Abstract
Purpose
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental condition characterized by inattention, hyperactivity, and impulsivity. A positive association between ADHD and obesity has been observed, especially in adult samples. In this study, prevalence and correlates of self-reported symptoms indicative of a positive screening for ADHD were examined in patients seeking bariatric treatment.
Material and Methods
The study sample was composed of 260 adult patients with obesity referred for bariatric surgery to the Obesity Center of the Endocrinology Unit in Pisa University Hospital between January 2006 and November 2016 (BMI ≥ 30 kg/m2; mean ± standard deviation = 46.27 ± 7.45 kg/m2). ADHD symptoms were identified using ADHD Symptom Check‐List‐90‐R Screening Scale. Night-eating, binge-eating/purging behaviors, and temperamental and character traits were assessed in a subsample of 95 patients.
Results
Thirty participants had a positive screening for ADHD (11.5%, 95% CI = 7.9–16.1%). Patients with a positive screening showed significantly higher rates of anxiety disorders (40% vs. 16.5%, χ2 = 7.97, p = 0.005) panic disorder (40% vs. 14.3%, χ2 = 10.48, p = 0.001), and a higher severity of psychopathological symptoms and sleep disturbances than those without. In subsample analyses, ADHD symptoms severity was associated with more bulimic behaviors (r = 0.31–0.46), greater harm avoidance (r = 0.45–0.66), less self-directedness (r = − 0.44–0.63), and cooperativeness (r = − 0.26–0.42).
Conclusion
ADHD symptoms may be common in patients with obesity seeking bariatric treatment and are positively associated with disordered eating, internalizing features, and maladaptive character traits.
Level of Evidence: V, cross sectional descriptive study.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental condition characterized by inappropriate levels of inattention, hyperactivity, and impulsivity [1,2,3,4,5,6]. High rates of comorbidity can be found between ADHD and a variety of psychiatric disorders, especially mood, anxiety, substance use, conduct, and personality disorders [7,8,9,10,11]. Youths with ADHD present a significantly increased risk of developing later substance abuse or dependence [12, 13], major depression [14, 15], and bipolar disorder [16]. ADHD is also associated with specific medical conditions, with a growing interest for the connection between ADHD and obesity. Both are chronic conditions that represent a relevant public and clinical health concern globally [17].
The prevalence of ADHD in clinical samples of patients in care for obesity is higher than in the general population [18], with up to over one-fourth of patients with obesity being diagnosed with predominantly inattentive ADHD [19]. This association is more pronounced in adolescents and adults than in children [20], and it is crucial for gaining a better understanding of the development of severe obesity [21].
Many pathogenetic mechanisms and dysfunctional pathways have been proposed to underlie the association between obesity and ADHD [18, 22]. First, it has been argued that ADHD and obesity share common genetics and neurobiological mechanisms that involve the dopaminergic system and brain reward pathways. Functional magnetic resonance imaging studies have identified a significant neural overlap in circuits associated with reward, response inhibition, and emotional processing and regulation in individuals with ADHD, obesity, and abnormal eating behavior [23]. Recent genetic and prenatal studies have further supported the bidirectional association between these conditions, encompassing both genetic and early environmental origins [22, 24].
From a clinical standpoint, obesity can also be considered, in comorbid cases, secondary to deficits in inhibitory control and executive functions associated with ADHD. Executive dysfunctions have been observed in patients with obesity [25] and may lead to disordered eating behaviors and feeding anomalies, such as binge-eating or bulimic behaviors, skipping meals, emotional hunger, eating at inappropriate times, and night-eating [22, 26]. Anomalies of the dopamine system may also lead to decreased physical activity and to a more sedentary lifestyle, combined with the consumption of highly palatable or caloric food, that activate the dopamine-reward pathways and could be used as self‐medication [27]. In addition, sleep problems encountered by individuals with ADHD, including disruptions in circadian rhythm and shortened sleep duration resulting from delayed onset of melatonin, have already been associated with the development of obesity [28, 29].
ADHD could potentially contribute to treatment challenges in patients with obesity participating in weight loss programs [30]. Although findings on the effect of ADHD on BMI change in patients undergoing bariatric surgery were mixed, ADHD symptoms have been associated with lower adherence to scheduled follow-up visits after the intervention [31], and there is some evidence that ADHD treatment might potentially improve the outcomes of weight-loss strategies in comorbid individuals [32]. From a different perspective, impulsivity, a core symptom domain of ADHD, has been proposed as a transdiagnostic psychological construct contributing to eating behavior and obesity, as well as to suboptimal outcomes of bariatric surgery [3]. Impulsivity refers both to the inability to inhibit automatic behavior in response to salient stimuli (i.e., response inhibition) and to the tendency to discount future consequences in favor of immediate rewards (i.e., delay discounting) [3]. Deficits of response inhibition and delay discounting, which are central to neuropsychological theories of ADHD [33, 34], have been observed in patients with obesity [35,36,37] and predict weight loss through obesity intervention [38,39,40]. Given the evidence of positive effects of ADHD treatment on response inhibition and delay discounting [41,42,43], diagnosing and treating ADHD in patients with obesity might help improve eating behavior and bariatric surgery outcomes.
Despite the potential significance of the comorbidity between these conditions, only a limited number of studies have explored the prevalence of ADHD or ADHD symptoms among patients with obesity seeking bariatric surgery [44,45,46,47,48,49,50,51]. Importantly, one of the most commonly used instruments to assess psychopathology in candidates for bariatric surgery, the Structured Clinical Interview for DSM-IV Axis I Disorders – Clinical Version (SCID-I) [52], does not include any section on adult ADHD [52]. Accordingly, ADHD has not been considered in several studies on the prevalence of psychiatric disorders in bariatric samples [53,54,55,56,57,58].
Even fewer studies focused on the psychopathological correlates of ADHD symptoms in these patients [45, 48]. Particularly, Gruss et al. investigated differences in demographic variables, history of psychotherapeutic contact, depressive symptoms and disorders, screening for binge-eating disorder, and daytime sleepiness between patients screening positive or negative for adult ADHD [48], while Alfonsson et al. examined the correlations among ADHD, anxious, depressive symptoms, and food cravings [45]. None of these studies focused on the associations of ADHD symptoms with other formally diagnosed affective disorders, such as bipolar disorder, anxiety disorders, and eating disorders. Additionally, they did not explore connections with other psychopathological dimensions, including bulimic and night-eating behaviors, as well as temperamental traits.
For a better identification of patients potentially impacted by ADHD within patients with obesity, an exploration of ADHD-related dimensions becomes crucial. In this post hoc analysis of data from a previously described sample of patients with obesity referred for bariatric surgical treatment [59], we examined the prevalence and the psychiatric comorbidity with mood, anxiety, and eating disorders of self-reported symptoms indicative of a positive screening for ADHD [3]. Differences in eating behavior and temperamental traits between participants with obesity with and without a positive screening for ADHD were also assessed.
