Abstract
Purpose
Having a mental illness increases risk of mortality for women with breast cancer, partly due to barriers to accessing recommended care (e.g., cancer screening). Early detection is one important factor in breast cancer survival. To further understand this disparity in survival, we examined whether older women with mental illness are more likely to be diagnosed with later-staged breast cancers compared to women without mental illnesses.
Methods
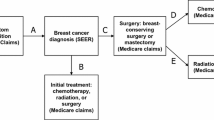
We used 2005–2015 SEER-Medicare data to identify AJCC stage I–IV breast cancer patients with and without a history of mental illness prior to cancer diagnosis. We used generalized ordinal regression to examine associations between mental illness diagnoses and stage at diagnosis, controlling for age, race/ethnicity, income, comorbidities, primary care use, rurality, and marital status.
Results
Among 96,034 women with breast cancer, 1.7% have a serious mental illness (SMI), 19.9% depression or anxiety, and 7.0% other mental illness. Those with SMI have 40% higher odds of being diagnosed with AJCC Stages II, III than Stage I; women with depression/anxiety have 25% lower odds of being diagnosed with Stage IV cancer than Stage I; and women with other mental illnesses have similar odds of being diagnosed in later stages.
Conclusion
Women with SMI have higher odds of being diagnosed at later stages, which likely contributes to higher mortality after breast cancer. Surprisingly, women with depression and anxiety have a lower risk of being diagnosed with Stage IV cancer. Earlier breast cancer diagnosis in women with SMI is an important goal for reducing disparities breast cancer survival.

Similar content being viewed by others
Data availability
The datasets analyzed during the current study are not publicly available nor are they able to be shared by the corresponding author due to the data use agreement. Access to this data is managed through the SEER-Medicare program through the National Cancer Institute. These data are available by request through the SEER-Medicare program (https://healthcaredelivery.cancer.gov/seermedicare/obtain/).
References
Viron MJ, Stern TA (2010) The impact of serious mental illness on health and healthcare. Psychosomatics 51:458–465. https://doi.org/10.1016/S0033-3182(10)70737-4
Iglay K, Santorelli ML, Hirshfield KM et al (2017) Diagnosis and treatment delays among elderly breast cancer patients with pre-existing mental illness. Breast Cancer Res Treat 166:267–275. https://doi.org/10.1007/s10549-017-4399-x
Dalton SO, Suppli NP, Ewertz M et al (2018) Impact of schizophrenia and related disorders on mortality from breast cancer: a population-based cohort study in Denmark, 1995–2011. Breast 40:170–176. https://doi.org/10.1016/j.breast.2018.06.002
Ni L, Wu J, Long Y et al (2019) Mortality of site-specific cancer in patients with schizophrenia: a systematic review and meta-analysis. BMC Psychiatry 19:323. https://doi.org/10.1186/s12888-019-2332-z
Ribe AR, Laurberg T, Laursen TM et al (2016) Ten-year mortality after a breast cancer diagnosis in women with severe mental illness: a Danish population-based cohort study. PLoS ONE 11:e0158013. https://doi.org/10.1371/journal.pone.0158013
Corrigan PW, Markowitz FE, Watson AC (2004) Structural levels of mental illness stigma and discrimination. Schizophr Bull 30:481
Shefer G, Henderson C, Howard LM et al (2014) Diagnostic overshadowing and other challenges involved in the diagnostic process of patients with mental illness who present in emergency departments with physical symptoms—a qualitative study. PLoS ONE 9:e111682. https://doi.org/10.1371/journal.pone.0111682
Weinstein L, Stefancic A, Cummingham AT et al (2016) Cancer screening, prevention, and treatment in people with mental illness. CA Cancer J Clin 66:133–151. https://doi.org/10.3322/caac.21334
SEER*Explorer Application. https://seer.cancer.gov/explorer/application.html?site=55&data_type=4&graph_type=5&compareBy=stage&chk_stage_104=104&chk_stage_105=105&chk_stage_106=106&series=age_range&chk_age_range_1=1&chk_age_range_157=157&sex=3&race=1&advopt_precision=1&advopt_display=2#fnote_methodology. Accessed 01 Sep 2022
