Abstract
Purpose
The literature was reviewed to determine the risks or benefits of short-term (less than four weeks) smoking cessation on postoperative complications and to derive the minimum duration of preoperative abstinence from smoking required to reduce such complications in adult surgical patients.
Source
We searched MEDLINE, EMBASE, Cochrane, and other relevant databases for cohort studies and randomized controlled trials that reported postoperative complications (i.e., respiratory, cardiovascular, wound-healing) and mortality in patients who quit smoking within six months of surgery. Using a random effects model, meta-analyses were conducted to compare the relative risks of complications in ex-smokers with varying intervals of smoking cessation vs the risks in current smokers.
Principal findings
We included 25 studies. Compared with current smokers, the risk of respiratory complications was similar in smokers who quit less than two or two to four weeks before surgery (risk ratio [RR] 1.20; 95% confidence interval [CI] 0.96 to 1.50 vs RR 1.14; CI 0.90 to 1.45, respectively). Smokers who quit more than four and more than eight weeks before surgery had lower risks of respiratory complications than current smokers (RR 0.77; 95% CI 0.61 to 0.96 and RR 0.53; 95% CI 0.37 to 0.76, respectively). For wound-healing complications, the risk was less in smokers who quit more than three to four weeks before surgery than in current smokers (RR 0.69; 95% CI 0.56 to 0.84). Few studies reported cardiovascular complications and there were few deaths.
Conclusion
At least four weeks of abstinence from smoking reduces respiratory complications, and abstinence of at least three to four weeks reduces wound-healing complications. Short-term (less than four weeks) smoking cessation does not appear to increase or reduce the risk of postoperative respiratory complications.
Résumé
Objectif
La littérature disponible a été passée en revue pour déterminer les risques ou avantages d’un arrêt du tabagisme à court terme (moins de quatre semaines) sur les complications postopératoires et pour en déduire la durée minimum d’abstinence tabagique préopératoire qui permet de diminuer la survenue de ces complications chez des adultes subissant une chirurgie.
Source
Notre étude a porté sur les bases de données MEDLINE, EMBASE, Cochrane, et les autres bases de données pertinentes à la recherche d’études de cohortes ou d’études randomisées et contrôlées ayant décrit les complications postopératoires (c’est-à-dire respiratoires, cardiovasculaires, retard de cicatrisation) et la mortalité chez des patients ayant cessé de fumer dans les six mois ayant précédé l’intervention chirurgicale. Des méta-analyses ont été effectuées en utilisant un modèle à effets aléatoires pour comparer les risques relatifs de complications chez les anciens fumeurs, avec des délais variables d’arrêt du tabagisme, aux risques chez des fumeurs actifs.
Constatations principales
Nous avons inclus 25 études. Comparés aux fumeurs actifs, les risques de complications respiratoires ont été comparables chez les fumeurs ayant cessé de fumer moins de deux semaines, ou entre deux et quatre semaines avant une intervention chirurgicale (rapport de risque [RR]: 1,20; intervalle de confiance [IC] à 95 %: 0,96-1,50, contre, respectivement, RR: 1,14; IC à 95 %: 0,90-1,45). Les fumeurs ayant cessé de fumer plus de quatre semaines et plus de huit semaines avant l’intervention chirurgicale avaient des risques de complications respiratoires moins élevés que les fumeurs actifs (RR: 0,77; IC à 95 %: 0,61-0,96 et RR: 0,53; IC à 95 %: 0,37-0,76, respectivement). Concernant les complications liées à la cicatrisation, le risque a été plus faible chez les fumeurs ayant cessé plus de trois à quatre semaines avant l’intervention que chez les fumeurs actifs (RR: 0,69; IC à 95%: 0,56-0,84). Peu d’études ont décrit des complications cardiovasculaires et il n’y a eu que peu de décès.
Conclusion
Un minimum de quatre semaines d’abstinence du tabagisme diminue le risque de complications respiratoires et un minimum de trois à quatre semaines réduit le risque de complications liées à la cicatrisation. L’arrêt à court terme (moins de quatre semaines) du tabagisme ne semble pas augmenter ou réduire le risque de complications respiratoires postopératoires.
Similar content being viewed by others
Smoking is associated with increased postoperative morbidity and mortality.1-3 This is a major concern as up to 20% of surgical patients are smokers.4,5 A recent large observational study of non-cardiac surgical patients reported that smoking is associated with a 38% increase in the risk of perioperative death and a 30-109% increase in the risk of serious postoperative complications, depending on the type of complication.3 However, this study did not examine whether short-term abstinence from smoking before surgery reduces the risk of postoperative complications.