Based on previous studies, significant positive associations between ADHD symptoms and bipolar or related disorders, sleep disturbances, and bulimic behaviors are expected. Importantly, this was the first study to investigate on temperament and ADHD symptoms in patients with obesity. Based on the available data in adult samples without obesity [60, 61], higher novelty seeking and harm avoidance, and lower self-directedness are expected to be associated with ADHD symptoms.
Patients and Methods
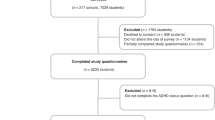
Recruitment and Assessment
The study sample was composed of 260 patients with obesity (BMI ≥ 30 kg/m2) referred for evaluation for bariatric surgery to the Obesity Center of the Endocrinology Unit in Pisa University Hospital between January 2006 and November 2016.
All patients were adult (≥ 18 years) and provided written informed consent to data collection for research purposes. Partial overlapping samples and procedures were previously described in studies from our group [5, 59]. Particularly, clinical charts of patients were retrieved and examined. For any given patient, two independent researchers retrieved the data and filled a pre-defined data abstraction form. Any disagreement was resolved by consensus after discussion.
All the medical records available were searched for sociodemographic information, anthropometric variables, i.e., weight and BMI, and lifetime diagnoses of mood, anxiety, and eating disorders. During the presurgical evaluation, all patients underwent standard interviews conducted by experienced licensed psychiatrists. In a single session, both current and lifetime psychiatric diagnoses were assessed. The SCID-I Clinical Version [52] was utilized to systematically assess symptoms of major depressive disorder, bipolar spectrum disorders (including BD type 1 and 2, and other specified bipolar disorder), anxiety disorders, and eating disorders (specifically anorexia and bulimia nervosa). Since the SCID-I was routinely used as part of clinical presurgical evaluations, no specific training was provided for the purposes of this study. The psychiatrists who conducted the interviews had received training during their education and had extensive experience in administering the SCID-I. Due to the nature of the interviews, a thorough assessment of the history of anorexia, bulimia, and binge-eating disorder was further conducted in accordance with DSM-IV-TR criteria [62]. Lifetime diagnoses of mood, anxiety, and eating disorders finally reported by clinicians according to DSM-IV-TR criteria after comprehensive evaluation of all the available information (e.g., information from other informants, review of past records, family history, treatment history) were recorded for this study.
The Symptom Checklist-90-Revised (SCL-90-R) was routinely used to investigate the severity of current general psychopathological symptoms and distress [63]. The SCL-90-R is a multidimensional self-rated measure consisting of 90 items rated on a five-point scale from 0 (“Not at All”) to 4 (“Extremely”) specifying how much each symptom has bothered during the past 7 days. Items are assembled into nine symptom dimensions, namely somatization, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. Three additional items investigate sleep disturbances. In bariatric patients, good internal consistency of all subscales (Cronbach’s α = 0.77–0.90) and convergent validity with the data gathered in the clinical interviews have been demonstrated [64]. A recent study also found good discriminant validity of the Italian version of the scale for binge-eating disorder and major depression in bariatric surgery candidates (area under the curve ≥ 0.70) [65]. Only patients having completed the SCL-90-R during pre-surgical consultations were included in this study.
ADHD symptoms were identified using the ADHD‐SCL‐90‐R screening scale [66], a recently developed screening instrument composed of 16 items selected from SCL-90-R, based on content match with items from the Conners’ Adult ADHD rating scale [67], an established questionnaire measuring adult ADHD symptoms. The items, originally belonging to the obsessive–compulsive, interpersonal sensitivity, depression, anxiety, and hostility dimensions of the SCL-90-R, are grouped in four subscales, which respectively capture Problems with Self‐Concept, Impulsivity/Emotional Lability, Inattention/Memory Problems, and Hyperactivity/Restlessness. As for the SCL-90-R, items are rated on a five-point Likert scale from 0 to 4. High significant correlations (r = 0.57–0.59) with ADHD‐specific scales have been evidenced. Compared to the other established ADHD‐specific tools, the ADHD‐SCL‐90‐R screening scale showed comparably good psychometric properties, except for a lower specificity. Overall, good to excellent internal consistency (Cronbach’s α = 0.79–0.90) and an acceptable discriminatory power (area under the curve = 0.74) was found in a sample of 412 individuals examined by an ADHD Special Consultations Unit [66]. The cut‐off value of 19 (i.e., total score ≥ 19) was chosen to detect patients with a positive screening for ADHD in our sample. This threshold was previously suggested by Abbass and colleagues, who reported a sensitivity of 78% and a specificity of 56% when utilizing that specific cut-off [66].
Disordered eating behaviors and temperamental traits were further investigated in a subsample of 95 patients (36.5% of the whole sample) who completed the Night Eating Questionnaire (NEQ) [68, 69], the Bulimic Investigatory Test, Edinburgh (BITE) [70, 71], and the Temperament and Character Inventory (TCI) [72, 73].
The NEQ, a commonly used screening instrument for night-eating disorder, consists of 14 self-rated items subdivided into four facets: morning anorexia, evening hyperphagia, mood/sleep, and nocturnal ingestions [68, 69]. Adequate internal consistency (Cronbach’s α = 0.70), convergent validity with measures of night eating, disordered eating, sleep, mood, and stress, and appropriate discriminant validity for night-eating syndrome (positive predictive value = 72.7%) were found in bariatric surgery candidates [68]. Similar internal consistency (Cronbach’s α = 0.48–0.71), positive correlations with measures of disordered eating, sleep, and mood, and adequate test–retest reliability (intraclass correlation coefficient = 0.68) were observed for the Italian version of the questionnaire [69].
The BITE is a self-report measure composed of two subscales: the symptom scale (30 items in yes/no format), which assess disordered eating and related psychological symptoms, and the severity scale (three items on a Likert scale), which evaluates the frequency of fasting, purging, and binge-eating behaviors [70, 71]. Good reliability (Cronbach’s α = 0.62–0.96; test–retest r = 0.68–0.86), excellent discriminant validity, convergence with other measures of disordered eating, and sensitivity to change were demonstrated in samples including patients with binge-eating behaviors and healthy controls [71]. The Italian version of the test has proved high internal consistency (Cronbach’s α = 0.82–0.91) and good discriminant validity for binge-eating disorder in women with obesity [70].
Finally, the TCI was used to evaluate temperamental traits based on Cloninger’s psychobiological theory of temperaments [72, 73]. It consists of 240 items, answered yes or no, exploring four temperamental dimensions (i.e., novelty seeking, harm avoidance, reward dependence, and persistence) and three character facets (i.e., self-directedness, cooperativeness, and self-transcendence). Adequate internal consistency and test–retest reliability have been repeatedly reported for TCI scales both in clinical [73, 74] and nonclinical samples [72, 75, 76].