Early cancer diagnosis saves lives, cuts treatment costs. https://www.who.int/news/item/03-02-2017-early-cancer-diagnosis-saves-lives-cuts-treatment-costs. Accessed 11 Apr 2021
ACS Breast Cancer Early Detection Recommendations. https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html. Accessed 9 Apr 2021
Jensen LF, Pedersen AF, Bech BH et al (2016) Psychiatric morbidity and non-participation in breast cancer screening. Breast 25:38–44. https://doi.org/10.1016/j.breast.2015.10.002
Carney CP, Jones LE (2006) The influence of type and severity of mental illness on receipt of screening mammography. J Gen Intern Med 21:1097–1104. https://doi.org/10.1111/j.1525-1497.2006.00565.x
Thomas M, James M, Vittinghoff E et al (2018) Mammography among women with severe mental illness: exploring disparities through a large retrospective cohort study. Psychiatr Serv 69:48–54. https://doi.org/10.1176/appi.ps.201600170
Hwong A, Wang K, Bent S, Mangurian C (2020) Breast cancer screening in women with schizophrenia: a systematic review and meta-analysis. Psychiatr Serv 71:263–268. https://doi.org/10.1176/appi.ps.201900318
Richards M, Westcombe A, Love S et al (1999) Influence of delay on survival in patients with breast cancer: a systematic review. The Lancet 353:1119–1126. https://doi.org/10.1016/S0140-6736(99)02143-1
Céspedes P, Sánchez-Martínez V, Lera-Calatayud G et al (2019) Delay in the diagnosis of breast and colorectal cancer in people with severe mental disorders. Cancer Nurs. https://doi.org/10.1097/NCC.0000000000000727
Goodwin JS, Zhang DD, Ostir GV (2004) Effect of depression on diagnosis, treatment, and survival of older women with breast cancer. J Am Geriatr Soc 52:106–111
National Cancer Institute About the SEER Program. https://seer.cancer.gov/about/. Accessed 12 Apr 2019
Centers for Medicare and Medicaid Services Research—General Information | CMS. https://www.cms.gov/research-statistics-data-and-systems/research/researchgeninfo. Accessed 4 Apr 2021
Warren JL, Klabunde CN, Schrag D et al (2002) Overview of the SEER-medicare data: content, research applications, and generalizability to the united states elderly population. Med Care 40:3–18
Enewold L, Parsons H, Zhao L et al (2020) Updated overview of the SEER-medicare data: enhanced content and applications. J Natl Cancer Inst Monogr 2020:3–13. https://doi.org/10.1093/jncimonographs/lgz029
Narod SA, Iqbal J, Giannakeas V et al (2015) Breast cancer mortality after a diagnosis of ductal carcinoma in situ. JAMA Oncol 1:888. https://doi.org/10.1001/jamaoncol.2015.2510
Condition Categories - Chronic Conditions Data Warehouse. https://www.ccwdata.org/web/guest/condition-categories. Accessed 19 Apr 2019
Mallet J, Dubertret C, Huillard O (2017) Clinical diagnosis of mental disorders before cancer diagnosis. JAMA Oncol 3:565–566. https://doi.org/10.1001/jamaoncol.2016.5293
Figueroa JF, Phelan J, Orav EJ et al (2020) Association of mental health disorders with health care spending in the medicare population. JAMA Netw Open 3:e201210–e201210
SAMHSA Behavioral Health Spending and Use Accounts, 1986–2014 | Publications and Digital Products
Boyd RW, Lindo EG, Weeks LD, McLemore MR (2020) On racism: a new standard for publishing on racial health inequities. Health Affairs Blog 10:1
National Cancer Institute, Division of Cancer Control and Population Sciences Comorbidity SAS Macro (2014 version). https://healthcaredelivery.cancer.gov/seermedicare/considerations/macro-2014.html. Accessed 3 Dec 2020
Ferrante JM, Lee J-H, McCarthy EP et al (2013) Primary care utilization and colorectal cancer incidence and mortality among medicare beneficiaries. Ann Intern Med 159:437–446. https://doi.org/10.7326/0003-4819-159-7-201310010-00003
Roetzheim RG, Ferrante JM, Lee J-H et al (2012) Influence of primary care on breast cancer outcomes among medicare beneficiaries. Ann Family Med 10:401–411. https://doi.org/10.1370/afm.1398
