Abstract
Background
Obesity and rapid weight loss after bariatric surgery (BS) are independent risk factors for development of cholelithiasis (CL), a prevalent disease in the Chilean population. This study aimed to determine the incidence of CL in obese Chilean patients 12 months after BS and identify risk factors for development of gallstones.
Methods
Retrospective study of patients who underwent BS in 2014. Patients with preoperative negative abdominal ultrasound (US) for CL and follow-up for at least than 12 months were included. Patients underwent US at 6 months and 12 months. We analyzed sex, age, hypertension, dyslipidemia, type 2 diabetes mellitus, body mass index (BMI), surgical procedure, percentage of excess BMI loss (%EBMIL) at 6 months, and BMI at 6 months.
Results
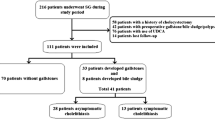
Of 279 patients who underwent bariatric surgery during 2014, 66 had previous gallbladder disease and 176 met the inclusion criteria (82.6%), while 54.6% were female. The mean age was 37.8 ± 10.5 years and preoperative BMI was 37.5 kg/m2. BMI and %EBMIL at 6 months were 27.8 ± 3.3 kg/m2 and 77.9 ± 33.6%, respectively. At 12 months after BS, CL was found in 65 patients (36.9%). Hypertension turned out to be protective against occurrence of gallstones at 1 year with an OR 0.241.
Conclusions
Incidence of CL was up to one-third of the patients followed up for 12 months after BS. Excessive weight loss and other variables studied did not increase risk. Hypertension seems to be protective against gallstone formation, but this result needs further analysis.

Similar content being viewed by others
Change history
28 May 2019
Due to a metadata tagging error the name of author Andrés Esteban San Martín was indexed incorrectly. The author’s given name is Andrés Esteban and his family name is San Martín.
References
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg. 2017;27(9):2279–89. https://doi.org/10.1007/s11695-017-2666-x.
Covarrubias C, Valdivieso V, Nervi F. Epidemiology of gallstone disease in Chile. In: Capocaccia L, Ricci G, Angelico F, Angelico M, Attili AF, editors. Epidemiology and prevention of gallstone disease. Dordrecht: Springer; 1984.
Amaral J, Thompson W. Gallbladder disease in the morbidly obese. Am J Surg. 1985;149(4):551–7.
Warschkow R, Tarantino I, Ukegjini K, et al. Concomitant cholecystectomy during laparoscopic Roux-en-Y gastric bypass in obese patients is not justified: a meta-analysis. Obes Surg. 2013;23(3):397–407. https://doi.org/10.1007/s11695-012-0852-4.
Shiffman ML, Sugerman HJ, Kellum JM, et al. Gallstone formation after rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am J Gastroenterol. 1991;86:1000–5.
Shiffman ML, Sugerman HJ, Kellum JH, et al. Gallstones in patients with morbid obesity: relationship to body weight, weight loss and gallbladder bile cholesterol solubility. Int J Obes Relat Metab Disord. 1993;17:153–8.
Sugerman HJ1, Brewer WH, Shiffman ML, Brolin RE, Fobi MA, Linner JH. A multicenter, placebo-controlled, randomized, double-blind, prospective trial of prophylactic ursodiol for the prevention of gallstone formation following gastric-bypass-induced rapid weight loss. Am J Surg 1995;169(1):91–96; discussion 96
Iglézias Brandão de Oliveira C, Adami Chaim E, da Silva BB. Impact of rapid weight reduction on risk of cholelithiasis after bariatric surgery. Obes Surg. 2003;13(4):625–8. https://doi.org/10.1381/096089203322190862.
Scott DJ, Villegas L, Sims TL, et al. Intraoperative ultrasound and prophylactic ursodiol for gallstone prevention following laparoscopic gastric bypass. Surg Endosc. 2003;17:1796–802.
Villegas L, Schneider B, Provost D, et al. Is routine cholecystectomy required during laparoscopic gastric bypass? Obes Surg. 2004;14:206–11.
Teivelis MP, Faintuch J, Ishida R, et al. Endoscopic and ultrasonographic evaluation before and after Roux-en-Y gastric bypass for morbid obesity. Arq Gastroenterol. 2007;44:8–13.
Nagem R, Lázaro-da-Silva A. Cholecystolithiasis after gastric bypass: a clinical, biochemical, and ultrasonographic 3-year follow-up study. Obes Surg. 2012;22(10):1594–9. https://doi.org/10.1007/s11695-012-0710-4.
Coupaye M, Castel B, Sami O, et al. Comparison of the incidence of cholelithiasis after sleeve gastrectomy and Roux-en-Y gastric bypass in obese patients_ a prospective study. Surg Obes Relat Dis. 2014;11(4):1–20. https://doi.org/10.1016/j.soard.2014.10.015.