Statistical Analyses
All the statistical analyses were performed using R Statistical Software (Foundation for Statistical Computing, Vienna, Austria) between January and June 2022. Shapiro–Wilk test was used to exclude normality. First, patients with and without a positive screening for ADHD were compared using Pearson’s chi-squared tests (or Fisher’s exact test, when needed) for gender and psychiatric comorbidity, and Wilcoxon rank-sum test for age, BMI and SCL-90-R subscales that did not included items overlapping with ADHD‐SCL‐90‐R screening scale (i.e., somatization, phobic anxiety, paranoid ideation, psychoticism, sleep) (N = 260).
Eating pattern and temperamental differences between patients with and without a positive screening were the evaluated in the subsample (N = 95) using Wilcoxon rank-sum test (or Student’s t test when comparing TCI-NS scores). Finally, the associations between ADHD symptoms severity as measured by ADHD‐SCL‐90‐R screening scale and its subscales and scales assessing eating behaviors and temperamental traits were tested using Spearman’s rank correlation coefficient (N = 95). This latter approach allowed to examine whether differential correlates of separate ADHD dimensions could be highlighted.
Non-parametric tests were used for continuous variables after exclusion of normality using Shapiro–Wilk test. A statistical significance level of p < 0.05 was set for all tests, after false discovery rate (FDR) correction for multiple comparisons.
Results
The sample was composed of 260 patients with obesity referred for bariatric surgery. Most patients were female (N = 187, 71.9%). Age ranged between 18 and 66 years, with a mean of 44.31 ± 10.71 years. Weight ranged between a minimum of 81.8 kg to a maximum of 221 kg, with a mean of 127.88 ± 24.53 kg. BMI ranged between 31.95 and 76.95 kg/m2, with a mean of 46.27 ± 7.45 kg/m2. Most patients were diagnosed with class II obesity (35 kg/m2 ≤ BMI < 40 kg/m2), with 208 out of 260 patients affected (80%). The other patients were diagnosed with class III obesity (BMI ≥ 40 kg/m2; N = 47, 18.1%), except for five (1.9%) who were affected by class I obesity (BMI < 35 kg/m2) and were referred for presurgical evaluation due to severe obesity complications or comorbidities. Similar characteristics were evidenced in patients’ subsample (Table 1).
Notably, according to some guidelines [77], bariatric surgery could be considered for patients with BMI ≥ 35–40 kg/m2 with associated comorbidities that are expected to improve with weight loss, as well as for patients with BMI ≥ 30–35 kg/m2 and type 2 diabetes and/or hypertension with poor control despite optimal medical therapy. Not all patients included were considered eligible for bariatric surgery after the evaluation.
Thirty participants were identified as having a positive screening for ADHD according to ADHD‐SCL‐90‐R screening scale (11.5%, 95% CI = 7.9–16.1%). A similar prevalence was observed in patients’ subsample (13 of 95, 13.7%, 95% CI = 7.5–22.3%).
Differences in demographic and anthropometric characteristics, lifetime psychiatric comorbidity, and SCL-90-R subscales not including items overlapping with ADHD‐SCL‐90‐R screening scale were assessed in the whole sample (N = 260) (Table 2). No significant differences emerged for age, gender, and BMI. Patients with a positive screening for ADHD were significantly more frequently diagnosed with anxiety disorders in comparison with patients without. Panic disorder was specifically significantly associated with a positive screening for ADHD. Mood disorders, particularly bipolar disorder type 2 and bipolar or related disorders in general, were more frequently diagnosed in patients with a positive screening for ADHD than in those without; however, these differences did not survive FDR correction for multiple comparisons. No significant differences were observed for eating disorders and family history of mood and anxiety disorders. Significant differences in all the non-overlapping SCL-90-R subscales were observed: patients with a positive screening for ADHD showed significantly higher scores on somatization, phobic anxiety, paranoid ideation, psychoticism, and sleep disturbances compared to unaffected participants.
Differences in NEQ, BITE and TCI subscales were evaluated within the study subsample (N = 95) (Table 3). Patients with a positive screening for ADHD scored significantly higher on NEQ mood/sleep subscale, BITE symptom scale, and TCI harm avoidance scale compared to patients without. Significantly lower scores on the TCI self-directedness and cooperativeness scales were found in patients with a positive screening for ADHD. Higher NEQ total scores were also observed in patients with a positive screening; however, the difference was not significant after FDR correction.
The associations between NEQ, BITE, and TCI subscales and ADHD‐SCL‐90‐R screening scale total and subscales scores were also tested according to a dimensional approach, to evaluate whether different ADHD facets could be specifically associated with disordered eating behavior and/or with distinct temperament and character dimensions. A similar pattern of correlations was observed for ADHD‐SCL‐90‐R screening scale total score and for each of its subscales, corresponding to previously observed differences between patients with and without a positive screening for ADHD (Table 4).
Discussion
A positive screening for ADHD was found in 11.5% of our sample (N = 260) and was significantly associated with anxiety disorders, especially panic disorder. Patients who had a positive screening showed a significantly higher severity of psychopathological symptoms and sleep disturbances compared to those unaffected. In contrast with our hypothesis, mood disorders, particularly bipolar disorder type 2 and bipolar or related disorders in general, were associated with a positive screening for ADHD only at the uncorrected level of analysis. No significant association with eating disorders, nor with gender, was observed. However, in subsample analyses (N = 95), ADHD symptoms were associated with mood and sleep problems, bulimic behaviors, greater harm avoidance, and lower self-directedness and cooperativeness.
The proportion of patients screening positive for adult ADHD was two to four times higher than the prevalence of adult ADHD in the general population [78,79,80]. This rate was consistent with the 12% prevalence of ADHD reported in youths with obesity aged 10 to 17 years [81]. Higher rates of ADHD or ADHD symptoms were previously repeatedly reported in adult samples with obesity, with estimates ranging between 27 and 38% in multiple studies [19, 46, 47, 51, 82]. Nevertheless, most of the studies had low sample sizes and only few reports included more than one hundred of patients [19, 45, 48, 50, 51]. Among these latter, prevalence rates ranged from 5.6% [50] to 27.4–28.3% [19, 51] in studies based on clinical interviews, and hovered around 10.2–12.1% in studies relying on self-report screening measures [45, 48]. A similar proportion of patients screening positive for adult ADHD (8.9%) was found in 90 individuals with severe obesity considering bariatric surgery [49].
Our finding is consistent with estimates from previous studies using self-report screening questionnaires in patients referred to bariatric surgery. The discrepancy with other studies may be attributed to differences in setting and assessment methods. First, it could be hypothesized that less patients with ADHD or with ADHD symptoms, such as disorganization or impulsivity, are referred to bariatric surgery than to other weight loss programs. Moreover, it could be possible that screening measures developed in the general population may have less validity in patients with obesity, especially during presurgical evaluations. However, it could not be excluded that the higher prevalence obtained through patients’ interviews in other studies may have been partly inflated by lack of third-party information on childhood behavior.
