Abstract
Purpose
Obesity and bariatric surgery are both risk factors for cholelithiasis (CL). However, most previous studies have focused on Roux-en-Y gastric bypass, and limited published data are available for sleeve gastrectomy (SG).
Methods
Patients were evaluated in two groups depending on the presence of gallstones (Group I, present; Group II, absent). Demographic characteristics, comorbid diseases, pre-operative blood values, and early and late weight loss rates were compared between the groups.
Results
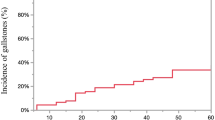
The study included 111 patients with a mean age of 38.9. The mean follow-up period was 20.6 (12–39) months. During follow-up, gallstone formation was observed in 36.9% (n = 41) of patients. Thirteen patients (31.8%) had symptomatic cholelithiasis that was resolved with laparoscopic cholecystectomy. The mean interval between sleeve gastrectomy and the detection of cholelithiasis was 210 days and the mean time of post-operative cholecystectomy was 540 days. A multivariate analysis showed that only dyslipidemia was independently and significantly associated with gallstone formation. There was no significant difference in the weight loss rate between the groups.
Conclusions
Although CL development was found to be associated with rapid weight loss in several published studies in post-SG patients, the present study showed no significant difference between the groups in terms of early or late weight loss. Pre-operative dyslipidemia may be associated with an increased risk of developing CL.

Similar content being viewed by others
References
Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–7.
Fahed AC, El-Hage-Sleiman AK, Farhat TI, Nemer GM. Diet, genetics, and disease: a focus on the middle east and north Africa region. J Nutr Metab. 2012;2012:109037.
Akkurt G, Buluş H, Alimoğulları M, Albuz Ö. Upper gastrointestinal endoscopy performed before sleeve gastrectomy in patients with morbid obesity retrospective analysis of 460 patients. Med J Islam World Acad Sci. 2018;26(3):70–3.
Nguyen NT, Nguyen B, Gebhart A, et al. Changes in the makeup of bariatric surgery: a national increase in use of laparoscopic sleeve gastrectomy. J Am Coll Surg. 2013;216:252–7.
Shiffman ML, Sugerman HJ, Kellum JM, Brewer WH, Moore EW. Gallstone formation after rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am J Gastroenterol. 1991;86:1000–5.
de Oliveira CIB, AdamiChaim E, da Silva BB. Impact of rapid weight reduction on risk of cholelithiasis after bariatric surgery. Obes Surg. 2003;13(4):625–8.
Moon RC, Teixeira AF, DuCoin C, Varnadore S, Jawad MA. Comparison of cholecystectomy cases after Roux-en-Y gastric bypass, sleeve gastrectomy, and gastric banding. Surg Obes Relat Dis. 2014;10(1):64–70.
Coupaye M, Castel B, Sami O, Tuyeras G, Msika S, Ledoux S. Comparison of the incidence of cholelithiasis after sleeve gastrectomy and Roux-en-Y gastric bypass in obese patients: a prospective study. Surg Obes Relat Dis. 2015;11(4):779–84. https://doi.org/10.1016/j.soard.2014.10.015.
Manatsathit W, Leelasinjaroen P, Al-Hamid H, Szpunar S, Hawasli A. The incidence of cholelithiasis after sleeve gastrectomy and its association with weight loss: a two-centre retrospective cohort study. Int J Surg. 2016;30:13–8.
Festi D, Dormi A, Capodicasa S, et al. Incidence of gallstone disease in Italy: results from a multicenter, population-based Italian study (the MICOL project). World J Gastroenterol. 2008;14(34):5282–9.
Grover BT, Kothari S. Biliary issues in the bariatric population. Surg Clin N Am. 2014;94(2):413–25.
Nakeeb A, Comuzzie AG, Martin L, Sonnenberg GE, Swartz-Basile D, Kissebah AH, et al. Gallstones: genetics versus environment. Ann Surg. 2002;235(6):842–9.