A relatively long period of abstinence from smoking before surgery reduces postoperative complications.6,7 Two systematic reviews showed that preoperative smoking cessation programs increased short-term (up to six months) abstinence.8,9 Consequently, both the American Society of Anesthesiologists10 and the Canadian Anesthesiologists’ Society11 recommend promoting smoking cessation before surgery. However, surgery is frequently scheduled within a few weeks of diagnosis of certain conditions, thus precluding longer periods of preoperative abstinence. As well, anesthesiologists typically see patients within one to four weeks of planned surgery. Anesthesiologists may be reluctant to advocate smoking cessation shortly before surgery because the benefits of a short period of abstinence (less than four weeks) are uncertain, and there could possibly be increased risks of postoperative respiratory12 or cardiovascular complications, or mortality.13 Interestingly, a paradoxical effect of lower mortality and improved outcome was observed in smokers compared with non-smokers after acute myocardial infarction, heart failure, and stroke.14-16 These data suggest that it may be inappropriate to stop smoking shortly before surgery.
A recent meta-analysis found that smoking cessation less than eight weeks before surgery did not increase or decrease the rate of overall or respiratory complications.17 However, the authors pooled studies with varying duration of smoking cessation (two to eight weeks before surgery) and did not examine wound-healing complications. Therefore, the effect of cessation of smoking shortly before surgery is still unclear.
It is important to determine the benefits or risks of short-term abstinence from smoking before surgery in order to guide anesthesiologists and other clinicians when providing preoperative advice to smokers. The objectives of this systematic review are to determine the benefits or risks of short-term (less than four weeks) abstinence from smoking compared with continued smoking on postoperative complications (respiratory, cardiovascular, wound-healing) and mortality and to determine the minimum duration of preoperative smoking cessation to reduce postoperative complications.
Methods
Search strategy
In collaboration with a research librarian, we searched Medline (January 1950 - April 2010 and May 2010 - January 2011), EMBASE (January 1980 - January 2011), Cochrane Database of Systematic Reviews (January 2005 - January 2011), and the Cochrane Controlled Trials Register (January 2011). Searches were conducted using two different components: 1) Smoking/Smoking cessation and related terms component 2) Preoperative/Surgery/Anesthesia and related terms component. Both text-word and index-word terms were used; the text word terms in our search strategies included smoke*, nicotine?, cigar*, preop*, preoperat*, perioperat*, preanesthe*, presurg*, surger*, surgical*, operat*, resect*, operati*, operation?, operative*, anesthe*, anaesthe*, perisurg*, preadmit*, and preadmission*. The following exploded index-word terms were used: ‘tobacco use cessation’, ‘smoking cessation’, ‘smoking’, ‘tobacco’, ‘tobacco use disorder’, ‘nicotine’, ‘preoperative care’, ‘preoperative period’, ‘perioperative care’, ‘perioperative nursing’, ‘surgical procedures, operative’, ‘general surgery’, ‘anesthesiology’ and ‘anesthesia’. Articles were limited to human studies and to the English language (Appendix). The bibliographies of retrieved articles and relevant reviews were searched manually for further studies.
Study selection
Two reviewers (J.W., D.L.) independently screened titles and abstracts to identify studies reporting postoperative complications (respiratory, cardiovascular, wound-healing) or death in relation to timing of preoperative smoking cessation within six months before surgery. Any disagreements were resolved by consensus or by consulting the senior author (F.C.). All randomized controlled trials (RCT) and cohort studies were included.
Studies were excluded if the period of smoking cessation was more than six months before surgery or not reported. We included RCTs that offered interventions if the complications were reported according to the actual smoking behaviour (i.e., continued to smoke or abstained) regardless of the intervention that the patient was randomized to receive. We contacted the corresponding authors if complications were not reported according to actual smoking status. Strategies were used to avoid duplicate publications.
Data extraction
Two reviewers (J.W., D.L.) independently extracted study characteristics and rated study quality. The following information was extracted from each study: continent, number of study participants, description of intervention, study design, surgical procedure, duration of preoperative smoking cessation, and postoperative complications (as reported in the primary studies) for ex-smokers, current smokers, and non-smokers. Respiratory complications included: bronchospasm needing treatment, atelectasis requiring bronchoscopy and/or assisted ventilation, pulmonary infection, pleural effusion, pneumothorax, empyema, pulmonary embolus, adult respiratory distress syndrome, respiratory failure or arrest, re-intubation and ventilation, tracheostomy, and high inspired oxygen required for 24 hr. Cardiovascular complications included: life-threatening arrhythmias, severe hemodynamic disturbances, myocardial infarction, congestive heart failure, and cerebral vascular accident. Wound-healing complications included: impaired wound healing requiring intervention (e.g., debridement or re-suturing), wound dehiscence, flap or fat necrosis, hernia, vessel thrombosis, wound hematoma, seroma, mediastinitis, wound infection with positive microbial culture or requiring antibiotic therapy, wound cellulitis and swelling. We also extracted information about study quality, including number of dropouts, comparability of groups, adjustment for confounders, blinding, follow-up period, biochemical validation of smoking cessation, and funding source. We categorized non-smokers as those who never smoked; ex-smokers were those who stopped smoking any time before surgery, and current smokers were those who continued to smoke up to the day of surgery.
