Abstract
Background
In the field of bariatric surgery, research on symptoms of adult attention deficit hyperactivity disorder (ADHD) and their interrelationships with other psychological risk factors such as depression and anxiety is scarce. The symptoms of adult ADHD seem to be common in the obese population, but they are rarely investigated before bariatric surgery. ADHD-related symptoms such as impulsivity have at the same time been identified as potential risk factors for less successful weight loss among bariatric surgery patients. The aims of the current study were to screen for symptoms of adult ADHD and to investigate their relationships with other psychological risk factors.
Methods
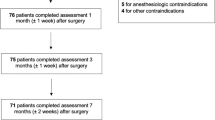
Candidates for bariatric surgery (N = 187) were anonymously screened for symptoms of anxiety, depression, and adult ADHD, in addition to disordered eating patterns, by means of questionnaires. The relations between these symptoms were investigated.
Results
In the current sample, 10% of patients screened positively for adult ADHD, and the symptoms of adult ADHD were significantly correlated with those of anxiety, depression, and disordered eating.
Conclusions
The results show that adult ADHD is more common in this clinical group than in the general population (4%) and that adult ADHD is associated with disordered eating patterns, depression, and anxiety. Further prospective research, using multivariate analysis, is needed to investigate whether the symptoms of adult ADHD, and their interaction with anxiety, depression, or disordered eating, may possibly constitute a risk factor in terms of difficulties in adhering to the post-surgery regime and its potential unfavorable outcome.
Similar content being viewed by others
References
Sjostrom L, Lindroos A, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
Luppino F, De Wit L, Bouvy P, et al. Overweight, obesity, and depression. Arch Gen Psychiatry. 2010;67:220–9.
Simon GE, Von Korff M, Saunders K, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63:824–30.
Gertler R, Ramsey Stewart G. Pre-operative psychiatric assessment of patients presenting for gastric bariatric surgery (surgery control of morbid obesity). Aust N Z J Surg. 1986;56:157–61.
Solow C, Silberfarb PM, Swift K. Psychosocial effects of intestinal bypass surgery for severe obesity. N Engl J Med. 1974;290:300–4.
Ashton D, Favretti F, Segato G. Preoperative psychological testing—another form of prejudice. Obes Surg. 2008;18:1330–7.
Odom J, Zalesin K, Washington T, et al. Behavioral predictors of weight regain after bariatric surgery. Obes Surg. 2010;20:349–56.
Van Hout GCM, Verschure SKM, Van Heck GL. Psychosocial predictors of success following bariatric surgery. Obes Surg. 2005;15:552–60.
de Zwaan M, Enderle J, Wagner S, et al. Anxiety and depression in bariatric surgery patients: a prospective, follow-up study using structured clinical interviews. J Affect Disord. 2011;133(1–2):61–8.
Herpertz S, Kielmann R, Wolf A, et al. Do psychosocial variables predict weight loss or mental health after obesity surgery? A systematic review. Obesity (Silver Spring). 2004;12:1554–69.
Katon W, Ciechanowski P. Impact of major depression on chronic medical illness. J Psychosom Res. 2002;53:859–63.
Lin EHB, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154–60.
Elkins G, Whitfield P, Marcus J, et al. Noncompliance with behavioral recommendations following bariatric surgery. Obes Surg. 2005;15(4):546–51.
Pontiroli AE, Fossati A, Vedani P, et al. Post-surgery adherence to scheduled visits and compliance, more than personality disorders, predict outcome of bariatric restrictive surgery in morbidly obese patients. Obes Surg. 2007;17:1492–7.
Toussi R, Fujioka K, Coleman KJ. Pre- and postsurgery behavioral compliance, patient health, and postbariatric surgical weight loss. Obesity (Silver Spring). 2009;17:996–1002.
DiMatteo M, Lepper H, Croghan T. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7.
McNally K, Rohan J, Pendley JS, et al. Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care. 2010;33:1159–62.
Goodman DW. The consequences of attention-deficit/hyperactivity disorder in adults. J Psychiatr Pract. 2007;13:318–27.
Fried M, Hainer V, Basdevant A, et al. Interdisciplinary European guidelines on surgery of severe obesity. Obes Facts. 2008;1:52–9.
Mechanick J, Kushner R, Sugerman H, et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery Medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Surg Obes Relat Dis. 2008;4:109–84.
Pull CB. Current psychological assessment practices in obesity surgery programs: what to assess and why. Curr Opin Psychiatry. 2010;23:30–6.
LeMont D, Moorehead M, Parish M, et al. Suggestions for the pre-surgical psychological assessment of bariatric surgery candidates. American Society for Bariatric Surgery. 2004;1–29.
