Abstract
Background
Bariatric surgery is being recognized increasingly as an effective treatment for obesity and related comorbidities. In Japan, the cost of laparoscopic sleeve gastrectomy (LSG) is covered by the national health insurance for adults with a body mass index (BMI) ≥ 35 kg/m2 and specific comorbidities (type 2 diabetes mellitus (T2DM), hypertension (HT), dyslipidemia (DL), and obstructive sleep apnea syndrome (OSAS)). However, only 0.6% of the adult population have a BMI ≥ 35 kg/m2. In contrast, 4.3% have class I obesity (a BMI of 30–34.9 kg/m2). The BMI of Asians with central obesity-induced diabetes and other metabolic disorders is much lower than that of Westerners.
Objectives
To evaluate the medium-term (up to 5 years) outcomes of LSG performed in Japanese patients with class I obesity.
Methods
One hundred eighteen consecutive patients with class I obesity treated by LSG at our center between August 2007 and December 2018 were included in a retrospective study. Mean preoperative body weight (BW) and BMI were 88.6 ± 10.3 kg and 32.8 ± 1.6 kg/m2, respectively. Weight loss, comorbidity status, and adverse events were assessed.
Results
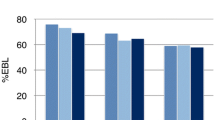
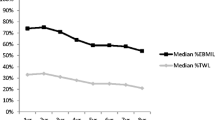
Mean BW/BMI at 1, 3, and 5 years after LSG decreased significantly to 66.6 ± 11.2 kg/24.6 ± 2.8 kg/m2, 68.0 ± 14.0 kg/25.4 ± 4.0 kg/m2, and 69.1 ± 12.9 kg/26.5 ± 3.0 kg/m2, respectively. Mean total weight loss at 1, 3, and 5 years was 24.7 ± 8.2%, 21.8 ± 12.1%, and 18.5 ± 9.7%, respectively. Metabolic disorders such as T2DM, HT, and DL improved significantly. There was no mortality.
Conclusion
LSG is safe, yields excellent weight loss, and improves obesity-related comorbidities in Japanese patients with class I obesity.

Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, et al. IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28:3783–94.
Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference statement. Am J Clin Nutr 1992;55(2 Suppl):615S–9S.
Bassett J, Organization WH. The Asia-Pacific perspective: redefining obesity and its treatment: Health Communications Australia; 2000.
Yoon KH, Lee JH, Kim JW, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–8.
Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Rubino F, Nathan DM, Eckel RH, et al. Delegates of the 2nd Diabetes Surgery Summit. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care. 2016;39:861–77.
Zimmet P, Alberti KG, Rubino F, et al. IDF’s view of bariatric surgery in type 2 diabetes. Lancet. 2011;378:108–10.
Kasama K, Lee WJ, Seki Y, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012;22:677–84.
Ohta M, Seki Y, Wong SK, et al. Bariatric/metabolic surgery in the Asia-Pacific region: APMBSS 2018 survey. Obes Surg. 2019;29:534–41.
Guidelines for clinical application of laparoscopic bariatric surgery. Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). http://www.sages.org/publications/guidelines/guidelines-for-clinical-application-of- laparoscopic-bariatricsurgery/.
Colles SL, Dixon JB, Marks P, et al. Preoperative weight loss with a very-low-energy diet: quantitation of changes in liver and abdominal fat by serial imaging. Am J Clin Nutr. 2006;8:304–11.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Shimamoto K, Ando K, Fujita T, et al. Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014;37:253–390.
Teramoto T, Sasaki J, Ueshima H, et al. Japan Atherosclerosis Society (JAS) Committee for Epidemiology and Clinical Management of Atherosclerosis. Diagnostic criteria for dyslipidemia. Executive summary of Japan Atherosclerosis Society (JAS) guideline for diagnosis and prevention of atherosclerotic cardiovascular diseases for Japanese. J Atheroscler Thromb. 2007;14:155–8.
Brethauer SA, Kim J, el Chaar M, et al. ASMBS Clinical Issues Committee. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis. 2015;11:489–506.
