Abstract
Background
COVID-19 now exists for more than 3 years and has caused almost 7 million deaths worldwide. At the beginning of this study only little was known on the patients’ characteristics and comparative autopsy studies are still rare.
Material and methods
Between 11 March 2020 and 10 March 2021, 55 consecutive and complete autopsies of individuals who died in association with SARS-CoV‑2 infections were performed shortly after death (median PMI 6.8 h) by the same team. Clinical data were available in 45 of 55 cases. 1st vs. 2nd infection wave cases and male vs. female cases were compared.
Results
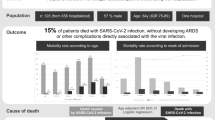
Thirty-five patients were male (63.6%) 20 were female (36.4%), average age 72.4 years. Seventeen cases (30.9%) could be assigned to the 1st and 38 cases (69.1%) to the 2nd infection wave. Forty-two of the decedents (76.4%) died due to COVID-19. Arterial hypertension, obesity, and cardiac hypertrophy were the most frequent detected comorbidities.
Discussion
The present study corroborates previous research data but also reveals new approaches for further comparative studies. Patient-specific personal and general ICU-related risk factors for the development of thromboembolisms oppose the effects of changes in anticoagulant medication.
Zusammenfassung
Hintergrund
Seit mehr als 3 Jahren verursachte COVID-19 bislang weltweit fast 7 Mio. Todesfälle. Zu Beginn dieser Studie war vergleichsweise wenig über die Charakteristika dieser Patienten bekannt und vergleichende Obduktionsstudien existieren bislang kaum.
Material und Methoden
Zwischen dem 11. März 2020 und dem 10. März 2021 wurden 55 Personen, die im Zusammenhang mit SARS-CoV-2-Infektionen verstarben, von dem selben Team vollständig obduziert. Die Obduktionen wurden kurz nach dem Tod durchgeführt (medianer PMI 6,8 h). In 45 von 55 Fällen waren zudem klinische Daten verfügbar. Verglichen wurden Fälle der ersten und zweiten Infektionswelle sowie männliche und weibliche Patienten.
Ergebnisse
35 Patienten waren männlich (63,6 %) und 20 weiblich (36,4 %); das Durchschnittsalter betrug 72,4 Jahre. 17 Fälle (30,9 %) konnten der ersten und 38 Fälle (69,1 %) der zweiten Infektionswelle zugeordnet werden. 42 Verstorbene (76,4 %) starben direkt an COVID-19. Arterielle Hypertonie, Adipositas und Herzhypertrophie waren die am häufigsten nachgewiesenen Vorerkrankungen.
Diskussion
In Bezug auf die Hauptcharakteristika der COVID-19-Todesfälle bestätigen die Ergebnisse der vorliegenden Studie im Wesentlichen bisherige Forschungsdaten, zeigten aber auch neue Ansätze für weitere Vergleichsstudien auf. Patientenspezifische persönliche und allgemeine intensivmedizinische Risikofaktoren für die Entwicklung von Thrombembolien stehen den Auswirkungen einer Änderung der gerinnungshemmenden Medikation entgegen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) is an RNA virus that causes the coronavirus disease 2019 (COVID-19) [24]. Since its first description in Wuhan, China, in December 2019, it rapidly spread all over the world. On March 11 2020, the World Health Organization (WHO) “made the assessment that COVID-19 can be characterized as a pandemic” [5]. In the following months, the incidence of COVID-19 cases in Germany showed a wave-like course, similar to other viral respiratory diseases. Until today (Spring 2023) nearly 7 million people died from or in association with a SARS-CoV‑2 infection worldwide, of which approximately 170,000 died in Germany [40].
Scientific literature on COVID-19 autopsies ranges from single case reports to autopsy studies with over 700 patients [10, 39]. To reduce the transmission of virus containing aerosols some research groups used postmortem imaging and minimally invasive techniques or partial/incomplete autopsies [19, 26], but many centers also conducted a number of conventional full autopsies (Table 1). These examinations were usually performed within time intervals of only a few hours up to 10 days after death with an average post-mortem interval (PMI) of a few days [41, 43]. The decedents were predominantly male, elderly (average age at death approx. 50–80 years) and overweight, suffering from multiple preconditions such as cardiovascular diseases, chronic pulmonary diseases, and diabetes [13, 17]. The most reported post-mortem organ findings concerned the lungs, mainly in the form of lung fibrosis and diffuse alveolar damage (DAD), followed by affections of the kidneys and the liver that finally often led to fatal multiple organ failure [8, 22]. In addition, (micro-) thromboembolism, particularly within the pulmonary vessels, were frequently observed [7, 12, 17].