Walfish S, Vance D, Fabricatore A. Psychological evaluation of bariatric surgery applicants: procedures and reasons for delay or denial of surgery. Obes Surg. 2007;17:1578–83.
Friedman KE, Applegate KL, Grant J. Who is adherent with preoperative psychological treatment recommendations among weight loss surgery candidates? Surg Obes Relat Dis. 2007;3:376–82.
Tsuda S, Barrios L, Schneider B, et al. Factors affecting rejection of bariatric patients from an academic weight loss program. Surg Obes Relat Dis. 2009;5:199–202.
Mühlhans B, Horbach T, de Zwaan M. Psychiatric disorders in bariatric surgery candidates: a review of the literature and results of a German prebariatric surgery sample. Gen Hosp Psychiatry. 2009;31:414–21.
APA. DSM-IV: diagnostic and statistical manual of mental disorders. Washington: American Psychiatric Association; 1994.
Davidson M. ADHD in adults: a review of the literature. J Atten Disord. 2008;11:628–41.
Faraone SV, Sergeant J, Gillberg C, et al. The worldwide prevalence of ADHD: is it an American condition? World Psychiatr. 2003;2:104–13.
Kessler RC, Adler L, Barkley R, et al. Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: results from the national comorbidity survey replication. Biol Psychiatry. 2005;57:1442–51.
Faraone SV, Biederman J. What is the prevalence of adult ADHD? Results of a population screen of 966 adults. J Atten Disord. 2005;9:384–91.
Simon V, Czobor P, Balint S, et al. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194:204–11.
Altfas J. Prevalence of attention deficit/hyperactivity disorder among adults in obesity treatment. BMC Psychiatry. 2002;2:9.
Cortese S, Angriman M, Maffeis C, et al. Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Crit Rev Food Sci Nutr. 2008;48:524–37.
Pagoto S, Curtin C, Lemon S, et al. Association between adult attention deficit/hyperactivity disorder and obesity in the US population. Obesity (Silver Spring). 2009;17:539–44.
Bazar K, Yun A, Lee P, et al. Obesity and ADHD may represent different manifestations of a common environmental oversampling syndrome: a model for revealing mechanistic overlap among cognitive, metabolic, and inflammatory disorders. Med Hypotheses. 2006;66:263–9.
Davis C. Attention-deficit/hyperactivity disorder: associations with overeating and obesity. Curr Psychiatry Rep. 2010;1–7.
Fuemmeler B, Østbye T, Yang C, et al. Association between attention-deficit/hyperactivity disorder symptoms and obesity and hypertension in early adulthood: a population-based study. Int J Obes. 2010;852–62.
Cortese S, Morcillo PC. Comorbidity between ADHD and obesity: exploring shared mechanisms and clinical implications. Postgrad Med. 2010;122:88–96.
Lokken K, Boeka A, Yellumahanthi K, et al. Cognitive performance of morbidly obese patients seeking bariatric surgery. Am Surg. 2010;76:55–9.
Cortese S, Bernardina B, Mouren M. Attention deficit/hyperactivity disorder (ADHD) and binge eating. Nutr Rev. 2007;65:404–11.
Davis C. Psychobiological traits in the risk profile for overeating and weight gain. Int J Obes. 2009;33:S49–53.
Davis C, Patte K, Levitan RD, et al. A psycho-genetic study of associations between the symptoms of binge eating disorder and those of attention deficit (hyperactivity) disorder. J Psychiatr Res. 2009;43(7):687–96.
de Zwaan M. Binge eating disorder and obesity. Int J Obes Suppl. 2001;25:51–5.
Bauchowitz A, Gonder-Frederick L, Olbrisch M, et al. Psychosocial evaluation of bariatric surgery candidates: a survey of present practices. Psychosom Med. 2005;67:825–32.
Colles S, Dixon J, O’Brien P. Grazing and loss of control related to eating: two high-risk factors following bariatric surgery. Obesity (Silver Spring). 2008;16:615–22.
Niego S, Kofman M, Weiss J, et al. Binge eating in the bariatric surgery population: a review of the literature. Int J Eat Disord. 2007;40:349–59.
Sallet P, Sallet J, Dixon J, et al. Eating behavior as a prognostic factor for weight loss after gastric bypass. Obes Surg. 2007;17:445–51.
Sarwer DB, Wadden TA, Moore RH, et al. Preoperative eating behavior, postoperative dietary adherence, and weight loss after gastric bypass surgery. Surg Obes Relat Dis. 2008;4:640–6.
White MA, Kalarchian MA, Masheb RM, et al. Loss of control over eating predicts outcomes in bariatric surgery: a prospective 24-month follow-up study. J Clin Psychiatry. 2010;71:175–84.
Allison KC, Wadden TA, Sarwer DB, et al. Night eating syndrome and binge eating disorder among persons seeking bariatric surgery: prevalence and related features. Surg Obes Relat Dis. 2006;2:153–8.