Abo-Ryia MH, Abd-Allah HS, El-Khadrawy OH, et al. Predictors of gallstone formation in morbidly obese patients after bariatric surgery: a retrospective observational study. Surg Sci. 2014;5:1–5.
Pezzolla F, Lantone G, Guerra V, et al. Influence of the method of digestive tract reconstruction on gallstone development after total gastrectomy for gastric cancer. Am J Surg. 1993;166(1):6–10.
Shiffman ML, Shamburek RD, Schwartz CC, et al. Gallbladder mucin, arachidonic acid, and bile lipids in patients who develop gallstones during weight reduction. Gastroenterology. 1993;105:1200–8.
Fisher RS, Rock E, Malmud LS. Effects of meal composition on gallbladder and gastric emptying in man. Dig Dis Sci. 1987;32:1337–444.
Sioka E, Zacharoulis D, Zachari E, Papamargaritis D, Pinaka O, Katsogridaki G, et al. Complicated gallstones after laparoscopic sleeve gastrectomy. J Obes. 2014;2014:468203. https://doi.org/10.1155/2014/468203.
Yardımcı S, Coskun M, Demircioglu S, Erdim A, Cingi A. Is concomitant cholecystectomy necessary for asymptomatic cholelithiasis during laparoscopic sleeve gastrectomy? Obes Surg. 2017. https://doi.org/10.1007/s11695-017-2867-3.
Nagem R, Lazaro-da-Silva A. Cholecystolithiasis after gastric bypass: a clinical, biochemical, and ultrasonographic 3-year follow-up study. Obes Surg. 2012;22:1594–9.
Li VK, Pulido N, Martinez-Suartez P, et al. Symptomatic gallstones after sleeve gastrectomy. Surg Endosc. 2009;23(11):2488–92.
Aridi HD, Sultanem S, Abtar H, et al. Management of gallbladder disease after sleeve gastrectomy in a selected Lebanese population. Surg Obes Rel Dis. 2016;12:1300–4.
Chang J, Corcelles R, Boules M, Jamal MH, Schauer PR, Kroh MD. Predictive factors of biliary complications after bariatric surgery. Surg Obes Rel Dis. 2016;12:1706–10.
Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Obesity (Silver Spring). 2009;17(1):1–70.
Li VK, Pulido N, Fajnwaks P, Szomstein S, Rosenthal R, Martinez-Duartez P. Predictors of gallstone formation after bariatric surgery: a multivariate analysis of risk factors comparing gastric bypass, gastric banding, and sleeve gastrectomy. Surg Endosc. 2009;23(7):1640–4.
Warschkow R, Tarantino I, Ukegjini K, et al. Concomitant cholecystectomy during laparoscopic Roux-en-Y gastric by pass in obese patients. Is not justified: a meta-analysis. Obes Surg. 2013;23(3):397–407.
Yang H, Petersen GM, Roth MP, Schoenfield LJ, Marks JW. Risk factors for gallstone formation during rapid loss of weight. Dig Dis Sci. 1992;37:912–8.
Tsirline VB, Keilani ZM, Djouzi S, et al. How frequently and when do patients undergo cholecystectomy after bariatric surgery? Surg Obes Rel Dis. 2014;10:313–21.
Uy MC, Talingdan-Te MC, Espinosa WZ, Daez MLO, Ong JP. Ursodeoxycholic acid in the prevention of gallstone formation after bariatric surgery: a meta-analysis. Obes Surg. 2008;18:1532–8.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the preparation of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare there are no conflicts of interest, financial or otherwise, related to the material presented here.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alimoğulları, M., Buluş, H. Predictive factors of gallstone formation after sleeve gastrectomy: a multivariate analysis of risk factors. Surg Today 50, 1002–1007 (2020). https://doi.org/10.1007/s00595-020-01971-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-020-01971-2