocardiography and cardiac electrophysiology of the council on clinical cardiology, American heart association. Circulation 81(2):730–739
Malik M (1996) Task force of the European society of cardiology and the North American society of pacing and electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Eur Heart J 17:354–381
Goldberger AL, Amaral LAN, Glass L, Hausdorff JM, Ivanov PC, Mark RG, Mietus JE, Moody GB, Peng CK, Stanley HE (2000) PhysioBank, physiotoolkit, and physionet–components of a new research resource for complex physiologic signals. Circulation 101:E215–E220
Amann A, Tratnig R, Unterkofler K (2006) Detecting ventricular fibrillation by time-delay methods. IEEE Trans Biomed Eng 54(1):174–177. https://doi.org/10.1109/TBME.2006.880909
Amann A, Tratnig R, Unterkofler K (2005) Reliability of old and new ventricular fibrillation detection algorithms for automated external defibrillators. Biomed Eng Online 4(1):60. https://doi.org/10.1186/1475-925X-4-60
American Heart Association (1989) AHA database. URLhttps://www.americanheart.org
Nolle FM, Badura FK, Catlett JM, Bowser RW, Sketch MH (1986) CREI-GARD, a new concept in computerized arrhythmia monitoring systems. Comput Cardiol 13:515–518
Laguna P, Mark RG, Goldberg A, Moody GB (1997) A database for evaluation of algorithms for measurement of QT and other waveform intervals in the ECG. In: Computers in Cardiology, IEEE. https://doi.org/10.1109/CIC.1997.648140
Behar JA, Bonnemains L, Shulgin V, Oster J, Ostras O, Lakhno I (2019) Noninvasive fetal electrocardiography for the detection of fetal arrhythmias. Prenat Diagn 39(3):178–187. https://doi.org/10.1002/PD.5412
Penzel T, Moody GB, Mark RG, Goldberger AL, Peter JH (2000) The apnea-ECG database. In: Computers in cardiology 2000. Vol. 27 (Cat. 00CH37163), pp. 255–258. IEEE, https://doi.org/10.1109/CIC.2000.898505
Andreotti F, Behar J, Zaunseder S, Oster J, Clifford GD (2016) An open-source framework for stress-testing non-invasive fetal ECG extraction algorithms. Physiol Meas 37(5):627
Iyengar N, Peng CK, Morin R, Goldberger AL, Lipsitz LA (1996) Age-related alterations in the fractal scaling of cardiac interbeat interval dynamics. Am J Physiology-Regulatory, Integr Comp Physiol 271(4):R1078–R1084. https://doi.org/10.1152/AJPREGU.1996.271.4.R1078
Baim DS, Colucci WS, Scott Monrad E, Smith HS, Wright RF, Lanoue A, Gauthier DF, Ransil BJ, Grossman W, Braunwald E (1986) Survival of patients with severe congestive heart failure treated with oral milrinone. J Am Coll Cardiol 7(3):661–670. https://doi.org/10.1016/S0735-1097(86)80478-8
Albrecht P (1983) ST segment characterization for long term automated ECG analysis. PhD diss., Massachusetts Institute of Technology, Department of Electrical Engineering and Computer Science
Moody GB, Mark RG (2001) The impact of the MIT-BIH arrhythmia database. IEEE Eng Med Biol Mag 20(3):45–50. https://doi.org/10.1109/51.932724
Moody G (1983) A new method for detecting atrial fibrillation using RR intervals. Comput Cardiol 227–230
Taddei A, Distante G, Emdin M, Pisani P, Moody GB, Zeelenberg C, Marchesi C (1992) The European ST-T database: standard for evaluating systems for the analysis of ST-T changes in ambulatory electrocardiography. Eur Heart J 13(9):1164–1172. https://doi.org/10.1093/OXFORDJOURNALS.EURHEARTJ.a060332
Bousseljot R, Kreiseler D, Schnabel A (1995) Nutzung der EKG-Signaldatenbank CARDIODAT der PTB über das Internet. Biomedizinische technik/Biomed Eng 40(s1):317–318. https://doi.org/10.1515/BMTE.1995.40.s1.317
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All Authors of this work declare no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tripathi, P.M., Kumar, A., Komaragiri, R. et al. A Review on Computational Methods for Denoising and Detecting ECG Signals to Detect Cardiovascular Diseases. Arch Computat Methods Eng 29, 1875–1914 (2022). https://doi.org/10.1007/s11831-021-09642-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11831-021-09642-2