Canetti L, Berry E, Elizur Y. Psychosocial predictors of weight loss and psychological adjustment following bariatric surgery and a weight loss program: the mediating role of emotional eating. Int J Eat Disord. 2009;42:109–17.
Rusch M, Andris D. Maladaptive eating patterns after weight-loss surgery. Nutr Clin Pract. 2007;22:41–9.
Leite F, de Oliveira K, Pereira F, et al. Snack-eating patients experience lesser weight loss after Roux-en-Y gastric bypass surgery. Obes Surg. 2009;19:1293–6.
Gorin AA, Raftopoulos I. Effect of mood and eating disorders on the short-term outcome of laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2009;19:1685–90.
Heinberg L, Ashton K, Windover A. Moving beyond dichotomous psychological evaluation: the Cleveland Clinic Behavioral Rating System for weight loss surgery. Surg Obes Relat Dis. 2010;6:185–90.
Lanyon R, Maxwell B. Predictors of outcome after gastric bypass surgery. Obes Surg. 2007;17:321–8.
Kessler RC, Adler L, Ames M, et al. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–56.
Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70.
Bjelland I, Dahl A, Haug T, et al. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52:69–77.
de Man Lapidoth J, Ghaderi A, Halvarsson-Edlund K, et al. Psychometric properties of the Eating Disorders in Obesity questionnaire: validating against the Eating Disorder Examination interview. Eat Weight Disord. 2007;12:168–75.
Celio AA, Wilfley DE, Crow SJ, et al. A comparison of the binge eating scale, questionnaire for eating and weight patterns revised, and eating disorder examination questionnaire with instructions with the eating disorder examination in the assessment of binge eating disorder and its symptoms. Int J Eat Disord. 2004;36(4):434–44.
White MA, Grilo CM. Diagnostic efficiency of DSM-IV indicators for binge eating episodes. J Consult Clin Psychol. 2011;79:75–83.
Nijs IM, Franken IH, Muris P. The modified Trait and State Food-Cravings Questionnaires: development and validation of a general index of food craving. Appetite. 2007;49:38–46.
SPSS. SPSS 18.0 statistical package for social sciences: SPSS 18.0 for Windows user’s guide. Chicago: SPSS; 2010.
Karlsson J, Taft C, Rydén A, et al. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes. 2007;31:1248–61.
Burgmer R, Petersen I, Burgmer M, et al. Psychological outcome two years after restrictive bariatric surgery. Obes Surg. 2007;17:785–91.
de Zwaan M, Mitchell JE, Howell LM, et al. Characteristics of morbidly obese patients before gastric bypass surgery. Compr Psychiatry. 2003;44:428–34.
Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Compr Psychiatry. 2007;48:124–31.
Sarwer DB, Cohn NI, Gibbons LM, et al. Psychiatric diagnoses and psychiatric treatment among bariatric surgery candidates. Obes Surg. 2004;14:1148–56.
Wilfley DE, Schwartz MB, Spurrell EB, et al. Assessing the specific psychopathology of binge eating disorder patients: interview or self-report? Behav Res Ther. 1997;35:1151–9.
Livingston EH, Ko CY. Socioeconomic characteristics of the population eligible for obesity surgery. Surgery. 2004;135:288–96.
Lutfi R, Torquati A, Sekhar N, et al. Predictors of success after laparoscopic gastric bypass: a multivariate analysis of socioeconomic factors. Surg Endosc. 2006;20:864–7.
Rutledge T, Groesz LM, Savu M. Psychiatric factors and weight loss patterns following gastric bypass surgery in a veteran population. Obes Surg. 2009;21:29–35.
Pataky Z, Carrard I, Golay A. Psychological factors and weight loss in bariatric surgery. Curr Opin Gastroenterol. 2011;27:167–73.
Adler LD, Nierenberg AA. Review of medication adherence in children and adults with ADHD. Postgrad Med. 2010;122:184–91.
Mitchell JE, Steffen KJ, de Zwaan M, et al. Congruence between clinical and research-based psychiatric assessment in bariatric surgical candidates. Surg Obes Relat Dis. 2010;6:628–634
Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716–23.
Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66:1254–69.
Wilson KG, Eriksson MY, D’Eon JL, et al. Major depression and insomnia in chronic pain. Clin J Pain. 2002;18:77–83.
Conflicts of Interest
The authors Sven Alfonsson, Thomas Parling, and Ata Ghaderi declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alfonsson, S., Parling, T. & Ghaderi, A. Screening of Adult ADHD Among Patients Presenting for Bariatric Surgery. OBES SURG 22, 918–926 (2012). https://doi.org/10.1007/s11695-011-0569-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-011-0569-9