Quality assessment
We did not assess the quality of the RCTs, as the objective of this review was not to determine the effectiveness of various interventions for reducing complications but rather to determine the effect of short-term smoking cessation on postoperative complications and the minimum duration of smoking cessation to reduce postoperative complications. We conformed to the Meta-analysis of observational studies in epidemiology (MOOSE) group guidelines.18 The quality of the studies was considered high if the design, conduct, and reporting of the studies were unlikely to be susceptible to bias. High-quality studies fulfilled the following criteria: validation of self-reported smoking status with biochemical methods, comparability of patients, adjustment for potential confounders for postoperative complications, adequate length of follow-up, blinding of the outcome assessor, and reporting of the source of funding.
Data synthesis and analysis
The primary outcome was the respiratory complications among ex-smokers with less than two weeks and two to four weeks of abstinence compared with current smokers. Secondary outcomes included postoperative complications (respiratory, cardiovascular, wound-healing) and mortality among ex-smokers and smokers, smokers and non-smokers, ex-smokers and non-smokers.
Meta-analysis of the relative risks of complications (respiratory, cardiovascular, wound-healing) and mortality was performed in ex-smokers and smokers and ex-smokers and non-smokers when at least two studies comparing similar intervals were available. We also directly compared the relative risks of complications in different periods of preoperative smoking cessation with the risks in smokers and non-smokers. For the meta-analyses, we planned to categorize ex-smokers into different preoperative smoking cessation periods, i.e., less than two weeks, two to four weeks, more than four weeks, or more than eight weeks based on the cessation period reported in the original studies. Due to the clinical differences between the studies (e.g., patient population, study design, etc.), a random-effects model was used in all meta-analyses. The Mantel-Haenszel test was used to calculate the risk ratio (RR) and the corresponding 95% confidence interval (CI) for each meta-analysis. The I2 statistic was used to measure inconsistency among the study results. 19 A value > 50% may be considered moderate heterogeneity. Review Manager (RevMan) version 5.1 (The Nordic Cochrane Centre, The Cochrane Collaboration, 2011, Copenhagen) was used for all meta-analyses. Sensitivity analyses were performed for type of surgery (e.g., cardiac vs non-cardiac) and quality of study.
Results
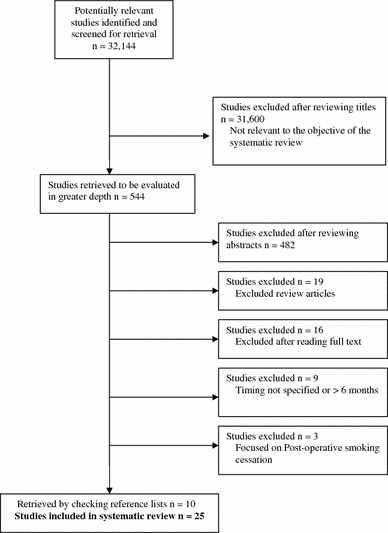
The search strategy yielded 32,144 citations. We identified 25 studies that fulfilled our inclusion criteria, for a total of 21,381 patients (Fig. 1). There were seven prospective cohort studies,12,20-25 16 retrospective cohort studies,26-41 and two RCTs (Table 1).42,43 Both RCTs offered nicotine replacement therapy.42,43 There were 14 studies from North America,12,21,23,26,30-35,37,39-41 six from Europe,22,27,28,38,42,43 four from Asia,20,25,29,36 and one from Australia.24
There were more male than female smokers, and smokers were younger than non-smokers or ex-smokers in many of the studies. The type of surgery, definition of complications, duration of smoking cessation, and the definition of “non-smokers”, “ex-smokers”, and “current smokers” reported in the individual studies varied between studies.
