Abstract
Background
Venous thromboembolism (VTE) is the most frequent 30-day complication in patients with morbid obesity undergoing bariatric surgery. Therefore, there is a need for optimized low molecular weight heparin (LMWH) thromboprophylaxis dosing strategies in order to avoid VTE-associated morbidity and mortality in this patient population.
Objective
The primary goal was to evaluate if a pre-specified enoxaparin dosing regimen in patients undergoing bariatric surgery reaches anti-factor Xa (aFXa) levels in the defined target range (0.2–0.4 U/ml). Second, we aimed to identify biometric and laboratory parameters that might influence the aFXa value.
Methods
A prospective database of 236 patients with obesity who received thromboprophylaxis with enoxaparin was established. These patients were divided into two weight-adjusted groups (group 1 < 150 kg, group 2 ≥ 150 kg). Enoxaparin was administered twice daily; dosing was determined by weight (group 1, 2 × 40 mg/day; group 2, 2 × 60 mg/day). In both groups, the peak aFXa serum level was evaluated 3 days after initiating the thromboprophylaxis.
Results
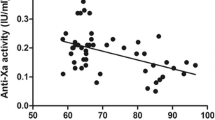
In group 1 (body mass index (BMI) 42.94 ± 6.84 kg/m2, weight of 121.7 ± 17.49 kg), seventy-one of the included 124 patients (57.25%) reached the aFXa target range of 0.2 to 0.4 U/m. In group 2 (BMI 63.21 ± 10.05 kg/m2, weight of 191.66 ± 33.37 kg), 68 of 112 (60.71%) patients scored prophylactic aFXa range. Multiple regression of the biometric and laboratory parameters showed significance for weight, waist-to-hip ratio, glomerular filtration rate (GFR), creatinine, and HbA1c exclusively in group 1. There was no case of VTE within 3 months after surgery and no case of severe perioperative bleeding in those patients who underwent surgery.
Conclusions
Measurement of the aFXa level helps to define the real prophylactic thromboprophylaxis status in patients with obesity, especially in those with a weight above 150 kg. In patients at risk, the measurement of aFXa should be considered in routine clinical practice.




Similar content being viewed by others
References
Chang SH, Freeman NLB, Lee JA, et al. Early major complications after bariatric surgery in the USA, 2003-2014: a systemic review and meta-analysis. Obes Rev. 2018;19(4):529–37.
Daigle CR, Brethauer SA, Tu C, et al. Which postoperative complications matters most after bariatric surgery? Prioritizing quality improvement efforts to improve national outcome. SOARD. 2018;14(5):652–7.
Venclauskas L, Maleckas A, Arcelus JI, et al. European guidelines on perioperative venous thromboembolism prophylaxis: surgery in the obese patient. Eu J Anaestesiol. 2018;35(2):147–53.
Hamadi R, Marlow CF, Nasseredidne S, et al. Bariatric venous thromboembolism prophylaxis: an update on the literature. Expert Rev Hematol. 2019;20
Bartlett MA, Mauck KF, Daniels PR. Prevention of venous thromboembolism in patients undergoing bariatric surgery. Vasc Health Risk Manag. 2015;11:461–77.
Shelkrot M, Miraka J, Perez ME. Appropriate enoxaparin dose for venous thromboembolism prophylaxis in patients with extreme obesity. Hosp Pharm. 2014;49(8):740–7.
Vilahur G et al. New insights into the role of adipose tissue in thrombosis. Cardiovasc Res. 2017;113(9):1046–54.
Chiappetta S, Schaak HM, Wölnerhannsen B, et al. The impact of obesity and metabolic surgery on chronic inflammation. Obes Surg. 2018;28(10):3028–40.
Müller S, Runkel N. Delphi survey: anticoagulation in obese patients. Bariatric surgery consensus on antithrombotic prophylaxis. CHAZ. 2017;3(18):127–32.
Moulin PA, Dutour A, Ancel P, et al. Perioperative thromboprophylaxis in severely obese patients undergoing bariatric surgery: insights from a French national survey. SOARD. 2017;13:320–6.
Rowan BO, Kuhl DA, Lee MD, et al. Anti-Xa levels in bariatric surgery patients receiving prophylactic enoxaparin. Obes Surg. 2008;18:162–6.
Ikesaka R, Delluc A, Le Gal G, et al. Efficacy and safety of weight-adjusted heparin prophylaxis for the prevention of acute venous thromboembolism among obese patients undergoing bariatric surgery: a systematic review and meta-analysis. Thromb Res. 2014;133(4):682–7.
Aminian A, Andalip A, Khorgami Z, et al. Who should get extended thromboprophylaxis after bariatric surgery? Ann Surg. 2017;265(1):143–50.
Kabrhel C, Varraso R, Goldhaber SZ, et al. Prospective study of BMI and the risk of pulmonary embolism in women. Obesity (Silver Spring). 2009;17(11):2040–6.
Khoursheed M, Al-Bader I, Al-Asfar F, et al. Therapeutic effect of low-molecular weight heparin and incidence of lower limb deep venous thrombosis and pulmonary embolism after laparoscopic bariatric surgery. Surg Lap Endosc Percutan Tech. 2013;23(6):491–3.
Kalfarentzos F, Stavropoulou F, Yarmenitis S, et al. Prophylaxis of venous thromboembolism using two different doses of low-molecular-weight heparin (nadroparin) in bariatric surgery: a prospective randomized trial. Obes Surg. 2001;11(6):670–6.
Scholten DJ, Hoedema RM, Scholten SE. A comparison of two different prophylactic dose regimens of low molecular weight heparin in bariatric surgery. Obes Surg. 2002;12(1):19–24.
Munoz_Atienza V, Gil-Rendo A, Amo-Salas M, et al. Extended use of bemiparin as thromboprophylaxis during bariatric surgery: results of anti-factor Xa activity. Surg Obes Relat Dis. 2018;14(3):354–60.
Author information
Authors and Affiliations
Contributions
All authors contributed to the article. CS designed the study and collected data. SC and RS calculated statistics. AK and SC improved the composition of the article with their wealth of knowledge. CS, SC, AK, RS, and AS reviewed and improved the article.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stier, C., Koschker, AC., Stier, R. et al. Are We Missing Treatment Standards for Thromboprophylaxis of the Obese and Super-Obese Patient Population? A Prospective Systematic Cohort Study. OBES SURG 30, 1704–1711 (2020). https://doi.org/10.1007/s11695-020-04383-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04383-w