Comparative studies between study samples of different infection waves are still rare [3, 20] and often consider single organs only [11, 42]. Hence, the present retrospective study compares the autopsy findings encountered during the first and second infection wave in Germany as well as the differences between male and female patients. Thereby, the study primarily aims at the characterization of individuals, who died in association with a SARS-CoV‑2 infection, including the identification of the substantial comorbidities. Furthermore, the effects of different therapeutical measures during different times of the first year of the COVID-19 pandemic is analyzed.
Materials and methods
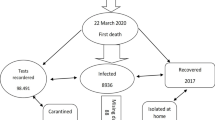
With approval of the local ethical board (registration number 2020-1773), 55 consecutive autopsies of individuals, who died in association with a SARS-CoV‑2 infection, were performed at the Institute of Forensic Medicine of the Jena University Hospital between 11 March 2020 and 10 March 2021. Except for two, in all patients SARS-CoV‑2 was detected by naso-pharyngeal swab testing prior to death. While all clinical cases were tested by PCR, this knowledge was only available to a limited extent in forensic and private cases. Based on the phase classification of the Robert Koch Institute Berlin (German public health institute for investigation and prevention of infectious diseases), two ‘infection waves’ (dynamics of the official nation-wide SARS-CoV‑2 case detection) were defined [32]: autopsy cases from 11 March 2020 to 31 July 2020 were assigned to the ‘first infection wave’ and cases from 1 October 2020 to 10 March 2021 to the ‘second infection wave’.
The study group finally included the following types of autopsies:
-
1.
Clinical autopsies of deceased patients from the Jena University Hospital and 4 regional hospitals located in the German Federal State of Thuringia (n = 45).
-
2.
“Private” autopsies requested by public health departments or a family member of the deceased (n = 3).
-
3.
Forensic autopsies requested by departments of public prosecution of the German Federal State of Thuringia (n = 7).
All cases were autopsied as soon as possible after death in order to achieve a very short post-mortem interval (PMI; time between death and autopsy), facilitating optimal morphological post-mortem diagnostics due to minimal tissue degradation, even in tissues that usually loose histomorphological quality very fast (e.g. gastrointestinal samples). A short PMI was essentially achieved by close and reliable cooperation between all players involved (ICUs, forensic department, and the patient’s relatives). Clinical autopsies were conducted with consent of the relatives only. All autopsies were complete autopsies, i.e. post-mortem examination of all internal organs and tissues of all body cavities, and performed by the same team. The leg vessels were autopsied only if thromboembolisms had previously been found in other organs or vessels. The main objectives of the autopsies were the determination of the cause of death, the recording of findings possibly typical (or even specific) for COVID-19, and the detection of the morphological comorbidities.
During each autopsy, a total of at least 60 tissue and organ samples were collected for comprehensive histological and immunohistochemical analyses.
After autopsy, a categorization of SARS-CoV‑2 positive deaths was done according to a modification of the proposal by Edler et al. (2020) [4]:
-
Category 1: Death is due to COVID-19 alone.
-
Category 2: Death is due to COVID-19 and due to at least one another severe disease.
-
Category 3: Death is not due to the detected SARS-CoV‑2 infection.
-
Category 4: Cause of death is undetermined.
In addition, medical records, including clinical data and metadata on the deceased patients, were respectively provided by the participating clinical institutions and the customers of the autopsies. These data included information on diagnosis and treatment, police investigation results, and death certificates. Medical records were completely available in 45 of the 55 cases. In forensic and private autopsy cases, the collection of such information was not possible or only possible to a limited extent.
Statistical analyses were performed with MS Excel 16 (Version 2301, 2023), IBM SPSS Statistics 27 (2020), IDL 8.8.0 (2020), and GraphPad Prism 4.00 (2003). P‑values were calculated using the Fisher-Yates test and student’s t‑test. P-values < 0.05 were considered statistically significant.
Results
Total study sample
The general characteristics of the study sample are shown in Table 2. Out of the 55 SARS-CoV-2-associated death cases autopsied 35 cases (63.6%) were male, and 20 cases (36.4%) were female, predominantly in older age (median 77.2 years). The PMI was very low (median 6.8 h), and even lower when considering the clinical autopsy cases only (81.8% of the cases, median 5.2 h). Most patients (43 cases, 78.2%) died on an Intensive Care Unit (ICU).