There were few studies that fulfilled most of the criteria for high quality (Table 1). Four studies used biochemical methods, including exhaled carbon monoxide and urinary cotinine concentrations, to validate the smoking status of the patients.12,24,42 Four studies had comparable groups among smokers, ex-smokers, and non-smokers.43 Six of the observational studies adjusted for potential confounders (Table 1). The follow-up periods were not specified in 13 studies (Table 1).12,20,22,27-30,33-38,40 The outcome assessor for postoperative complications was blinded to the smoking status of the patients in only five of the studies.12,29,36,42,43 All five studies reporting the source of funding received public funding,21,24,36,42,43 and the nicotine replacement products were provided by the manufacturers (Table 1).42,43
Respiratory complications
Fifteen studies involving 19,323 patients reported respiratory complications (Table 2, available as electronic supplemental material [ESM]).12,20,21,23-32,40,42 There were four different time points commonly reported by the studies for respiratory complications, i.e., less than two weeks, two to four weeks, more than four weeks, and more than eight weeks of smoking cessation before surgery. Fourteen studies involving 17,160 patients were included in the meta-analyses.12,20,21,23-26,28-32,40,42 Eight of these studies involving 3,331 patients were prospective.12,20,21,23-25,42,43 As there was only one study examining the effect of less than or more than 12 weeks cessation, we could not perform a meta-analysis of this time point.27
Summary of meta-analyses of respiratory complications
(The individual meta-analyses are available as ESM, Figs 6-17).
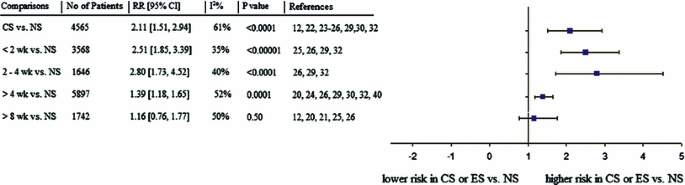
The relative risk (RR) of postoperative respiratory complications was higher in those who continued smoking at the time of surgery compared with non-smokers (RR 2.11; 95% CI 1.51 to 2.94; I2 = 61%; P < 0.0001). When the period of abstinence from smoking was more than eight weeks, the risk was similar in ex-smokers and in non-smokers (RR 1.16; 95% CI 0.76 to 1.77; I2 = 50%; P = 0.50), but a shorter period of abstinence failed to reduce the risk to values as low as those in non-smokers (Fig. 2). The type of surgery largely explained the heterogeneity, and grouping similar types of surgery together, i.e., cardiac vs non-cardiac surgery, reduced heterogeneity.
Summary of the meta-analyses of postoperative respiratory complications in current smokers or ex-smokers compared with non-smokers. The squares indicate the overall relative risk and the horizontal lines indicate the 95% confidence interval for each time interval. CS = current smoker; NS = non-smoker; ES = ex-smokers
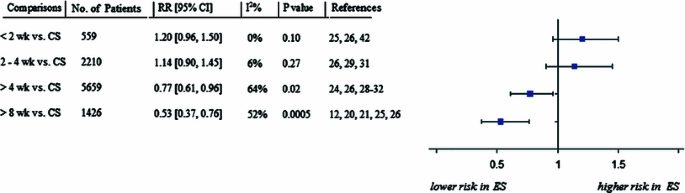
Compared with current smokers, the risk of respiratory complications was not higher in ex-smokers who abstained less than two weeks or two to four weeks before surgery (Fig. 3). On the other hand, the risks of respiratory complications in those who quit more than four weeks before surgery were significantly lower compared with current smokers (Fig. 3). The RR was 0.77 (95% CI 0.61 to 0.96; I2 = 64%; P = 0.02) with more than four weeks of smoking cessation, and the RR was further reduced to 0.53 (95% CI 0.37 to 0.76; I2 = 52%; P = 0.0005) in those who quit more than eight weeks before surgery. The type of surgery, i.e., cardiac vs non-cardiac surgery, explained part of the heterogeneity at more than eight weeks but not at more than four weeks. The number of high-quality studies with similar smoking cessation intervals was insufficient to perform sensitivity analyses.
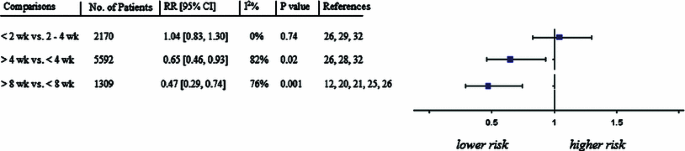
Direct comparisons of different intervals of smoking cessation and respiratory complications showed that there was no difference between patients who stopped smoking less than two weeks vs two to four weeks before surgery (Fig. 4). Notably, the risk of respiratory complications was lower in those who stopped smoking more than four weeks vs less than four weeks before surgery. Similarly, the RR was less in ex-smokers who quit more than eight weeks vs less than eight weeks before surgery (Fig. 4). The type of surgery, i.e., cardiac vs non-cardiac surgery, largely explained the heterogeneity at four weeks but not at eight weeks.
