Abstract
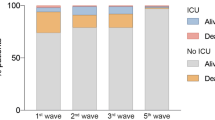
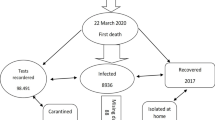
The objective of this study is to analyze the characteristics of patients who died in the Hospital Emergency Department (HED) of a Spanish third-level hospital, with a special focus on those who died due to SARS-CoV-2. A retrospective cohort study was conducted, including all patients over 18 years old who died in the Hospital Emergency Department (HED) of a Spanish third-level hospital located in Badalona, Spain, from Jun 2019 to Dec 2020. Various sociodemographic, clinical, and diagnostic variables of the patients were analyzed to identify potential risk factors associated with mortality. During the first wave of the COVID-19 pandemic, a total of 72 patients died in the HED, representing a 42% increase compared to the pre-pandemic period. Of the deceased patients, 11% were attributed to SARS-CoV-2. Furthermore, it was found that patients who died from SARS-CoV-2 during the first wave were significantly younger than those in the second wave, with an average age of 78.6 ± 3.1 years in the first wave and 91.8 ± 4.8 years in the second wave. No significant differences were found regarding gender or associated comorbidities. Overall, the mortality rate at the HED in relation to COVID-19 was low, and infected patients died at younger ages during the first wave compared to the second wave.


Similar content being viewed by others
References
Rodríguez Maroto O, Llorente Álvarez S, Casanueva Gutierrez M, Álvarez Álvarez B, Menéndez Somoano P, Riva MG (2004) Mortalidad en un Servicio de Urgencias Hospitalarias. Características clínico epidemiológicas Emergencias 16:17–22
Stefanovski PH, Vladimir Radkov R, Lyubomir Ilkov T, Pencho Tonchev T, Yoana Mladenova T, Vihar Manchev K, Radko Nikolov R (2017) Analysis of mortality in the emergency department at a university hospital in Pleven. J Int Med Res 45(5):1553–1561. https://doi.org/10.1177/0300060517707901
Vázquez-García D, Rica-Escuín M, Germán-Bes C, Caballero-Navarro AL (2020) Características epidemiológicas de los pacientes fallecidos en los servicios de urgencias hospitalarias del sistema aragonés de salud y su relación con el índice comorbilidad. Emergencias 32:162–168
Richardson PG, Greenslade J, Isoardi J, Davey M, Gillett M, Tucker A et al (2016) End-of-life issues: withdrawal and withholding of life-sustaining healthcare in the emergency department: a comparison between emergency physicians and emergency registrars: a sub-study. Emerg Med Australas 28:684–690
Parra-Caballero P, Curbelo-García JJ, Gullón-Ojesto A, Ruiz-Giménez Arrieta N, Suárez-Fernández C, Del Arco-Galán C (2011) Mortalidad precoz en un hospital terciario: análisis de la calidad asistencial. Emergencias 23:430–436
Le Conte P, Riochet D, Batard E, Volteau C, Giraudeau B, Arnaudet I et al (2010) Death in emergency departments: a multicenter cross-sectional survey with analysis of withholding and withdrawing life support. Intensive Care Med 36:765–772
VanTricht M, Riochet D, Batard E, Martinage A, Montassier E, Potel G et al (2012) Palliative care for patients who died in emergency depart- ments : analysis of a multicentre cross-sectional survey. Emerg Med J 29:795–797
Aylin P, Yunus A, Bottle A, Majeed A, Bell D (2010) Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 19(3):213–217. https://doi.org/10.1136/qshc.2008.028639
Informe no 59. Situación de COVID-19 en España. Casos diagnosticados a partir 10 de mayo. https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Paginas/Informes_Previos_COVID-19_2020.aspx
Las 10 principales causas de defunción. https://www.who.int/es/news-room/fact-sheets/detail/the-top-10-causes-of-death
Srivastava N, Baxi P, Ratho RK, Saxena SK. Global Trends in Epidemiology of Coronavirus Disease 2019 (COVID-19). SK Saxena (ed), Coronavirus Disease 2019 (COVID-19) Medical Virology: from Pathogenesis to Disease Control. 2020:9–21
COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. https://www.COVID19treatmentguidelines.nih.gov/overview/overview-of-COVID-19/
Bases para un modelo catalán de atención a las personas con necesidades complejas. Conceptualización e introducción a los elementos operativos. Versión 6.0 del 27 de marzo de 2017. https://scientiasalut.gencat.cat/bitstream/handle/11351/3305/bases_modelo_catalan_atencion_personas_necesidades_complejas_2017_cas.pdf?sequence=5
Clasificación Internacional de Enfermedades 10.ª revisión, modificación clínica. Edición Española. https://eciemaps.mscbs.gob.es/ecieMaps/browser/index_10_mc.html.