Kramer H, Cao G, Dugas L, et al. Increasing BMI and waist circumference and prevalence of obesity among adults with type 2 diabetes: the national health and nutrition examination surveys. J Diabetes Complicat. 2010;24:368–74.
Japan Diabetes Clinical Data Management Study Group. http://jddm.jp/data/index-2017/.
World Health Organization. Global Health Observatory data. https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adults/en/.
International Diabetes Federation. https://idf.org/our-network/regions-members/.
Guh DP, Zhang W, Bansback N, et al. The incidence of co-morbidities related to obesity and over-weight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719–29.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Aminian A, Chang J, Brethauer SA, et al. American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. ASMBS updated position statement on bariatric surgery in class I obesity (BMI 30-35 kg/m2). Surg Obes Relat Dis. 2018;14:1071–87.
Hsu CC, Almulaifi A, Chen JC, et al. Effect of bariatric surgery vs medical treatment on type 2 diabetes in patients with body mass index lower than 35: five-year outcomes. JAMA Surg. 2015;150:1117–24.
Amin A, Siddiq G, Haider MI, et al. Laparoscopic sleeve gastrectomy versus lifestyle modification in class i obesity in Pakistani population: a prospective cohort study. Cureus. 2019;11:e5031.
Ismail M, Nagaraj D, Rajagopal M, et al. Seven-year outcomes of laparoscopic sleeve gastrectomy in Indian patients with different classes of obesity. Obes Surg. 2019;29:191–6.
Hong JS, Kim WW, Han SM. Five-year results of laparoscopic sleeve gastrectomy in Korean patients with lower body mass index (30-35 kg/m2). Obes Surg. 2015;25:824–9.
Park JY, Kim YJ. Efficacy of laparoscopic sleeve gastrectomy in mildly obese patients with body mass index of 30-35 kg/m2. Obes Surg. 2015;25:1351–7.
Seki Y, Kasama K, Yasuda K, et al. The effects of laparoscopic sleeve gastrectomy with duodenojejunal bypass on Japanese patients with BMI <35 kg/m2 on type 2 diabetes mellitus and the prediction of successful glycemic control. Obes Surg. 2018;28:2429–38.
Lee WJ, Hur KY, Lakadawala M, et al. Predicting success of metabolic surgery: age, body mass index, C-peptide, and duration score. Surg Obes Relat Dis. 2013;9:379–84.
Naitoh T, Kasama K, Seki Y, et al. Efficacy of sleeve gastrectomy with duodenal-jejunal bypass for the treatment of obese severe diabetes patients in Japan: a retrospective multicenter study. Obes Surg. 2018;28:497–505.
Lee WJ, Chong K, Ser KH, et al. Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg. 2011;146:143–8.
Robert M, Denis A, Badol-Van Straaten P, et al. Prospective longitudinal assessment of change in health-related quality of life after adjustable gastric banding. Obes Surg. 2013;23:1564–70.
Schauer PR, Bhatt DL, Kirwan JP, et al. STAMPEDE investigators. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376:641–51.
Lee WJ, Lee MH, Yu PJ, et al. Gastro-intestinal quality of life after metabolic surgery for the treatment of type 2 diabetes mellitus. Obes Surg. 2015;25:1371–9.
Seki Y, Pantanakul S, Kasama K, et al. Impact of metabolic surgery on health-related quality of life and quality of alimentation. Surg Obes Relat Dis. 2019;15:488–96.
Ollendorf DA, Cameron CG, Pearson SD. Effectiveness and value of treatment options for obesity--a report for the California technology assessment forum. JAMA Intern Med. 2016;176:247–8.
Acknowledgments
The authors thank Prof. Tina Tajima of St. Marianna University School of Medicine for her meticulous English editing.
Funding
The study was funded by departmental resources only.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no commercial associations that might constitute a conflict of interest related to this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethics approval of this study was granted by the Institutional Review Board of Yotsuya Medical Cube (Ref No. YCR19006).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seki, Y., Kasama, K., Kikkawa, E. et al. Five-Year Outcomes of Laparoscopic Sleeve Gastrectomy in Japanese Patients with Class I Obesity. OBES SURG 30, 4366–4374 (2020). https://doi.org/10.1007/s11695-020-04789-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04789-6