Cardiovascular complications
Cardiovascular complications were evaluated in only five studies involving 1,818 patients.20,31,40,42,43 One of the RCTs did not report cardiovascular complications according to actual abstinence or continued smoking, and the authors did not respond to our request for these data.43 There were no differences in risks for cardiovascular complications among current smokers, ex-smokers (one to eight weeks abstinence), and non-smokers (Table 3; available as ESM). However, a meta-analysis on this outcome was not performed as there were few cardiovascular complications reported in the studies, and the sample sizes were limited.
Wound-healing complications and studies for performing a meta-analysis
There were 15 studies involving 9,536 patients that reported wound-healing complications (Table 4, available as ESM).22,24,27,28,33-43
There was only one time point (i.e., less than or more than three to four weeks before surgery) with an adequate number of studies for meta-analysis. Thirteen studies involving 7,265 patients were included in the meta-analysis.22,24,28,33-42 There was twice the risk of wound-healing complications in those who continued smoking at the time of surgery vs non-smokers (RR 2.08; 95% CI 1.60 to 2.71; I2 = 8%; P < 0.00001) (Fig. 18, available as ESM).
The risk remained higher in ex-smokers who quit smoking within three to four weeks before surgery vs non-smokers (RR 1.64; 95% CI 1.40 to 1.92; I2 = 0%; P < 0.00001) (Fig. 19, available as ESM). However, risks of wound-healing complications in patients who abstained from smoking beyond three to four weeks before surgery were similar to those in patients who had never smoked (RR 1.44; 95% CI 0.97 to 2.15; I2 = 76%; P = 0.07) (Fig. 20, available as ESM). The type of surgery did not explain the heterogeneity.
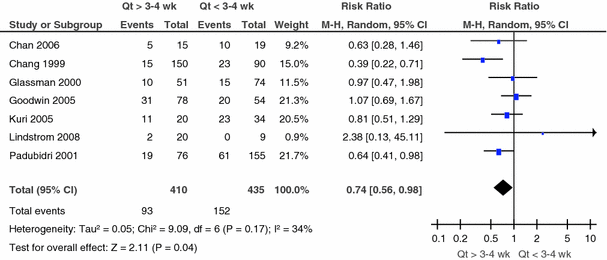
Ex-smokers who quit less than three to four weeks before surgery had similar risks for wound-healing complications as current smokers (RR = 1.22; 95% CI 0.56 to 2.67; I2 = 86%; P = 0.61) (Fig. 21, available as ESM). The type of surgery did not explain heterogeneity, but the number of studies was limited at this time interval. The risks of wound-healing complications in ex-smokers who stopped smoking more than three to four weeks before surgery were significantly lower than in current smokers (RR 0.69; 95% CI 0.56 to 0.84; I2 = 0%; P = 0.0003) (Fig. 22, available as ESM). In addition, direct comparisons showed the risk was significantly lower in ex-smokers who stopped smoking more than three to four weeks before surgery vs those who stopped less than three to four weeks before surgery (RR 0.74; 95% CI 0.56 to 0.98; I2 = 34%; P = 0.04) (Fig. 5). Therefore, more than three to four weeks of preoperative abstinence is necessary to reduce risks of wound-healing complications.
Ex-smokers who quit more than three to four weeks before surgery had lower relative risks of postoperative wound-healing complications than those who quit less than three to four weeks before surgery. The squares indicate the overall relative risk and the horizontal lines indicate the 95% confidence interval for each time interval. The diamond represents the pooled estimate. Qt = quit time; CI = confidence interval; M-H = Mantel Haenszel; wk = weeks
Mortality
Ten of the studies reported mortality rates.12,20,21,23,27,28,30,32,42,43 One large retrospective study in pulmonary resections for lung cancer reported higher mortality in current and ex-smokers compared with non-smokers (1.5% vs 0.3%, respectively; P < 0.05).32 The other nine studies did not report differences in mortality among smokers who quit at different intervals before surgery and current and non-smokers.12,20,21,23,27,28,30,42,43 However, there were few deaths reported in the included studies, and the individual studies were not large enough to detect differences in mortality.