As concerns psychiatric comorbidity, in our study, the strongest association of a positive screening for ADHD was observed for anxiety disorders, especially panic disorder. Comorbidity between panic disorder and ADHD has been seldom examined and mixed results emerged from comparisons between adults with ADHD and healthy controls [83, 84]. Although panic disorder was found to be the least common anxiety disorder in children with ADHD [85] and, in a Japanese study, the polygenic risk for ADHD was found to be negatively associated with panic disorder [86], a recent study found a relatively high comorbidity with panic disorder in adults with ADHD, second only to social anxiety disorder [87]. Importantly, stronger correlations between ADHD and anxiety symptoms than between ADHD and depressive symptoms have been previously observed in bariatric surgery candidates [45]. It may be posited that demographic factors, such as female gender predominance [84], and specific ADHD features, such as predominantly inattentive presentation and sluggish cognitive tempo, previously associated both with obesity [19, 88] and anxiety comorbidity [89], may be related to the high prevalence of anxiety disorders in patients with obesity reporting ADHD symptoms. Interestingly, lifetime anxiety disorders have been recently associated with greater impairments in delay discounting in patients seeking bariatric surgery [50].
Eating disorders were not significantly overrepresented among our patients with obesity with a positive screening for ADHD. However, when evaluating the eating pattern using the BITE questionnaire, patients who screened positive for ADHD scored significantly higher than those who did not on the symptom scale, but not on the severity scale. This implies a presence of more disordered eating behaviors, though not a higher frequency of bulimic symptoms. While population studies generally supported the association between ADHD and eating disorders [8], previous studies conducted in samples with obesity failed to identify increased rates of binge-eating disorder diagnoses in patients with ADHD [48, 49]. However, ADHD symptoms were positively associated with disordered eating patterns, loss of control over eating, and emotional cravings in candidates for bariatric surgery [45].
Eating behaviors not specifically addressed by current nosographic conceptualizations, such as loss of control over eating, craving for palatable foods, and emotional hunger, may be especially relevant in patients with obesity with ADHD or significant ADHD symptoms and warrant further investigation [8, 27, 90, 91]. Among these constructs, night-eating was specifically investigated in our study. While sleep disturbances were more frequently reported by patients with a positive screening for ADHD, no significant associations with nocturnal ingestions, nor with evening hyperphagia were observed. In contrast, a previous study found that, among patients with obesity, those screening positive for ADHD reported more frequently than the others to wake up at night to eat [91]. Moreover, according to an online survey of university students, those diagnosed with night-eating syndrome had more often than others a history of ADHD [92]. Given the paucity of studies, both in patients with and without obesity, more research is needed.
Finally, temperament and character dimensions were evaluated. ADHD symptoms were positively associated with harm-avoidant temperamental traits and negatively associated with self-directedness and cooperativeness character facets. Both high harm avoidance, the tendency to inhibit or avoid responses to aversive stimuli, and low self-directedness, the capacity to control, regulate, and modify behavior to fulfil one’s objectives and uphold one’s values, had been previously strongly associated with ADHD in adult samples [61]. Low self-directedness may reflect deficits in executive functioning and self-regulation observed in patients with ADHD [93], and may be associated with suboptimal outcomes of obesity treatment [94]. Also, cooperativeness, the propensity for identification with, and acceptance of others, has shown moderate negative associations with ADHD in previous studies [61].
Surprisingly, instead, no significant association was observed with novelty seeking, the tendency to approach novel situations for rewards. Novelty seeking had been previously strongly associated with ADHD both in adults and in children [61]. However, while novelty-seeking shows a closer relationship with hyperactivity/impulsivity symptoms, higher inattention symptoms have been associated with decreased self-directedness and increased harm avoidance [95, 96]. Predominantly inattentive manifestations of ADHD in patients with obesity could thereby explain the lack of association between ADHD symptoms and novelty-seeking in our sample.
Interestingly, a cluster analysis applied to TCI scores of 463 patients with obesity and binge-eating behaviors revealed a cluster of patients with higher harm avoidance and lower self-directedness showing greater depressive symptoms, higher eating impulsivity, more problems with body image and poorer quality of life, but no differences in BMI or prevalence of binge-eating disorder vs. eating disorder not otherwise specified [97], whether ADHD might subtend the manifestations of this more complex variant of eating disorders in patients with obesity warrant more investigation in future studies.
Importantly, high harm avoidance, low self-directedness, and low cooperativeness have been found to characterize, among women with ADHD, those with more pronounced borderline personality traits [98]. Personality disorders have been associated with suboptimal clinical outcomes of bariatric surgery [99]. Considering the potential benefits of treating ADHD in patients with personality disorders [100, 101], the assessment of ADHD could merit further attention in patients with personality disorders seeking bariatric treatment.
Some important limitations of this study should be considered. First, the cross-sectional study design limited the assessment of psychiatric comorbidity to retrospective accounts, which may be at risk of recall bias. Moreover, information on remission status or current psychopharmacotherapy were not systematically recorded. More importantly, ADHD was not systematically investigated by the evaluating clinician, and no retrospective assessment of childhood symptoms was conducted. The recognition of ADHD symptoms was based on a self-report screening questionnaire rather than on a structured diagnostic interview performed by an experienced psychiatrist, which limits the validity of the results. Indeed, while the validation of the screening tool used was performed in an outpatient ADHD consultation unit, where the proportion of individuals with ADHD was higher than in the general population, no studies were conducted in community samples, where lower positive predictive values are expected based on the prevalence of ADHD. In addition, the recruitment occurred during routinely performed presurgical evaluations, which could lead some patients to underreport psychopathological symptoms to avoid to prejudice surgery.
Despite these flaws, our findings are in line with previous studies reporting similar prevalence of patients screening positive for ADHD in bariatric samples. While preliminary, our study benefited from a relatively large sample size and contributed to characterizing a potential psychological and behavioral phenotype in patients with obesity marked by ADHD symptoms, anxiety disorders, bulimic behaviors, polymorphic psychopathological manifestations, sleep disturbances, and maladaptive character traits. Drawing from previous studies, it might be hypothesized that these patients could also exhibit a higher severity of depressive symptoms [48, 97], more psychotherapy contact in the past [48], poorer body image and quality of life [97], higher eating impulsivity and food cravings [45, 97], and potentially poorer outcomes of obesity treatment [30,31,32, 94].