The medical diagnoses determined at autopsy are summarized in Table S1. The vast majority of the present patient sample (37 cases, 67.3%) died directly from a COVID-19 pneumonia, accordingly, classified as category 1 (38 cases, 69.1%). One fatality of category 1 was due to pulmonary embolism alone. Four patients (7.3%) died from a combination of COVID-19 with another severe disease (e.g. intracerebral hemorrhage) and were classified as category 2. In 10 cases (18.2%), death could not unambiguously determined due to the proven SARS-CoV‑2 infection (category 3) because death was caused by another severe and concomitantly existing condition, such as drowning, or ileus due to a malignant tumor disease.
Except for three cases, all patients suffered from at least one substantial comorbidity. The three most frequent substantial comorbidities were ‘arterial hypertension’ (52.7%), ‘obesity’ (47.3%), and ‘cardiac hypertrophy’ (40.0%). Accordingly, the ‘circulatory system’ as well as the ‘endocrine and metabolic system’ were found to be the most frequent disease groups. The group of ‘malignant neoplasms’ was the third frequent group. In 10 of the 18 autopsy cases (55.6%) with a malignant tumor disease, the neoplasm was first diagnosed at autopsy. These tumors were chronic lymphocytic leukemia, endometrium carcinoma, prostate carcinomata, colorectal carcinomata, pancreatic precancer, hepatocellular carcinoma and liposarcoma. With exception for the endometrium carcinoma case, which showed evidence for lymphangiosis, no other tumor case revealed any sign of metastatic spread. In one case, the cancer diagnosis was made only a few days prior to death (cervical carcinoma).
Thromboembolic findings could be observed in 61.8% of the cases. None of the patients showed sole thromboses. Either there were no thromboembolic findings at all or a combination of thrombi and emboli.
The majority of our study group (45 cases, 81.8%) was overweight with a median body mass index (BMI) of 29.4 kg/m2.
Comparison between 1st and 2nd infection wave
A data comparison between 1st and 2nd infection wave is shown in Tables 2, S1 and S2. Seventeen cases (30.9%) could be assigned to the 1st infection wave, and 38 cases (69.1%) to the 2nd infection wave.
Concerning sex, age, place of death, and BMI, no significant differences were found between 1st and 2nd wave. In terms of the substantial comorbidities, endocrine diseases significantly predominated in the 1st wave (p = 0.007) and cardiovascular diseases in the 2nd wave (p = 0.043).
The relative case number of intubated patients in the second wave almost doubled from 41.2% (n = 7) in 1st wave to 78.6% (n = 22) in 2nd wave (p = 0.011). Considering anticoagulant and antiviral medication, the changes from Enoxaparin (p = 0.002) and Lopinavir/Ritonavir (Kaletra®) (p = 0.001) in the 1st wave to Tinzaparin (p < 0.001) and Remdesivir (p = 0.001) in the 2nd wave were striking. In addition, the number of patients treated with immunosuppressants (mainly dexamethasone) and multiple antibiotics increased significantly (p = 0.031).
Comparison between male and female patients
A data comparison between male and female patients is shown in Tables S3 and S4 and Figs. 1, 2 and 3. Even though the mean BMI was not significantly different, women tended to be overweight (mean BMI 29.5 kg/m2), while men were mostly obese (mean BMI 31.0 kg/m2) (Fig. 1). The most frequent place of death was the ICU in both groups; however, women died significantly more often on a normal ward (p = 0.045). The mean durance of hospitalization in general (19.7 days vs. 11.9 days; p = 0.043) and the length of stay in the intensive care unit (15.5 days vs. 10.8 days; p = 0.042) in particular was significantly longer in male patients.
While the majority (regardless of sex) died due to COVID-19 (74.3% of the men and 60.0% of the women), in female decedents the cause of death was not associated with COVID-19 more frequent (p = 0.017).
The most frequent comorbidities in both sexes were arterial hypertension and obesity. Men suffered from cardiac hypertrophy (p = 0.004) and coronary heart disease (p = 0.039) more often compared to women (Fig. 2). Sorted by groups, diseases of the circulatory system are the most common comorbidities in both sexes, followed by diseases of the endocrine and metabolic system and malignant neoplasms in male patients (Fig. 3).
60.0% of women (n = 12) but only 25.7% of men (n = 9) showed no thromboembolic findings at all. If thromboembolisms were found, pulmonary embolisms were observed significantly more often in male decedents (p = 0.028).
