Abstract
Bariatric surgery remains the most effective treatment for morbid obesity and its comorbidities. However, post-surgical leaks and fistulas can occur in about 1–5% of patients, with challenging treatment approaches. Endoscopic vacuum therapy (EVT) has emerged as a promising tool due to its satisfactory results and accessibility. In this first systematic review and meta-analysis on the subject, EVT revealed rates of 87.2% clinical success, 6% moderate adverse events, and 12.5% system dislodgements, requiring 6.47 EVT system exchanges every 4.39 days, with a dwell time of 25.67 days and a total length of hospitalization of 44.43 days. Although our results show that EVT is a safe and effective therapy for post-surgical leaks and fistulas, they should be interpreted with caution due to the paucity of available data.
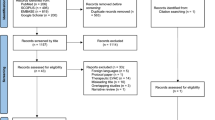
Graphical abstract










Similar content being viewed by others
References
O’Brien PE, Hindle A, Brennan L, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg Internet. 2019;29:3–14 Available from: http://www.ncbi.nlm.nih.gov/pubmed/30293134.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev [Internet]. 2014;CD003641. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25105982
Schulman AR, Thompson CC. Complications of bariatric surgery: what you can expect to see in your GI practice. Am J Gastroenterol Internet. 2017;112:1640–55 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/28809386).
Moura D, Oliveira J, De Moura EGH, et al. Effectiveness of intragastric balloon for obesity: a systematic review and meta-analysis based on randomized control trials. Surg Obes Relat Dis Internet. 2016;12:420–9 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/26968503).
Zellmer JD, Mathiason MA, Kallies KJ, et al. Is laparoscopic sleeve gastrectomy a lower risk bariatric procedure compared with laparoscopic Roux-en-Y gastric bypass? A meta-analysis. Am J Surg Internet. 2014;208:903–10 (discussion 909-10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25435298).
Cariani S, Nottola D, Grani S, et al. Complications after gastroplasty and gastric bypass as a primary operation and as a reoperation. Obes Surg Internet. 2001;11:487–90 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/11501361).
Haito-Chavez Y, Kumbhari V, Ngamruengphong S, et al. Septotomy: an adjunct endoscopic treatment for post-sleeve gastrectomy fistulas. Gastrointest Endosc Internet. 2016;83:456–7 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/26358326).
Haito-Chavez Y, Law JK, Kratt T, et al. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc Internet. 2014;80:610–22 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/24908191).
Lippert E, Klebl FH, Schweller F, et al. Fibrin glue in the endoscopic treatment of fistulae and anastomotic leakages of the gastrointestinal tract. Int J Colorectal Dis Internet. 2011;26:303–11 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/21190028).
Mukewar S, Kumar N, Catalano M, et al. Safety and efficacy of fistula closure by endoscopic suturing: a multi-center study. Endoscopy Internet. 2016;48:1023–8 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/27576179).
Schmidt F, Mennigen R, Vowinkel T, et al. Endoscopic vacuum therapy (EVT)-a new concept for complication management in bariatric surgery. Obes Surg Internet. 2017;27:2499–505 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/28695459).
Okazaki O, Bernardo WM, Brunaldi VO, et al. Efficacy and safety of stents in the treatment of fistula after bariatric surgery: a systematic review and meta-analysis. Obes Surg Internet. 2018;28:1788–96 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/29654447).
Gonzalez JM, Lorenzo D, Guilbaud T, et al. Internal endoscopic drainage as first line or second line treatment in case of postsleeve gastrectomy fistulas. Endosc Int open Internet. 2018;6:E745–50 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/29876512).
Kumbhari V, Cummings DE, Kalloo AN, et al. AGA Clinical practice update on evaluation and management of early complications after bariatric/metabolic surgery: expert review. Clin Gastroenterol Hepatol Internet. 2021;19:1531–7 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/33741500).
Vargas EJ, Abu Dayyeh BK. Keep calm under pressure: a paradigm shift in managing postsurgical leaks. Gastrointest Endosc Internet. 2018;87:438–41 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/29406928).
de Moura DTH, de Moura BFBH, Manfredi MA, et al. Role of endoscopic vacuum therapy in the management of gastrointestinal transmural defects. World J Gastrointest Endosc Internet. 2019;11:329–44.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev Internet. 2015;4:1 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/25554246).
Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc Internet. 2010;71:446–54 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/20189503).
Munn Z, Barker TH, Moola S, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth Internet. 2020;18:2127–33 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/33038125).