It remains to be explored whether a categorical diagnosis of ADHD or, alternatively, transdiagnostic psychopathological features, such as impulsivity or emotional dysregulation, or neuropsychological impairments of executive functioning better capture the complexity of patients with obesity and more severe psychopathology, as well as predict therapeutic outcomes. Further studies assessing both adulthood and childhood ADHD symptoms through validated clinical interviews as well as related attention deficits and executive dysfunctions through neuropsychological testing needs to be done to establish the prevalence of ADHD and to confirm or confute our findings and hypotheses. Longitudinal studies are also necessary to assess whether the phenotype outlined in this study, and which specific features within it, might be predictive of unfavorable surgery outcomes in bariatric patients. Moreover, a larger range of overweight conditions, as well as a controlled design, will be needed in future studies to investigate whether different ADHD features are more prevalent in patients with different BMI.
From a clinical perspective, diagnosing and treating ADHD in patients with obesity may have relevant implications. As previously mentioned, there is some indication that ADHD treatment might potentially reduce psychopathology severity in patients with comorbid personality disorders [100, 101] and improve response inhibition and delay discounting [41,42,43]. These changes, albeit indirectly, could potentially have a positive impact on bariatric surgery outcomes. Additionally, ADHD treatment might support long-term weight loss in individuals with suboptimal clinical response [32].
Based on our findings, patients with obesity showing comorbid anxiety disorders, especially panic disorder, high severity of psychopathological symptoms, sleep disturbances, bulimic behaviors, and specific character traits may screen positive for ADHD and, consequently, deserve further clinical assessment and management before bariatric surgery.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mansur RB, Brietzke E, McIntyre RS. Is there a “metabolic-mood syndrome”? A review of the relationship between obesity and mood disorders. Neurosci Biobehav Rev. 2015;52:89–104. https://doi.org/10.1016/j.neubiorev.2014.12.017.
McElroy SL, Crow S, Blom TJ, et al. Prevalence and correlates of DSM-5 eating disorders in patients with bipolar disorder. J Affect Disord. 2016;191:216–21. https://doi.org/10.1016/j.jad.2015.11.010.
Sarwer DB, Allison KC, Wadden TA, et al. Psychopathology, disordered eating, and impulsivity as predictors of outcomes of bariatric surgery. Surg Obes Relat Dis. 2019;15:650–5. https://doi.org/10.1016/j.soard.2019.01.029.
Segura-Garcia C, Caroleo M, Rania M, et al. Binge eating disorder and bipolar spectrum disorders in obesity: psychopathological and eating behaviors differences according to comorbidities. J Affect Disord. 2017;208:424–30. https://doi.org/10.1016/J.JAD.2016.11.005.
Brancati GE, Barbuti M, Calderone A, et al. Prevalence and psychiatric comorbidities of night-eating behavior in obese bariatric patients: preliminary evidence for a connection between night-eating and bipolar spectrum disorders. Eat Weight Disord. 2021. https://doi.org/10.1007/s40519-021-01306-1.
Weiss F, Barbuti M, Carignani G, et al. Psychiatric aspects of obesity: a narrative review of pathophysiology and psychopathology. J Clin Med. 2020;9:2344. https://doi.org/10.3390/jcm9082344.
Gillberg C, Gillberg IC, Rasmussen P, et al. Co-existing disorders in ADHD? implications for diagnosis and intervention. Eur Child Adolesc Psychiatry. 2004;13. https://doi.org/10.1007/s00787-004-1008-4.
Kaisari P, Dourish CT, Higgs S. Attention deficit hyperactivity disorder (ADHD) and disordered eating behaviour: a systematic review and a framework for future research. Clin Psychol Rev. 2017;53:109–21. https://doi.org/10.1016/J.CPR.2017.03.002.
Miller TW, Nigg JT, Faraone SV. Axis I and II comorbidity in adults with ADHD. J Abnorm Psychol. 2007;116:519–28. https://doi.org/10.1037/0021-843X.116.3.519.
Sobanski E, Brüggemann D, Alm B, et al. Psychiatric comorbidity and functional impairment in a clinically referred sample of adults with attention-deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci. 2007;257:371–7. https://doi.org/10.1007/s00406-007-0712-8.
Lin Y-J, Yang L-K, Gau SS-F. Psychiatric comorbidities of adults with early- and late-onset attention-deficit/hyperactivity disorder. Aust N Z J Psychiatry. 2016;50:548–56. https://doi.org/10.1177/0004867415609423.
Groenman AP, Janssen TWP, Oosterlaan J. Childhood psychiatric disorders as risk factor for subsequent substance abuse: a meta-analysis. J Am Acad Child Adolesc Psychiatry. 2017;56:556–69. https://doi.org/10.1016/j.jaac.2017.05.004.
Lee SS, Humphreys KL, Flory K, et al. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clin Psychol Rev. 2011;31:328–41. https://doi.org/10.1016/j.cpr.2011.01.006.
Erskine HE, Norman RE, Ferrari AJ, et al. Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2016;55:841–50. https://doi.org/10.1016/j.jaac.2016.06.016.
Meinzer MC, Pettit JW, Viswesvaran C. The co-occurrence of attention-deficit/hyperactivity disorder and unipolar depression in children and adolescents: a meta-analytic review. Clin Psychol Rev. 2014;34:595–607. https://doi.org/10.1016/j.cpr.2014.10.002.
Brancati GE, Perugi G, Milone A, et al. Development of bipolar disorder in patients with attention-deficit/hyperactivity disorder: a systematic review and meta-analysis of prospective studies. J Affect Disord. 2021;293:186–96. https://doi.org/10.1016/j.jad.2021.06.033.
Cortese S, Moreira-Maia CR, St Fleur D, et al. Association between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 2016;173:34–43. https://doi.org/10.1176/appi.ajp.2015.15020266.
Cortese S, Vincenzi B. Obesity and ADHD: Clinical and neurobiological implications. Curr Top Behav Neurosci. 2012;9:199–218. https://doi.org/10.1007/7854_2011_154.
Altfas JR. Prevalence of attention deficit/hyperactivity disorder among adults in obesity treatment. BMC Psychiatry. 2002;2:9. https://doi.org/10.1186/1471-244X-2-9.
Nigg JT, Johnstone JM, Musser ED, et al. Attention-deficit/hyperactivity disorder (ADHD) and being overweight/obesity: new data and meta-analysis. Clin Psychol Rev. 2016;43:67–79. https://doi.org/10.1016/j.cpr.2015.11.005.
Sandra Kooij JJ. ADHD and obesity. 101176/appi.ajp201515101315. 2016;173:1–2. https://doi.org/10.1176/APPI.AJP.2015.15101315.
Cortese S. The association between ADHD and obesity: intriguing, progressively more investigated, but still puzzling. Brain Sci. 2019;9:256. https://doi.org/10.3390/brainsci9100256.
Seymour KE, Reinblatt SP, Benson L, et al. Overlapping neurobehavioral circuits in ADHD, obesity, and binge eating: evidence from neuroimaging research. CNS Spectr. 2015;20:401–11. https://doi.org/10.1017/S1092852915000383.