Discussion
This review supports the notion that there is a time-related decrease in the risk of respiratory complications, i.e. the relative risk decreases as the duration of preoperative smoking cessation increases. Most importantly, cessation of smoking more than four weeks before surgery reduced the risk of respiratory complications by 23%. Those who stopped smoking more than eight weeks before surgery had greater benefits, and the risk of respiratory complications was reduced by 47%. Indeed, the risk of respiratory complications in those who stopped smoking more than eight weeks before surgery was comparable with non-smokers. In all probability, patients should stop smoking at least four weeks, and preferably eight weeks, before surgery to reduce postoperative respiratory complications. However, there was no evidence that short-term abstinence from smoking (less than four weeks) before surgery increases or reduces postoperative respiratory complications compared with continued smoking, but only a few studies examined this interval. There was no difference in mortality between smokers and ex-smokers, but there were few deaths reported in the included studies.
Our meta-analysis shows that smokers who abstained more than three to four weeks before surgery had fewer wound-healing complications than current smokers. As well, smokers who quit more than three to four weeks before surgery had fewer wound-healing complications than those who quit less than three to four weeks before surgery. Our results are consistent with a well-conducted study in wound healing following excisional punch biopsy that reported a reduction in the incidence of wound infections with four weeks of abstinence from smoking.44 However, this study was not included in our review as it did not involve a surgical procedure.
We did not find evidence to support that short-term abstinence from tobacco may lead to acute withdrawal, increased sympathetic activity, and increased cardiovascular complications. However, a limited number of studies reported cardiovascular complications. Therefore, we could not determine the risk or benefits of smoking cessation for prevention of cardiovascular complications.
The findings of our systematic review and meta-analysis are consistent with previous reviews and extend their findings.6,7,17 Our review included more studies than a previous review which was limited to a comparison of smokers vs ex-smokers who quit less than eight weeks before surgery.17 We also examined wound-healing complications, and we did not pool the results of studies with different periods of cessation. In contrast, by comparing different intervals of short-term cessation with continued smoking and including studies that directly compared different intervals of cessation (e.g., less than two weeks vs two to four weeks) on postoperative complications, we were able to determine the minimum duration of preoperative smoking cessation necessary to reduce postoperative respiratory and wound-healing complications. Our findings also confirm that smokers have higher risks for postoperative respiratory and wound-healing complications than non-smokers.3
The results of our review should be interpreted with caution due to several limitations of the included studies. Few studies had high methodological quality, and most of the included studies were retrospective observational studies. However, it would be difficult to perform a prospective trial with randomization of patients to different periods of abstinence before surgery. Our conclusions are based on the best evidence that is currently available. The majority of the studies relied on self-reporting of smoking status, which may have led to the status being inaccurately reported. Many of the studies did not adjust for confounding factors between groups. The study designs and definition of postoperative complications varied among the studies. As well, the smoking cessation intervals in some studies were not clearly defined, and intervals overlapped with more than one time interval. To overcome this problem, we grouped together similar intervals of the reported smoking cessation periods and compared them collectively. In addition, many of the studies did not report clinically significant outcome measures, including recovery room and hospital length of stay. Another limitation of this review is our exclusion of articles not published in English.
The heterogeneity was moderate or high for a few of the meta-analyses. The type of surgery could explain some of the heterogeneity; however, smoking increases complications across all non-cardiac surgical procedures3 and including different types of surgery increases generalizability of our findings. The number of high-quality studies with similar smoking cessation intervals was insufficient to perform the relevant sensitivity analysis. Other factors that explain the heterogeneity may include the wide range of time intervals vs clearly defined intervals reported in individual studies. Sensitivity analyses of other potential factors explaining heterogeneity, such as disease severity, patient morbidity, etc., were not possible due to limited data reported in the individual studies. However, heterogeneity exists in the amount of overall effect, not in the direction of the effect, i.e., although the RRs were different, all were on the same side of the Forest plot. Nonetheless, we used the random effects method, which is more suitable when heterogeneity exists.45
In conclusion, at least four weeks of preoperative smoking cessation is necessary to reduce respiratory complications, and at least three to four weeks of abstinence is needed to reduce wound-healing complications. Based on the available studies examining short-term (less than four weeks) abstinence from smoking, short-term abstinence does not increase or reduce postoperative respiratory complications. However, given the known long-term benefits of smoking cessation, including an improvement in long-term health, and the “teachable moment” a pre-admission visit provides, our findings should not deter anesthesiologists and other perioperative clinicians from counselling surgical patients to stop smoking regardless of the time of visit. Future studies should examine the ideal time frame for smoking cessation prior to surgery, consider adjusting for confounders, and target more clinically significant outcomes, such as hospital length of stay.
References
Warner DO. Perioperative abstinence from cigarettes: physiologic and clinical consequences. Anesthesiology 2006; 104: 356-67.
Warner DO. Tobacco dependence in surgical patients. Curr Opin Anaesthesiol 2007; 20: 279-83.