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ Internet. 2008;336:924–6 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/18436948).
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol Internet. 2005;5:13 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/15840177).
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997.
Morell B, Murray F, Vetter D, et al. Endoscopic vacuum therapy (EVT) for early infradiaphragmal leakage after bariatric surgery—outcomes of six consecutive cases in a single institution. Langenbeck’s Arch Surg Internet. 2019;404:115–21 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/30645682).
Christogianni V, Bemponis P, Buesing M, et al. O-068: The endoscopic-vacuum assisted closure-technique in the treatment of staple line leaks after sleeve gastrectomy. Obes Surg Internet. 2018;28:1–130 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/29693216).
Archid R, Bazerbachi F, Abu Dayyeh BK, et al. Endoscopic negative pressure therapy (ENPT) is superior to stent therapy for staple line leak after sleeve gastrectomy: a single-center cohort study. Obes Surg Internet. 2021;31:2511–9 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/33650088).
Leeds SG, Burdick JS. Management of gastric leaks after sleeve gastrectomy with endoluminal vacuum (E-Vac) therapy. Surg Obes Relat Dis Internet. 2016;12:1278–85 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/27178614).
Zaveri H, Surve A, Cottam D, Richards C, et al. A142 - Management of upper gastro-intestinal leaks with endoscopic vaccum-assisted closure system (E- VAC): two center experience. 34th Annu Meet Am Soc Metab Bariatr Surg [Internet]. 2017; Available from: https://asmbs.org/app/uploads/2018/03/ASMBS-2017-Abstract-Book-1.pdf
Donatelli G, Dumont J-L, Cereatti F, et al. Endoscopic internal drainage as first-line treatment for fistula following gastrointestinal surgery: a case series. Endosc Int Open Internet. 2016;04:E647–51 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/27556072).
Willingham FF, Buscaglia JM. Endoscopic management of gastrointestinal leaks and fistulae. Clin Gastroenterol Hepatol Internet. 2015;13:1714–21 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/25697628).
Newton NJ, Sharrock A, Rickard R, et al.. Systematic review of the use of endo-luminal topical negative pressure in oesophageal leaks and perforations. Dis esophagus Off J Int Soc Dis Esophagus Internet. 2017;30:1–5 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/27628015).
Rached AA. Gastric leaks post sleeve gastrectomy: review of its prevention and management. World J Gastroenterol Internet. 2014;20:13904 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/25320526).
de Moura DTH, Hirsch BS, Do Monte Junior ES, et al. Cost-effective modified endoscopic vacuum therapy for the treatment of gastrointestinal transmural defects: step-by-step process of manufacturing and its advantages. VideoGIE Internet. 2021;6:523–8 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/34917860).
de Moura DTH, do Monte Junior ES, Hathorn KE, et al. The use of novel modified endoscopic vacuum therapies in the management of a transmural rectal wall defect. Endoscopy [Internet]. 2020. Available from: http://www.thieme-connect.de/DOI/DOI?10.1055/a-1173-7727
de Moura DTH, do Monte Junior ES, Hathorn KE, et al. Modified endoscopic vacuum therapy in the management of a duodenal transmural defect. Endoscopy [Internet]. 2020; Available from: http://www.thieme-connect.de/DOI/DOI?https://doi.org/10.1055/a-1173-7282
Kuehn F, Loske G, Schiffmann L, et al. Endoscopic vacuum therapy for various defects of the upper gastrointestinal tract. Surg Endosc Internet. 2017;31:3449–58 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/28078463).
de Moura DTH, Hirsch BS, Boghossian MB, et al. Low-cost modified endoscopic vacuum therapy using a triple-lumen tube allows nutrition and drainage for treatment of an early post–bariatric surgery leak. Endoscopy [Internet]. 2021; Available from: http://www.ncbi.nlm.nih.gov/pubmed/34374043
Neumann P-A, Mennigen R, Palmes D, et al. Pre-emptive endoscopic vacuum therapy for treatment of anastomotic ischemia after esophageal resections. Endoscopy Internet. 2017;49:498–503.