Karhunen V, Bond TA, Zuber V, et al. The link between attention deficit hyperactivity disorder (ADHD) symptoms and obesity-related traits: genetic and prenatal explanations. Transl Psychiatry. 2021;11:455. https://doi.org/10.1038/s41398-021-01584-4.
Gunstad J, Paul RH, Cohen RA, et al. Elevated body mass index is associated with executive dysfunction in otherwise healthy adults. Compr Psychiatry. 2007;48:57–61. https://doi.org/10.1016/j.comppsych.2006.05.001.
Hanć T, Cortese S. Attention deficit/hyperactivity-disorder and obesity: a review and model of current hypotheses explaining their comorbidity. Neurosci Biobehav Rev. 2018;92:16–28. https://doi.org/10.1016/j.neubiorev.2018.05.017.
Davis C. Attention-deficit/hyperactivity disorder: associations with overeating and obesity. Curr Psychiatry Rep. 2010;12:389–95. https://doi.org/10.1007/S11920-010-0133-7.
Van Veen MM, Kooij JJS, Boonstra AM, et al. Delayed circadian rhythm in adults with attention-deficit/hyperactivity disorder and chronic sleep-onset insomnia. Biol Psychiatry. 2010;67:1091–6. https://doi.org/10.1016/j.biopsych.2009.12.032.
Vogel SWN, Bijlenga D, Tanke M, et al. Circadian rhythm disruption as a link between attention-deficit/hyperactivity disorder and obesity? J Psychosom Res. 2015;79:443–50. https://doi.org/10.1016/J.JPSYCHORES.2015.10.002.
Cortese S, Castellanos FX. The relationship between ADHD and obesity: implications for therapy. 101586/147371752014904748. 2014;14:473–479. https://doi.org/10.1586/14737175.2014.904748.
Mocanu V, Tavakoli I, MacDonald A, et al. The impact of ADHD on outcomes following bariatric surgery: a systematic review and meta-analysis. Obes Surg. 2019;29:1403–9. https://doi.org/10.1007/s11695-019-03735-5.
Levy LD, Fleming JP, Klar D. Treatment of refractory obesity in severely obese adults following management of newly diagnosed attention deficit hyperactivity disorder. Int J Obes. 2009;33(3):326–34. https://doi.org/10.1038/ijo.2009.5.
Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121:65–94. https://doi.org/10.1037/0033-2909.121.1.65.
Sonuga-Barke EJS. Causal models of attention-deficit/hyperactivity disorder: from common simple deficits to multiple developmental pathways. Biol Psychiatry. 2005;57:1231–8. https://doi.org/10.1016/j.biopsych.2004.09.008.
Mole TB, Irvine MA, Worbe Y, et al. Impulsivity in disorders of food and drug misuse. Psychol Med. 2015;45:771–82. https://doi.org/10.1017/S0033291714001834.
Bickel WK, Freitas-Lemos R, Tomlinson DC, et al. Temporal discounting as a candidate behavioral marker of obesity. Neurosci Biobehav Rev. 2021;129:307–29. https://doi.org/10.1016/j.neubiorev.2021.07.035.
Bartholdy S, Dalton B, O’Daly OG, et al. A systematic review of the relationship between eating, weight and inhibitory control using the stop signal task. Neurosci Biobehav Rev. 2016;64:35–62. https://doi.org/10.1016/j.neubiorev.2016.02.010.
Du Z, Li J, Huang J, et al. Executive functions in predicting weight loss and obesity indicators: a meta-analysis. Front Psychol. 2021;11. https://doi.org/10.3389/fpsyg.2020.604113.
Galioto R, Bond D, Gunstad J, et al. Executive functions predict weight loss in a medically supervised weight loss programme. Obes Sci Pract. 2016;2:334–40. https://doi.org/10.1002/osp4.70.
Kulendran M, Borovoi L, Purkayastha S, et al. Impulsivity predicts weight loss after obesity surgery. Surg Obes Relat Dis. 2017;13:1033–40. https://doi.org/10.1016/j.soard.2016.12.031.
Tamminga HGH, Reneman L, Huizenga HM, et al. Effects of methylphenidate on executive functioning in attention-deficit/hyperactivity disorder across the lifespan: a meta-regression analysis. Psychol Med. 2016;46:1791–807. https://doi.org/10.1017/S0033291716000350.
Campez M, Raiker JS, Little K, et al. An evaluation of the effect of methylphenidate on working memory, time perception, and choice impulsivity in children with ADHD. Exp Clin Psychopharmacol. 2022;30:209–19. https://doi.org/10.1037/pha0000446.
Shiels K, Hawk LW, Reynolds B, et al. Effects of methylphenidate on discounting of delayed rewards in attention deficit/hyperactivity disorder. Exp Clin Psychopharmacol. 2009;17:291–301. https://doi.org/10.1037/a0017259.
Leib S, Gilon Mann T, Stein D, et al. High prevalence of attention-deficit/hyperactivity disorder in adolescents with severe obesity seeking bariatric surgery. Acta Paediatr Int J Paediatr. 2020;109:581–6. https://doi.org/10.1111/apa.15039.
Alfonsson S, Parling T, Ghaderi A. Screening of adult ADHD among patients presenting for bariatric surgery. Obes Surg. 2012;22:918–26. https://doi.org/10.1007/s11695-011-0569-9.
Nicolau J, Ayala L, Francés C, et al. Are subjects with criteria for adult attention-deficit/ hyperactivity disorder doing worse after bariatric surgery? A case-control study. Nutr Hosp. 2014;31:1052–8. https://doi.org/10.3305/nh.2015.31.3.8089.
Marchesi DG, Ciriaco JGM, Miguel GPS, et al. O Transtorno de déficit de atenção e hiperatividade interfere nos resultados da cirurgia bariátrica? Rev Col Bras Cir. 2017;44:140–6. https://doi.org/10.1590/0100-69912017002006.
Gruss B, Mueller A, Horbach T, et al. Attention-deficit/hyperactivity disorder in a prebariatric surgery sample. Eur Eat Disord Rev. 2012;20:103–7. https://doi.org/10.1002/erv.1128.
Müller A, Claes L, Mitchell JE, et al. Binge eating and temperament in morbidly obese prebariatric surgery patients. Eur Eat Disord Rev. 2012;20:91–5. https://doi.org/10.1002/erv.1126.
Sarwer DB, Wadden TA, Ashare RL, et al. Psychopathology, disordered eating, and impulsivity in patients seeking bariatric surgery. Surg Obes Relat Dis. 2021;17:516–24. https://doi.org/10.1016/j.soard.2020.11.005.