Mishra T, Lakshmi KK, Peddi KK. Prevalence of cholelithiasis and choledocholithiasis in morbidly obese south Indian patients and the further development of biliary calculus disease after sleeve gastrectomy, gastric bypass and mini gastric bypass. Obes Surg. 2016;26(10):1–7. https://doi.org/10.1007/s11695-016-2113-4.
Wuttiporn Manatsathit MD, Pornchai Leelasincharoen MD, Hussein Al-Hamid MD, et al. The incidence of cholelithiasis after sleeve gastrectomy and its association with weight loss: an historical cohort study. Int J Surg. 2016;30:1–26. https://doi.org/10.1016/j.ijsu.2016.03.060.
Pacchioni M, Nicoletti C, Caminiti M, et al. Association of obesity and type II diabetes mellitus as a risk factor for gallstones. Dig Dis Sci. 2000;45(10):2002–6.
Paumgartner G, Sauerbruch T. Gallstones: pathogenesis. Lancet. 1991;338(8775):1117–21.
Bastouly M, Arasaki CH, Ferreira JB, et al. Early changes in postprandial gallbladder emptying in morbidly obese patients undergoing Roux-en-Y gastric bypass: correlation with the occurrence of biliary sludge and gallstones. Obes Surg. 2009;19(1):22–8. https://doi.org/10.1007/s11695-008-9648-y.
Alamo Alamo M, Sepúlveda Torres C, Zapata Perez L. Vertical isolated gastroplasty with gastro-enteral bypass: preliminary results. Obes Surg. 2006;16(3):353–8. https://doi.org/10.1381/096089206776116534.
Sepulveda M, Alamo M, Preiss Y, et al. Metabolic surgery comparing sleeve gastrectomy with jejunal bypass and Roux-en-Y gastric bypass in type 2 diabetic patients after 3 years. Obes Surg. 2018;28(11):3466–73. https://doi.org/10.1007/s11695-018-3402-x.
Lasnibat RJP, Molina FJC, Lanzarini SE, et al. Colelitiasis en pacientes obesos sometidos a cirugía bariátrica: estudio y seguimiento postoperatorio a 12 meses. Rev Chil Cir. 2017;69(1):49–52. https://doi.org/10.1016/j.rchic.2016.07.007.
Li VKM, Pulido N, Fajnwaks P, et al. Predictors of gallstone formation after bariatric surgery: a multivariate analysis of risk factors comparing gastric bypass, gastric banding, and sleeve gastrectomy. Surg Endosc. 2008;23(7):1640–4. https://doi.org/10.1007/s00464-008-0204-6.
Worni M, Guller U, Shah A, et al. Cholecystectomy concomitant with laparoscopic gastric bypass: a trend analysis of the nationwide inpatient sample from 2001 to 2008. Obes Surg. 2012;22(2):220–9. https://doi.org/10.1007/s11695-011-0575-y.
Amstutz S, Michel J-M, Kopp S, et al. Potential benefits of prophylactic cholecystectomy in patients undergoing bariatric bypass surgery. Obes Surg. 2015;25(11):2054–60. https://doi.org/10.1007/s11695-015-1650-6.
Nougou A, Suter M. Almost routine prophylactic cholecystectomy during laparoscopic gastric bypass is safe. Obes Surg. 2008;18(5):535–9. https://doi.org/10.1007/s11695-007-9368-8.
Villanueva L. Cancer of the gallbladder—Chilean statistics. Ecancermedicalscience. 2016;10:704.
Magouliotis DE, Tasiopoulou VS, Svokos AA, et al. Ursodeoxycholic acid in the prevention of gallstone formation after bariatric surgery: an updated systematic review and meta-analysis. Obes Surg. 2017;27(11):3021–30. https://doi.org/10.1007/s11695-017-2924-y.
Uy MC, Talingdan-Te MC, Espinosa WZ, et al. Ursodeoxycholic acid in the prevention of gallstone formation after bariatric surgery: a meta-analysis. Obes Surg. 2008;18:1532–8.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9(2):159–91. https://doi.org/10.1016/j.soard.2012.12.010.
Haute autorité de santé [homepage on the Internet]. Obésité, prise en charge chirurgicale chez l’adulte. [updated 2009 January]. Available from: www.has-sante.fr (Accessed 4 July 2018)
Acknowledgments
We thank Professor Waldo Aranda for his valuable contribution with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was previously approved by the scientific ethics committee of that same institution.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guzmán, H.M., Sepúlveda, M., Rosso, N. et al. Incidence and Risk Factors for Cholelithiasis After Bariatric Surgery. OBES SURG 29, 2110–2114 (2019). https://doi.org/10.1007/s11695-019-03760-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03760-4