Abstract
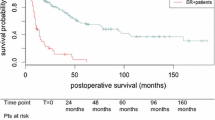
Esophageal resection for the treatment of esophageal cancer generally entails high rates of morbidity and mortality. Patients with a smoking history have increased post-operative complications following esophagectomy. This study was undertaken to determine how smoking or a history of smoking can affect perioperative outcomes and morbidity following robotic transhiatal esophagectomy. 75 patients were prospectively followed and divided; 44 patients actively smoking or with a history of significant smoking were classified as ‘smokers’, while the other 31 patients were classified as ‘non-smokers’. Significance was determined at a p-value of ≤ 0.05 and data are presented as median (mean ± SD). 'Smokers' averaged 70(70 ± 7.8) years, 89% male, with 82% undergoing neoadjuvant therapy. 'Nonsmokers' averaged 68(69 ± 7.8) years, 74% male, and 74% receiving neoadjuvant therapy. BMI and ASA class showed no significant difference between the cohorts. 'Smokers' had an operative time of 341(343 ± 91.0) minutes and a blood loss of 150(191 ± 140.0) mL; 'nonsmokers' had 291(298 ± 65.9) minutes and 100(140 ± 120.9) mL, respectively (p = 0.02 for operative time). Tumor size and AJCC staging were similar for both cohorts. No significant differences were noted in postoperative complications, Clavien–Dindo score ≥ III, in-hospital mortality, length of stay, or 30-day readmissions. Survival rates were comparable. Hospital costs for 'smokers' were $33,131(41,091 ± 23,465.17) and $34,896 (62,154 ± 65,839.53) for 'nonsmokers' (p = 0.05). Profit/loss was $-23,155 (− 15,137 ± 35,819.29) for smokers and $-23,720 (− 16,716 ± 50,864.64) for nonsmokers. Current or past ‘smokers’ had longer operative times and lower costs following robotic transhiatal esophagectomy, with no significant difference in postoperative complications or survival compared to ‘non-smokers’.


Similar content being viewed by others
Data availability
Due to the sensitive nature of the research data and the privacy constraints imposed by our study protocol, the data that support the findings of this study are not publicly available. All relevant data are protected to ensure participant confidentiality and comply with ethical standards.
References
Markar S, Gronnier C, Duhamel A et al (2015) The impact of severe anastomotic leak on long-term survival and cancer recurrence after surgical resection for esophageal malignancy. Ann Surg 262:972–980
Sakowitz S, Mabeza RM, Bakhtiyar SS et al (2023) Acute clinical and financial outcomes of esophagectomy at safety-net hospitals in the United States. PLoS ONE 18:e0285502
Weijs TJ, Ruurda JP, Nieuwenhuijzen GAP et al (2013) Strategies to reduce pulmonary complications after esophagectomy. World J Gastroenterol 19:6509–6514
Kamarajah SK, Madhavan A, Chmelo J et al (2021) Impact of Smoking Status on Perioperative Morbidity, Mortality, and Long-Term Survival Following Transthoracic Esophagectomy for Esophageal Cancer. Oncol 28:4905–4915
Zou G, Su Z, Li J et al (2019) Prognostic impact of cigarette smoking on the survival of patients with established esophageal squamous cell carcinoma receiving radiotherapy: A retrospective study from southern China. Exp Ther Med 17:3671–3681
Zingg U, Smithers BM, Gotley DC et al (2011) Factors associated with postoperative pulmonary morbidity after esophagectomy for cancer. Ann Surg Oncol 18:1460–1468
Nottingham JM, McKeown DG (2023) Transhiatal Esophagectomy. In: StatPearls. Treasure Island (FL): StatPearls Publishing
Hulscher JBF, Tijssen JGP, Obertop H et al (2001) Transthoracic versus transhiatal resection for carcinoma of the esophagus: a meta-analysis. Ann Thorac Surg 72:306–313
Clavien PA, Barkun J, De Oliveira ML et al (2009) The clavien-dindo classification of surgical complications: Five-year experience. Ann Surg 250:187–196
Wong J, Lam DP, Abrishami A et al (2012) Short-term preoperative smoking cessation and postoperative complications: A systematic review and meta-analysis. Can J Anesth 59:268–279
Wecowski J, Ross SB, Jadick MF et al (2019) The big deal: An institution’s experience with robotic transhiatal esophagectomy. Am Surg 85:1061–1065
Zheng Y, Cao X, Wen J et al (2015) Smoking affects treatment outcome in patients with resected esophageal squamous cell carcinoma who received chemotherapy. PLoS ONE 10:e0123246
Townsend AN, Denton A, Gohel N et al (2023) An Association Between Comorbidities and Postsurgical Complications in Adults Who Underwent Esophagectomy. Cureus 15:e36395
Goto H, Oshikiri T, Kato T et al (2022) The Influence of Preoperative Smoking Status on Postoperative Complications and Long-Term Outcome Following Thoracoscopic Esophagectomy in Prone Position for Esophageal Carcinoma. Ann Surg Oncol 30:2202–2211
Lee J, Taneja V, Vassallo R (2012) Cigarette smoking and inflammation: cellular and molecular mechanisms. J Dent Res 91(2):142–149
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by MC, and TP. The first draft of the manuscript was written by SR and KM. SR, IS and AR drafted the work and revised it critically for important intellectual content. All authors commented on previous versions of the manuscript, read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Sharona Ross is a consultant for Intuitive Surgical (Sunnyvale, CA) and Ethicon (Cincinnati, OH). Dr. Ross receives educational grants for her Women in Surgery Career Symposium from Intuitive Surgical and Medtronic (Minneapolis, MN). All other authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rayman, S., Ross, S., Sucandy, I. et al. The effects of smoking history on robotic transhiatal esophagectomy patient outcomes. J Robotic Surg 18, 76 (2024). https://doi.org/10.1007/s11701-024-01829-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11701-024-01829-6