Turan A, Mascha EJ, Roberman D, et al. Smoking and perioperative outcomes. Anesthesiology 2011; 114: 837-46.
Agostini P, Cieslik H, Rathinam S, et al. Postoperative pulmonary complications following thoracic surgery: are there any modifiable risk factors? Thorax 2010; 65: 815-8.
Centers for Disease Control and Prevention (CDC). Cigarette smoking among adults and trends in smoking cessation - United States, 2008. MMWR Morb Mortal Wkly Rep 2009; 58: 1227-32.
Theadom A, Cropley M. Effects of preoperative smoking cessation on the incidence and risk of intraoperative and postoperative complications in adult smokers: a systematic review. Tob Control 2006; 15: 352-8.
Mills E, Eyawo O, Lockhart I, Kelly S, Wu P, Ebbert JO. Smoking cessation reduces postoperative complications: a systematic review and meta-analysis. Am J Med 2011; 124: 144-54e8.
Thomsen T, Tonnsen H, Moller AM. Effect of preoperative smoking cessation interventions on postoperative complications and smoking cessation. Br J Surg 2009; 96: 451-61.
Zaki A, Abrishami A, Wong J, Chung F. Interventions in the preoperative clinic for long term smoking cessation: a quantitative systematic review. Can J Anesth 2008; 55: 11-21.
American Society of Anesthesiologists. Statement on Smoking Cessation (2008). Available from URL: http://www.asahq.org/For-Healthcare-Professionals/Standards-Guidelines-and-Statements.aspx (accessed January 2011).
Canadian Anesthesiologists Society. Stop Smoking for Safer Surgery. Available from URL: http://www.cas.ca/English/Stop-Smoking (accessed January 2011).
Warner MA, Offord KP, Warner ME, Lennon RL, Conover A, Jansson-Schumacher U. Role of preoperative smoking cessation and other factors in postoperative pulmonary complications: a blinded prospective study of coronary artery bypass patients. Mayo Clin Proc 1989; 64: 609-16.
Ruiz-Bailen M, de Hoyos EA, Reina-Toral A, et al. Paradoxical effect of smoking in the Spanish population with acute myocardial infarction and unstable angina. Chest 2004; 125: 831-40.
Fonarow GC, Abraham WT, Albert NM, et al. A smoker’s paradox in patients hospitalized for heart failure: findings from OPTIMIZE-HF. Eur Heart J 2008; 29: 1983-91.
Ovbiagele B, Saver JL. The smoking-thrombolysis paradox and acute ischemic stroke. Neurology 2005; 65: 293-5.
Ferreira R. The paradox of tobacco: smokers have a better post-infarct prognosis (Portuguese). Rev Port Cardiol 1998; 17: 855-6.
Myers K, Hajek P, Hinds C, McRobbie H. Stopping smoking shortly before surgery and postoperative complications: a systematic review and meta-analysis. Arch Int Med 2011; 171: 983-9.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting: Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 2000; 283: 2008-12.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327: 557-60.
Azarasa M, Azarfarin R, Changizi A, Alizadehasl A. Substance use among Iranian cardiac surgery patients and its effects on short-term outcome. Anesth Analg 2009; 109: 1553-9.
Barrera R, Shi W, Amar D, et al. Smoking and timing of cessation: impact on pulmonary complications after thoracotomy. Chest 2005; 127: 1977-83.
Araco A, Gravante G, Sorge R, Araco F, Delohu D, Cervelli V. Wound infections in aesthetic abdominoplasties: the role of smoking. Plast Reconstr Surg 2008; 121: 305e-10e.
Bluman LG, Mosca L, Newman N, Simon DG. Preoperative smoking habits and postoperative pulmonary complications. Chest 1998; 113: 883-9.
Myles PS, Iacono GA, Hunt JO, et al. Risks of respiratory complications and wound infection in patients undergoing ambulatory surgery: smokers versus nonsmokers. Anesthesiology 2002; 97: 842-7.
Yamashita S, Yamaguchi H, Sakaguchi M, et al. Effect of smoking on intraoperative sputum and postoperative pulmonary complication in minor surgical patients. Respir Med 2004; 98: 760-6.
Warner MA, Divertie MB, Tinker JH. Preoperative cessation of smoking and pulmonary complications in coronary artery bypass patients. Anesthesiology 1984; 60: 380-3.
Ngaage DL, Martins E, Orkell E. The impact of the duration of mechanical ventilation on the respiratory outcome in smokers undergoing cardiac surgery. Cardiovasc Surg 2002; 10: 345-50.