Nazar BP, de Sousa Pinna CM, Suwwan R, et al. ADHD rate in obese women with binge eating and bulimic behaviors from a weight-loss clinic. J Atten Disord. 2016;20:610–6. https://doi.org/10.1177/1087054712455503.
First MB, Gibbon M. The structured clinical interview for DSM-IV axis I disorders (SCID-I) and the structured clinical interview for DSM-IV axis II disorders (SCID-II). In: Hilsenroth J, Segal DL, editors. Comprehensive handbook of psychological assessment, Vol. 2. Personality assessment. John Wiley; 2004. pp. 134–143.
Jones-Corneille LR, Wadden TA, Sarwer DB, et al. Axis i psychopathology in bariatric surgery candidates with and without binge eating disorder: results of structured clinical interviews. Obes Surg. 2012;22:389–97. https://doi.org/10.1007/s11695-010-0322-9.
Kalarchian MA, Marcus MD, Levine MD, et al. Psychiatric disorders among bariatric surgery candidates: relationship to obesity and functional health status. Am J Psychiatry. 2007;164:328–34. https://doi.org/10.1176/ajp.2007.164.2.328.
Mitchell JE, Selzer F, Kalarchian MA, et al. Psychopathology before surgery in the longitudinal assessment of bariatric surgery-3 (LABS-3) psychosocial study. Surg Obes Relat Dis. 2012;8:533–41. https://doi.org/10.1016/j.soard.2012.07.001.
Mauri M, Rucci P, Calderone A, et al. Axis I and II disorders and quality of life in bariatric surgery candidates. J Clin Psychiatry. 2008;69:295–301. https://doi.org/10.4088/JCP.v69n0216.
Rosenberger PH, Henderson KE, Grilo CM. Psychiatric disorder comorbidity and association with eating disorders in bariatric surgery patients. J Clin Psychiatry. 2006;67:1080–5. https://doi.org/10.4088/JCP.v67n0710.
Mühlhans B, Horbach T, de Zwaan M. Psychiatric disorders in bariatric surgery candidates: a review of the literature and results of a German prebariatric surgery sample. Gen Hosp Psychiatry. 2009;31:414–21. https://doi.org/10.1016/j.genhosppsych.2009.05.004.
Barbuti M, Brancati GE, Calderone A, et al. Prevalence of mood, panic and eating disorders in obese patients referred to bariatric surgery: patterns of comorbidity and relationship with body mass index. Eat Weight Disord. 2021. https://doi.org/10.1007/s40519-021-01236-y.
Pinzone V, De Rossi P, Trabucchi G, et al. Temperament correlates in adult ADHD: a systematic review (bigstar bigstar). J Affect Disord. 2019;252:394–403. https://doi.org/10.1016/j.jad.2019.04.006.
Gomez R, Van Doorn G, Watson S, et al. Cloninger’s personality dimensions and ADHD: a meta-analytic review. Pers Individ Dif. 2017;107:219–27. https://doi.org/10.1016/j.paid.2016.11.054.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC; 2000.
Derogatis, LR, SCL-90-R revised manual. Baltimore: Johns Hopkins University School of Medicine; 1983.
Ransom D, Ashton K, Windover A, Heinberg L. Internal consistency and validity assessment of SCL-90-R for bariatric surgery candidates. Surg Obes Relat Dis. 2010;6:622–7. https://doi.org/10.1016/j.soard.2010.02.039.
Bianciardi E, Gentileschi P, Niolu C, et al. Assessing psychopathology in bariatric surgery candidates: discriminant validity of the SCL-90-R and SCL-K-9 in a large sample of patients. Eat Weight Disord. 2021;26:2211–8. https://doi.org/10.1007/s40519-020-01068-2.
Abbass K, Corbisiero S, Stieglitz RD. Development and psychometric properties of the ADHD-SCL-90-R screening scale for adult ADHD. J Clin Psychol. 2021;77:1428–42. https://doi.org/10.1002/jclp.23088.
Conners CK, Erhardt D, Sparrow EP. Conners’ adult ADHD rating scales (CAARS): technical manual. NY: Multi-Health Systems North Tonawanda; 1999.
Allison KC, Lundgren JD, O’Reardon JP, et al. The Night Eating Questionnaire (NEQ): psychometric properties of a measure of severity of the Night Eating Syndrome. Eat Behav. 2008;9:62–72. https://doi.org/10.1016/j.eatbeh.2007.03.007.
Aloi M, Rania M, De Fazio P, et al. Validation of the Italian version of the Night Eating Questionnaire (I-NEQ). J Psychopathol. 2017;23:137–44.
Orlandi E, Mannucci E, Cuzzolaro M. Bulimic Investigatory Test, Edinburgh (BITE). A validation study of the Italian version. Eat Weight Disord. 2005;10. https://doi.org/10.1007/BF03354662.
Henderson M, Freeman CPL. A self-rating scale for bulimia: the “BITE.” Br J Psychiatry. 1987;150:18–24. https://doi.org/10.1192/bjp.150.1.18.
Cloninger CR. A psychobiological model of temperament and character. Arch Gen Psychiatry. 1993;50:975. https://doi.org/10.1001/archpsyc.1993.01820240059008.
Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The temperament and character inventory (TCI): a guide to its development and use. Center for. St. Louis; 1994.
Sato T, Narita T, Hirano S, et al. Factor validity of the temperament and character inventory in patients with major depression. Compr Psychiatry. 2001;42:337–41. https://doi.org/10.1053/comp.2001.24587.
Brändström S, Schlette P, Przybeck TR, et al. Swedish normative data on personality using the temperament and character inventory. Compr Psychiatry. 1998;39:122–8. https://doi.org/10.1016/S0010-440X(98)90070-0.
de la Rie SM, Duijsens IJ, Cloninger CR. Temperament, character, and personality disorders. J Pers Disord. 1998;12:362–72. https://doi.org/10.1521/pedi.1998.12.4.362.
Di Lorenzo N, Antoniou SA, Batterham RL, et al. Clinical practice guidelines of the European Association for Endoscopic Surgery (EAES) on bariatric surgery: update 2020 endorsed by IFSO-EC, EASO and ESPCOP. Surg Endosc. 2020;34:2332–58. https://doi.org/10.1007/s00464-020-07555-y.
Fayyad J, Sampson NA, Hwang I, et al. The descriptive epidemiology of DSM-IV Adult ADHD in the World Health Organization World Mental Health Surveys. ADHD Atten Defic Hyperact Disord. 2017;9:47–65. https://doi.org/10.1007/s12402-016-0208-3.
Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716–23. https://doi.org/10.1176/ajp.2006.163.4.716.
Simon V, Czobor P, Bálint S, et al. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194:204–11. https://doi.org/10.1192/bjp.bp.107.048827.
Halfon N, Larson K, Slusser W. Associations between obesity and comorbid mental health, developmental, and physical health conditions in a nationally representative sample of us children aged 10 to 17. Acad Pediatr. 2013;13:6–13. https://doi.org/10.1016/j.acap.2012.10.007.