Gubler C, Vetter D, Schmidt HM, et al. Preemptive endoluminal vacuum therapy to reduce anastomotic leakage after esophagectomy: a game-changing approach? Dis Esophagus [Internet]. 2019;32. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30596963
Loske G, Müller J, Schulze W, et al. Pre-emptive active drainage of reflux (PARD) in Ivor-Lewis oesophagectomy with negative pressure and simultaneous enteral nutrition using a double-lumen open-pore film drain (dOFD). Surg Endosc Internet. 2022;36:2208–16 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/34973079).
de Medeiros FS, do Junior ESM, de França RL, et al. Preemptive endoluminal vacuum therapy after pancreaticoduodenectomy: a case report. World J Gastrointest Endosc Internet. 2020;12:493–9.
de Moura DTH, de Moura EGH, Hirsch BS, et al. Endoscopic vacuum therapy for duodenal hemorrhage in critically ill patients with COVID-19. Am J Gastroenterol Internet. 2022;117:688–688 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/35137700).
de Moura EGH, Silva GLR, de Moura ETH, et al. Esophageal perforation after epicardial ablation: an endoscopic approach. Endoscopy Internet. 2015;47(Suppl 1):E592–3 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/26671539).
Sachdev AH, Iqbal S, Ribeiro IB, et al. Use of omental patch and endoscopic closure technique as an alternative to surgery after endoscopic full thickness resection of gastric intestinal stromal tumors: a series of cases. World J Clin Cases Internet. 2020;8:120–5 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/31970177).
Barrichello Junior SA, Ribeiro IB, Fittipaldi-Fernandez RJ, et al. Exclusively endoscopic approach to treating gastric perforation caused by an intragastric balloon: case series and literature review. Endosc Int Open Internet. 2018;06:E1322–9.
Cereatti F, Grassia R, Drago A, et al. Endoscopic management of gastrointestinal leaks and fistulae: what option do we have? World J Gastroenterol Internet. 2020;26:4198–217 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/32848329).
de Moura DTH, Boghossian MB, Hirsch BS, et al. Long-term endoscopic follow-up after closure of a post-bariatric surgery fistula with a cardiac septal defect occluder. Endoscopy Internet. 2022;54:E127–8 (Available from: http://www.ncbi.nlm.nih.gov/pubmed/33862651).
Boghossian MB, Funari MP, do Monte Junior ES, et al. Endoscopic septotomy for fistula after bariatric surgery. Endoscopy Internet. 2022;54:E38–9 Available from:http://www.ncbi.nlm.nih.gov/pubmed/33607658.
Author information
Authors and Affiliations
Contributions
Vera Intriago JM: acquisition of data, analysis, interpretation of data, drafting the article, revising the article, final approval; de Moura DTH: analysis and interpretation of data, revising the article; Proença IM and Monteiro Junior ES: acquisition of data, analysis, interpretation of data, drafting the article, revising the article, final approval; Ribeiro IB: drafting the article, revising the article, final approval; Sánchez-Luna SA: drafting the article, linguistic correction, revising the article, final approval; Bernardo WM: analysis and interpretation of data, drafting the article, final approval; de Moura EGH: analysis and interpretation of data, drafting the article, revising the article, final approval.
Corresponding author
Ethics declarations
Ethics Approval
The study was approved by the Research Ethics Committee. For this type of study, formal consent is not required.
Conflict of Interest
Dr. Diogo Turiani Hourneaux De Moura: BariaTek—Advisory Board Member (Consulting fees). Dr. Sergio A. Sanchéz-Luna: Recipient of the 2021 American Society for Gastrointestinal Endoscopy (ASGE) Endoscopic Training Award by the ASGE and Fujifilm. This was not relevant to this study. Dr. Eduardo Guimaraes Hourneaux De Moura: Olympus—Consultant (Consulting fees), Boston Scientific—Consultant (Consulting fees). They were not relevant to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Endoscopic vacuum therapy (EVT) showed high clinical success rates in the treatment of post-bariatric surgery leaks and fistulas.
• However, EVT may be associated with multiple endoscopic sessions and a long length of hospital stay.
• Adjunctive therapies could be performed during EVT when needed.
• Incidents such as EVT system dislodgment may occur in around 12.5% of cases. Moderate AEs occurred in 6% of the patients but no mortality or severe adverse events (AEs) related to the EVT were reported.
• Although this systematic review and meta-analysis, the first of its kind on the subject, showed that EVT is a safe and effective therapy, our results should be interpreted with caution due to the paucity of available data.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Intriago, J.M.V., de Moura, D.T.H., do Monte Junior, E.S. et al. Endoscopic Vacuum Therapy (EVT) for the Treatment of Post-Bariatric Surgery Leaks and Fistulas: a Systematic Review and Meta-analysis. OBES SURG 32, 3435–3451 (2022). https://doi.org/10.1007/s11695-022-06228-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06228-0