Lyratzopoulos G, Abel GA, Barbiere JM et al (2012) Variation in advanced stage at diagnosis of lung and female breast cancer in an English region 2006–2009. Br J Cancer 106:1068–1075. https://doi.org/10.1038/bjc.2012.30
Tarlov E, Zenk SN, Campbell RT et al (2009) Characteristics of mammography facility locations and stage of breast cancer at diagnosis in Chicago. J Urban Health 86:196–213. https://doi.org/10.1007/s11524-008-9320-9
Desai MM, Bruce ML, Kasl SV (1999) The effects of major depression and phobia on stage at diagnosis of breast cancer. Int J Psychiatry Med 29:29–45. https://doi.org/10.2190/0C63-U15V-5NUR-TVXE
Aggarwal A, Pandurangi A, Smith W (2013) Disparities in breast and cervical cancer screening in women with mental illness: a systematic literature review. Am J Prev Med 44:392–398. https://doi.org/10.1016/j.amepre.2012.12.006
Murphy KA, Stone EM, Presskreischer R et al (2021) Cancer screening among adults with and without serious mental illness: a mixed methods study. Med Care 59:327–333. https://doi.org/10.1097/MLR.0000000000001499
Clifton A, Burgess C, Clement S et al (2016) Influences on uptake of cancer screening in mental health service users: a qualitative study. BMC Health Serv Res 16:257. https://doi.org/10.1186/s12913-016-1505-4
Ward MC, Druss BG (2017) Reverse integration initiatives for individuals with serious mental illness. Focus 15:271–278. https://doi.org/10.1176/appi.focus.20170011
Barley EA, Borschmann RD, Walters P, Tylee A (2016) Interventions to encourage uptake of cancer screening for people with severe mental illness. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009641.pub3
Drake RE, Deegan PE, Rapp C (2010) The promise of shared decision making in mental health. Psychiatr Rehabil J 34:7–13. https://doi.org/10.2975/34.1.2010.7.13
van der Krieke L, Emerencia AC, Boonstra N et al (2013) A web-based tool to support shared decision making for people with a psychotic disorder: randomized controlled trial and process evaluation. J Med Internet Res 15:e216. https://doi.org/10.2196/jmir.2851
Weinstein LC, LaNoue M, Hurley K et al (2015) Using concept mapping to explore barriers and facilitators to breast cancer screening in formerly homeless women with serious mental illness. J Health Care Poor Underserved 26:908–925. https://doi.org/10.1353/hpu.2015.0104
Weinstein L, LaNoue M, Hurley K et al (2019) Feasibility pilot outcomes of a mammography decision support and navigation intervention for women with serious mental illness living in supportive housing settings. J Prim Care Community Health. https://doi.org/10.1177/2150132719867587
NIMH » Mental Illness. https://www.nimh.nih.gov/health/statistics/mental-illness.shtml. Accessed 13 Feb 2019
Cancer Testing Covered by Medicare—SEER-Medicare. https://healthcaredelivery.cancer.gov/seermedicare/considerations/testing.html. Accessed 7 Apr 2022
Acknowledgements
Authors thank Drs Jeylan Mortimer and Nathan Shippee for their contributions to this work. This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
Funding
This research was supported by the National Cancer Institute of the National Institutes of Health [Award Number: T32CA163184 (Michele Allen, MD, MS, PI)] and the University of Minnesota’s Consortium of Law and Values, the Human in the Data MN-Drive Award, and the Minnesota Population Center Development Award.
Author information
Authors and Affiliations
Contributions
MB and DM worked on all parts of this project, from conceptualization to submission. DM additionally supervised this work. HP assisted in data curation, formal analysis, methodology, and writing. HP, AB, and KC assisted in conceptualization and writing.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bhattacharya, M., Parsons, H., Call, K. et al. Impact of a pre-existing diagnosis of mental illness on stage of breast cancer diagnosis among older women. Breast Cancer Res Treat 197, 201–210 (2023). https://doi.org/10.1007/s10549-022-06793-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06793-z