Al-Sarraf N, Thalib L, Hughes A, Tolan M, Young V, McGovern E. Effect of smoking on short-term outcome of patients undergoing coronary artery bypass surgery. Ann Thorac Surg 2008; 86: 517-23.
Nakagawa M, Tanaka H, Tsukuma H, Kishi Y. Relationship between the duration of the preoperative smoke-free period and the incidence of postoperative pulmonary complications after pulmonary surgery. Chest 2001; 120: 705-10.
Vaporciyan AA, Merriman KW, Ece F, et al. Incidence of major pulmonary morbidity after pneumonectomy: association with timing of smoking cessation. Ann Thorac Surg 2001; 73: 420-6.
Groth SS, Whitson BA, Kuskowski MA, Holmstrom AM, Rubins JB, Kelly RF. Impact of preoperative smoking status on postoperative complication rates and pulmonary function test results 1-year following pulmonary resection for non-small cell lung cancer. Lung Cancer 2009; 64: 352-7.
Mason DP, Subramanian S, Nowicki ER, et al. Impact of smoking cessation before resection of lung cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database Study. Ann Thor Surg 2009; 88: 362-71.
Chang DW, Reece GP, Wang B, et al. Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg 2000; 105: 2374-80.
Padubidri AN, Yetman R, Browne E, et al. Complications of postmastectomy breast reconstructions in smokers, ex-smokers, and nonsmokers. Plast Reconstr Surg 2001; 107: 342-9.
Goodwin SJ, McCarthy CM, Pusic AL, et al. Complications in smokers after postmastectomy tissue expander/implant breast reconstruction. Ann Plast Surg 2005; 55: 16-20.
Kuri M, Nakagawa M, Tanaka H, Hasuo S, Kishi Y. Determination of the duration of preoperative smoking cessation to improve wound healing after head and neck surgery. Anesthesiology 2005; 102: 892-6.
Spear SL, Ducic I, Cuoco F, Hannan C. The effect of smoking on flap and donor-site complications in pedicled TRAM breast reconstruction. Plast Reconstr Surg 2005; 116: 1873-80.
Chan LKW, Withey S, Butler PE. Smoking and wound healing problems in reduction mammaplasty: is the introduction of urine nicotine testing justified? Ann Plast Surg 2006; 56: 111-5.
Glassman SD, Anagnost SC, Parker A, Burke D, Johnson JR, Dimar JR. The effect of cigarette smoking and smoking cessation on spinal fusion. Spine (Phila Pa 1976) 2000; 25: 2608-15.
Moore S, Mills BB, Moore RD, Miklos JR, Mattox TF. Perisurgical smoking cessation and reduction of postoperative complications. Am J Obstet Gynecol 2005; 192: 1718-21.
Taber DJ, Ashcraft E, Cattanach LA, et al. No difference between smokers, former smokers, or nonsmokers in the operative outcomes of laparoscopic donor nephrectomies. Surg Laparosc Endosc Percutan Tech 2009; 19: 153-6.
Lindstrom D, Azodi OS, Wladis A, et al. Effects of a perioperative smoking cessation intervention on postoperative complications: a randomized trial. Ann Surg 2008; 248: 739-45.
Moller AM, Villebro N, Pedersen T, Tonnesen H. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet 2002; 359: 114-7.
Sorensen LT, Karlsmark T. Gottrup F Abstinence from smoking reduces incisional wound infection: a randomized controlled trial. Ann Surg 2003; 238: 1-5.
Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2009. Available from URL: http://www.cochrane-handbook.org (accessed January 2011).
Acknowledgements
The authors sincerely thank Marina Englesakis BA (Hons) MLIS, Information Specialist, Surgical Divisions, Neuroscience & Medical Education, Health Sciences Library, University Health Network, Toronto, ON, Canada for her assistance with the literature search.
Funding
This work was funded by the Department of Anesthesia, Toronto Western Hospital, University Health Network, and University of Toronto. No external funding. Dr. Wong is a recipient of a University of Toronto Merit Research Award.
Declaration of interests
Dr. Chung has received a research grant from Pfizer Inc. The other authors have nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Jean Wong was involved in data abstraction, interpretation of data, drafting and revising, and final approval of the article. David Paul Lam was involved in data abstraction and drafting of the article. Amir Abrishami was involved in drafting and revising the article, data analysis, and interpretation of the data. Matthew Chan revised and approved the final version of the article. Frances Chung was involved in the conception and design, revising, and final approval of the article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Wong, J., Lam, D.P., Abrishami, A. et al. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anesth/J Can Anesth 59, 268–279 (2012). https://doi.org/10.1007/s12630-011-9652-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-011-9652-x