No woman but 7 men (24.1%) were intubated and artificially ventilated with ECLS (p = 0.034). In addition, the proportion of female patients with no artificial ventilation was significantly higher (p = 0.005) and men had been artificially ventilated significantly longer (p = 0.042).
Concerning medication, both groups were treated approximately equally with one exception: administration of antiviral drugs was more infrequent in females (p = 0.031), especially Lopinavir/Ritonavir (Kaletra®) (p = 0.031), which was only used in males.
Discussion
The present study focused on the determination of characteristics of 55 SARS-CoV-2-associated autopsy cases and the analysis of the effects of therapeutical measures during the first year of the COVID-19 pandemic. We were able to ensure the best possible autopsy findings by means of a median post-mortem interval (PMI) of 6.8 h, which is, to the best of our knowledge, the lowest in European and American literature on COVID-19 autopsies.
The average age of the deceased of the present study (72.4 years) corresponds to the results of other studies [1, 3]. However, this average age differs from the average age at death of other large German studies, such as in the Hamburg study by Edler et al. [7] (mean 79.2 years). This discrepancy may be due to the different study design. While “the health authorities of the districts [of the City of Hamburg] ordered autopsies for all COVID-19 deaths according to the Infection Protection Act” [35], the case sample of the present study mainly consists of clinical patients with a severe clinical course of COVID-19.
The most frequent substantial comorbidities of the present COVID-19 study sample, i.e. cardiovascular diseases, obesity and diabetes, match those of other autopsy studies (Table 1) and are common preconditions in Germany. However, it is striking that the proportion of patients suffering from arterial hypertension and from an obesity is higher in our study group than in the average German population [25, 31]. Additionally considering other publications [37], this confirms that these illnesses must highly likely be considered risk factors for a severe course of COVID-19.
Another remarkable result concerning the comorbidities of the present COVID-19 decedents is that 10 of 18 malignant neoplasms found during autopsy were unknown ante-mortem. This finding supports the hypothesis that even unknown malignancies could have considerable influence on the course of COVID-19. Since previous autopsy studies on COVID-19 only appraise active, diagnosed tumor diseases [30, 34], further investigation on this point appears to be promising.
In line with many other COVID-19 autopsy studies [8, 10, 18], the present COVID-19 study sample revealed thromboembolic findings in many different organs, primarily affecting pulmonary arteries. However, as described by Dwiputra Hernugrahanto et al. [6], even more unusual locations such as cerebral or splenic vessels could be detected as well. Despite significant changes in anticoagulant therapy, observed by comparing the 1st and 2nd infection wave, and contrary to our expectations, we observed an increase in thromboembolic findings. In 2015, a meta-analysis of Malato et al. [21] found that deep vein thrombosis (DVT) occurred in approximately 1 of 8 ICU patients. Even with exclusion of clinical studies evaluating the presence of DVTs in patients without antithrombotic medication, this percentage only slightly decreased. Furthermore, while Pereyra et al. [27] were able to show that the administration of low-molecular-weight heparin in COVID-19 patients “was associated with reduced mortality”; other non-COVID-19-related publications did not reveal any difference between the use of Tinzaparin and Enoxaparin [28, 38]. To summarize, the afore-mentioned considerations suggest that the effect of anticoagulation in critically ill patients like in the present study sample may be negated by general and ICU specific risk factors, regardless of the antithrombotic drugs (Tinzaparin or Enoxaparin) administered.
The non-significantly increased high number of thromboembolic findings in the 2nd infection wave might also be the reason why the number of our patients dying directly from COVID-19 did not decrease either. Based on the present statistics, one patient (5.9%) of the 1st wave died from a COVID-19 induced pulmonary embolism, whereas 5 patients (13.2%) of the 2nd wave showed fatal thromboembolic findings of the lungs on top of a COVID-19 pneumonia.
Inherently, the present study has some limitations. First, the case number is rather small but still one of the more extensive compared to other full autopsy studies (see Table 1). Second, our study population underlies a selection bias as it is mainly composed of clinical patients with severe courses of COVID-19. However, using this deliberately chosen study design (i.e., examining those who were apparently most affected), we hoped for obtaining a deeper understanding on the new virus disease as quick as possible. Third, control cases are missing. While the investigation of this particular study sample enabled us to record rarer complications of the disease, it also means that our results cannot be easily extrapolated to the general (German) population where mild disease courses were predominant [33].
Conclusions
-
The present study group mainly consist of elderly, obese, mostly male COVID-19 patients; nearly all of the 55 patients suffered from more than one severe comorbidity.