Miró O, De Dios A, Antonio MT, Sánchez M, Borrás A, Millá J (1999) Estudio de la mortalidad en un servicio de urgencias hospitalario: incidencias, causas y consecuencias. Med Clin (Barc) 112:690–692
Sahuquillo Llamas JC, Tudela Hita P, Segura Egea A, Estrada CO (2000) Análisis de la mortalidad en el Servicio de Urgencias de un Hospital General. Emergencias. 12:377
Instituto Nacional de Estadística. https://www.ine.es/ss/Satellite?L=es_ES&c=INESeccion_C&cid=1259944484459&p=1254735110672&pagename=ProductosYServicios%2FPYSLayout¶m1=PYSDetalleFichaIndicador¶m3=1259947308577
Zhang JJ, Dong X, Liu GH, Gao YD (2023) Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol 64(1):90–107. https://doi.org/10.1007/s12016-022-08921-5. (Epub 2022 Jan 19. PMID: 35044620; PMCID: PMC8767775)
Pérez López FR, Tajada M, Savirón Cornudella R, Sanchez-Prieto M, Chedrauie P, Teráng E (2020) Coronavirus disease 2019 and gender-related mortality in European countries: a meta-analysis. Maturitas 141:59–62
Dorrucci M, Minelli G, Boros S, Manno V, Prati S, Battaglini M, Corsetti G, Andrianou X, Riccardo F, Fabiani M, Vescio MF, Spuri M, Urdiales AM, Martina DM, Onder G, Pezzotti P, Bella A (2021) Excess mortality in italy during the COVID-19 pandemic: assessing the differences between the first and the second wave, year 2020. Front Public Health 16(9):669209. https://doi.org/10.3389/fpubh.2021.669209.PMID:34336767;PMCID:PMC8322580
Yuan X-L, Du X-Y, Ding N (2022) A retrospective analysis of mortality in a Beijing hospital Emergency Department. Ann Ital Chir 93:453–456
Chavez-MacGregor M, Lei X, Zhao H, Scheet P, Giordano SH (2022) Evaluation of COVID-19 mortality and adverse outcomes in us patients with or without cancer. JAMA Oncol 8(1):69–78. https://doi.org/10.1001/jamaoncol.2021.5148.PMID:34709356;PMCID:PMC8554684
Naimi A, Yashmi I, Jebeleh R, Imani Mofrad M, Azimian Abhar S, Jannesar Y, Heidary M, Pakzad R (2022) Comorbidities and mortality rate in COVID-19 patients with hematological malignancies: a systematic review and meta-analysis. J Clin Lab Anal 36(5):e24387. https://doi.org/10.1002/jcla.24387. (Epub 2022 Apr 6. PMID: 35385130; PMCID: PMC9102765)
Aboueshia M, Hussein MH, Attia AS, Swinford A, Miller P, Omar M, Toraih EA, Saba N, Safah H, Duchesne J, Kandil E (2021) Cancer and COVID-19: analysis of patient outcomes. Future Oncol 17(26):3499–3510. https://doi.org/10.2217/fon-2021-0121. (Epub 2021 Jul 15. PMID: 34263660; PMCID: PMC8284249)
Kyoung DS, Lee J, Nam H, Park MH (2021) Dementia and COVID-19 Mortality in South Korea. Dement Neurocogn Disord 20(3):38–40. https://doi.org/10.12779/dnd.2021.20.3.38. (Epub 2021 May 31. PMID: 34354756; PMCID: PMC8326307)
Wang Q, Davis PB, Gurney ME, Xu R (2021) COVID-19 and dementia: analyses of risk, disparity, and outcomes from electronic health records in the US. Alzheimers Dement 17(8):1297–1306. https://doi.org/10.1002/alz.12296. (Epub 2021 Feb 9. PMID: 33559975; PMCID: PMC8014535)
Dadras O, SeyedAlinaghi S, Karimi A, Shamsabadi A, Qaderi K, Ramezani M, Mirghaderi SP, Mahdiabadi S, Vahedi F, Saeidi S, Shojaei A, Mehrtak M, Azar SA, Mehraeen E, Voltarelli FA (2022) COVID-19 mortality and its predictors in the elderly: a systematic review. Health Sci Rep 5(3):e657. https://doi.org/10.1002/hsr2.657.Erratum.In:HealthSciRep.2022Jul21;5(4):e723.PMID:35620541;PMCID:PMC9125886
Torres-Cantero AM, Álvarez León EE, Morán-Sánchez I, San Lázaro Campillo I, Bernal Morell E, Hernández Pereña M, Martínez-Morata I (2022) El impacto de la pandemia de COVID-19 sobre la salud. Informe SESPAS 2022 [Health impact of COVID pandemic. SESPAS Report 2022]. Gac Sanit 36(Suppl 1):S4–S12. https://doi.org/10.1016/j.gaceta.2022.02.008. (PMID: 35781147; PMCID: PMC9244867)
Funding
There is no funding or financial support in relation to the present study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflict of interest.
Ethical approval
All authors have confirmed the maintenance of confidentiality and respect for patient’s rights in the authorship responsibilities document, publication agreement, and rights transfer to Internal and Emergency Medicine.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sanlés-González, I., Grimal-Abejez, L., Serrat-Muñoz, J. et al. Characteristics of patients who died in the hospital emergency service during the SARS-CoV-2 pandemic: a retrospective cohort study in a tertiary hospital in Spain. Intern Emerg Med (2024). https://doi.org/10.1007/s11739-023-03519-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-023-03519-x