Fleming JP, Levy LD, Levitan RD. Symptoms of attention deficit hyperactivity disorder in severely obese women. Eat Weight Disord. 2005;10:10–3. https://doi.org/10.1007/BF03354661.
O’Rourke SR, Bray AC, Anastopoulos AD. Anxiety symptoms and disorders in college students with ADHD. J Atten Disord. 2020;24:1764–74. https://doi.org/10.1177/1087054716685837.
Cumyn L, French L, Hechtman L. Comorbidity in adults with attention-deficit hyperactivity disorder. Can J Psychiat. 2009;54:673–83. https://doi.org/10.1177/070674370905401004.
Eser HY, Kacar AS, Kilciksiz CM, et al. Prevalence and associated features of anxiety disorder comorbidity in bipolar disorder: a meta-analysis and meta-regression study. Front Psychiatry. 2018;9. https://doi.org/10.3389/fpsyt.2018.00229.
Ohi K, Otowa T, Shimada M, et al. Shared transethnic genetic basis of panic disorder and psychiatric and related intermediate phenotypes. Eur Neuropsychopharmacol. 2021;42:87–96. https://doi.org/10.1016/j.euroneuro.2020.11.003.
Quenneville AF, Kalogeropoulou E, Nicastro R, et al. Anxiety disorders in adult ADHD: a frequent comorbidity and a risk factor for externalizing problems. Psychiatry Res. 2022;310:1–6. https://doi.org/10.1016/j.psychres.2022.114423.
Öğütlü H, Karatekin Ş, Sürücü Kara İ, McNicholas F. Sluggish cognitive tempo, eating habits, and daytime sleepiness in obese adolescents. 101177/13591045221105194. 2022. https://doi.org/10.1177/13591045221105194.
Schatz DB, Rostain AL. ADHD with comorbid anxiety. A review of the current literature. J Atten Disord. 2006;10:141–9. https://doi.org/10.1177/1087054706286698.
El Archi S, Cortese S, Ballon N, et al. Negative affectivity and emotion dysregulation as mediators between adhd and disordered eating: a systematic review. Nutrients. 2020;12:1–34. https://doi.org/10.3390/nu12113292.
Docet MF, Larrañaga A, Pérez Méndez LF, García-Mayor RV. Attention deficit hyperactivity disorder increases the risk of having abnormal eating behaviours in obese adults. Eat Weight Disord. 2012;17:132–6. https://doi.org/10.1007/BF03325337.
Runfola CD, Allison KC, Hardy KK, et al. Prevalence and clinical significance of night eating syndrome in university students. J Adolesc Health. 2014;55:41–8. https://doi.org/10.1016/J.JADOHEALTH.2013.11.012.
Nigg JT. Annual Research Review: On the relations among self-regulation, self-control, executive functioning, effortful control, cognitive control, impulsivity, risk-taking, and inhibition for developmental psychopathology. J Child Psychol Psychiatry. 2017;58:361–83. https://doi.org/10.1111/jcpp.12675.
Dalle Grave R, Calugi S, El Ghoch M. Are personality characteristics as measured by the temperament and character inventory (TCI) associated with obesity treatment outcomes? A systematic review. Curr Obes Rep. 2018;7:27–36. https://doi.org/10.1007/s13679-018-0294-y.
Salgado CAI, Bau CHD, Grevet EH, et al. Inattention and hyperactivity dimensions of ADHD are associated with different personality profiles. Psychopathology. 2009;42:108–12. https://doi.org/10.1159/000203343.
Perroud N, Hasler R, Golay N, et al. Personality profiles in adults with attention deficit hyperactivity disorder (ADHD). BMC Psychiatry. 2016;16:1–9. https://doi.org/10.1186/s12888-016-0906-6.
Leombruni P, Rocca G, Fassino S, et al. An exploratory study to subtype obese binge eaters by personality traits. Psychother Psychosom. 2014;83:114–8. https://doi.org/10.1159/000356810.
Van Dijk FE, Lappenschaar M, Kan CC, et al. Symptomatic overlap between attention-deficit/hyperactivity disorder and borderline personality disorder in women: the role of temperament and character traits. Compr Psychiatry. 2012;53:39–47. https://doi.org/10.1016/j.comppsych.2011.02.007.
Livhits M, Mercado C, Yermilov I, et al. Preoperative predictors of weight loss following bariatric surgery: systematic review. Obes Surg. 2012;22:70–89. https://doi.org/10.1007/s11695-011-0472-4.
Lieslehto J, Tiihonen J, Lähteenvuo M, et al. Association of pharmacological treatments and real-world outcomes in borderline personality disorder. Acta Psychiatr Scand. 2023;147:603–13. https://doi.org/10.1111/acps.13564.
Prada P, Nicastro R, Zimmermann J, et al. Addition of methylphenidate to intensive dialectical behaviour therapy for patients suffering from comorbid borderline personality disorder and ADHD: a naturalistic study. ADHD Attent Defic Hyperact Disord. 2015;7:199–209. https://doi.org/10.1007/s12402-015-0165-2.
Funding
Open access funding provided by Università di Pisa within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Ferruccio Santini, Giulio Perugi and Margherita Barbuti contributed to the study conception and design. Recruitment and data collection were performed by Alba Calderone, Paola Fierabracci and Guido Salvetti. Margherita Barbuti and Francesco Weiss designed and prepared the database. Statistical analyses and interpretation of the data were performed by Giulio Emilio Brancati. The first draft of the manuscript was written by Giulio Emilio Brancati and Viarda Cosentino and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Competing Interests
Prof. Perugi acted as consultant to Lundbeck, Angelini, FB-Health. He received a scholarship/research support from Lundbeck and Angelini. He is a member of the speaker/advisory board of Sanofi-Aventis, Lundbeck, FB-Health, Angelini. Prof. Santini has acted as a consultant, has received grant/research support and/or is on the speaker/advisory board for NovoNordisk, Bruno Farmaceutici, Aegerion-Amrit, Bio Italia srl. Other authors have no affiliation or financial interest in any organization that may constitute a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• Positive screening for ADHD found in 11.5% of 260 candidates for bariatric surgery.
• ADHD symptoms associated with panic disorder and psychopathology severity.
• ADHD severity correlated with mood and sleep problems, and bulimic behaviors.
• Greater harm avoidance, lower self-directedness, and lower cooperativeness.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brancati, G.E., Cosentino, V., Barbuti, M. et al. Prevalence and Correlates of Self-Reported ADHD Symptoms in Bariatric Patients: Focus on Mood and Anxiety Comorbidity, Disordered Eating, and Temperamental Traits. OBES SURG (2024). https://doi.org/10.1007/s11695-024-07308-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11695-024-07308-z