-
COVID-19 was the cause of death in over 75% of the patients.
-
Despite changes in medication and clinical treatment, no significant differences in terms of age, BMI, thromboembolic findings, and days in clinic respectively days on ICU were detected between decedents of the 1st and 2nd infection wave.
-
Thromboembolic events could be found in more than half of the cases (61.8%) with pulmonary embolism affecting men more frequently than women.
References
Bradley BT, Maioli H, Johnston R et al (2020) Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet 396:320–332
Carsana L, Sonzogni A, Nasr A et al (2020) Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet Infect Dis 20:1135–1140
Danics K, Pesti A, Toro K et al (2021) A COVID-19-association-dependent categorization of death causes in 100 autopsy cases. Geroscience 43:2265–2287
Deinhardt-Emmer S, Wittschieber D, Sanft J et al (2020) Early postmortem mapping of SARS-CoV‑2 RNA in patients with COVID-19 and correlation to tissue damage (bioRxiv:2020.2007.2001.182550)
https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 24 Mar 2023
Dwiputra Hernugrahanto K, Novembri Utomo D, Hariman H et al (2021) Thromboembolic involvement and its possible pathogenesis in COVID-19 mortality: lesson from post-mortem reports. Eur Rev Med Pharmacol Sci 25:1670–1679
Edler C, Schroder AS, Aepfelbacher M et al (2020) Dying with SARS-CoV‑2 infection—an autopsy study of the first consecutive 80 cases in Hamburg, Germany. Int J Legal Med 134:1275–1284
Elezkurtaj S, Greuel S, Ihlow J et al (2021) Causes of death and comorbidities in hospitalized patients with COVID-19. Sci Rep 11:4263
Falasca L, Nardacci R, Colombo D et al (2020) Postmortem findings in Italian patients with COVID-19: a descriptive full autopsy study of cases with and without comorbidities. J Infect Dis 222:1807–1815
Fitzek A, Schadler J, Dietz E et al (2021) Prospective postmortem evaluation of 735 consecutive SARS-CoV-2-associated death cases. Sci Rep 11:19342
Fortarezza F, Pezzuto F, Hofman P et al (2022) COVID-19 pulmonary pathology: the experience of European pulmonary pathologists throughout the first two waves of the pandemic. Diagnostics (Basel) 12(1):95
Fox SE, Akmatbekov A, Harbert JL et al (2020) Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med 8:681–686
Haberecker M, Schwarz EI, Steiger P et al (2022) Autopsy-based pulmonary and vascular pathology: pulmonary endotheliitis and multi-organ involvement in COVID-19 associated deaths. Respiration 101:155–165
Han B, Bhalla R, da Silva Lameira F et al (2020) Coronavirus disease 2019 autopsies and personal protective equipment. Arch Pathol Lab Med 144:1295a
Jackson NR, Zeigler K, Torrez M et al (2021) New Mexico’s COVID-19 experience. Am J Forensic Med Pathol 42:1–8
Keresztesi AA, Perde F, Ghita-Nanu A et al (2020) Post-mortem diagnosis and autopsy findings in SARS-coV‑2 infection: forensic case series. Diagnostics (Basel) 10(12):1070
Kommoss FKF, Schwab C, Tavernar L et al (2020) The pathology of severe COVID-19-related lung damage. Dtsch Ärztebl Int 117:500–506
Kyada HC, Bhalara RV, Vadgama DK et al (2022) Pathological findings in COVID-19: a conventional autopsy-based study from India. Indian J Med Res 155:178–188
Lax SF, Skok K, Zechner P et al (2020) Pulmonary arterial thrombosis in COVID-19 with fatal outcome : results from a prospective, single-center, clinicopathologic case series. Ann Intern Med 173:350–361
Maccio U, Zinkernagel AS, Schuepbach R et al (2022) Long-term persisting SARS-coV‑2 RNA and pathological findings: lessons learnt from a series of 35 COVID-19 autopsies. Front Med (Lausanne) 9:778489
Malato A, Dentali F, Siragusa S et al (2015) The impact of deep vein thrombosis in critically ill patients: a meta-analysis of major clinical outcomes. Blood Transfus 13:559–568
Martin-Martin J, Martin-Cazorla F, Suarez J et al (2022) Comorbidities and autopsy findings of COVID-19 deaths and their association with time to death: a systematic review and meta-analysis. Curr Med Res Opin 38:785–792
Menter T, Haslbauer JD, Nienhold R et al (2020) Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunction. Histopathology 77:198–209
Mohamadian M, Chiti H, Shoghli A et al (2021) COVID-19: virology, biology and novel laboratory diagnosis. J Gene Med 23:e3303
Neuhauser HK, Adler C, Rosario AS et al (2015) Hypertension prevalence, awareness, treatment and control in Germany 1998 and 2008–11. J Hum Hypertens 29:247–253
Nunes MC, Hale MJ, Mahtab S et al (2022) Clinical characteristics and histopathology of COVID-19 related deaths in South African adults. PLoS ONE 17:e262179
Pereyra D, Heber S, Schrottmaier WC et al (2021) Low-molecular-weight heparin use in coronavirus disease 2019 is associated with curtailed viral persistence: a retrospective multicentre observational study. Cardiovasc Res 117:2807–2820
Planes A, Samama MM, Lensing AW et al (1999) Prevention of deep vein thrombosis after hip replacement—comparison between two low-molecular heparins, tinzaparin and enoxaparin. Thromb Haemost 81:22–25
Puelles VG, Lutgehetmann M, Lindenmeyer MT et al (2020) Multiorgan and renal tropism of SARS-CoV‑2. N Engl J Med 383:590–592
Schaller T, Hirschbuhl K, Burkhardt K et al (2020) Postmortem examination of patients with COVID-19. JAMA 323:2518–2520
Schienkiewitz A, Kuhnert R, Blume M et al (2022) Overweight and obesity among adults in Germany—results from GEDA 2019/2020-EHIS. J Health Monit 7:21–28
Schilling JBS, Tolksdorf K (2022) Zweite Aktualisierung der „Retrospektiven Phaseneinteilung der COVID-19-Pandemie in Deutschland“. Epidemiol Bull 10:3–5
Schilling J, Tolksdorf K, Marquis A et al (2021) The different periods of COVID-19 in Germany: a descriptive analysis from January 2020 to February 2021. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 64:1093–1106
Schurink B, Roos E, Radonic T et al (2020) Viral presence and immunopathology in patients with lethal COVID-19: a prospective autopsy cohort study. Lancet Microbe 1:e290–e299
Sperhake JP (2020) Autopsies of COVID-19 deceased? Absolutely! Leg Med 47:101769
Swoboda J, Wittschieber D, Sanft J et al (2021) Bone marrow haemophagocytosis indicates severe infection with severe acute respiratory syndrome coronavirus 2. Histopathology 78:727–737
Treskova-Schwarzbach M, Haas L, Reda S et al (2021) Pre-existing health conditions and severe COVID-19 outcomes: an umbrella review approach and meta-analysis of global evidence. BMC Med 19:212
Trujillo-Santos J, Farge-Bancel D, Pedrajas JM et al (2022) Enoxaparin versus dalteparin or tinzaparin in patients with cancer and venous thromboembolism: the RIETECAT study. Res Pract Thromb Haemost 6:e12736
Varga Z, Flammer AJ, Steiger P et al (2020) Endothelial cell infection and endotheliitis in COVID-19. Lancet 395:1417–1418
https://covid19.who.int. Accessed 24 Mar 2023
Wichmann D, Sperhake JP, Lutgehetmann M et al (2020) Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med 173:268–277
Wu L, Baylan U, van der Leeden B et al (2022) Cardiac inflammation and microvascular procoagulant changes are decreased in second wave compared to first wave deceased COVID-19 patients. Int J Cardiol 349:157–165
Youd E, Moore L (2020) COVID-19 autopsy in people who died in community settings: the first series. J Clin Pathol 73:840–844
Zacharias M, Kashofer K, Wurm P et al (2022) Host and microbiome features of secondary infections in lethal covid-19. iScience 25:104926
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Autsch, H. Ihle, S. Kleemann, J. Sanft, M. Hahnemann, M. Hubig, M. Philipp, M. Bauer, S. Deinhardt-Emmer, N. Gaßler, G. Mall and D. Wittschieber declare that they have no competing interests.
All procedures on humans were performed with the approval of the local ethics committee (registration number 2020-1773), in accordance with national law and in accordance with the Declaration of Helsinki from 1975 (in the current, revised version).
Additional information
Availability of data and material
The manuscript has data included as electronic supplementary material.

Scan QR code & read article online
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Autsch, A., Ihle, H., Kleemann, S. et al. SARS-CoV-2-associated fatalities within the first year of the COVID-19 pandemic: an autopsy study. Rechtsmedizin 33, 262–268 (2023). https://doi.org/10.1007/s00194-023-00636-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00194-023-00636-x