Abstract
Background
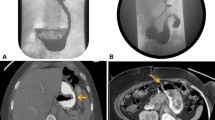
Gastric stenosis (GS) is a potential adverse event post-laparoscopic sleeve gastrectomy (LSG). Endoscopic management is preferred; however, there is significant variation in therapeutic strategies with no defined algorithm. This study aims to describe the safety and efficacy of a predefined step-wise algorithm for endoscopic management of GS post-LSG.
Methods
Consecutive patients with symptomatic GS post-LSG, presenting between July 2015 and August 2016, were subjected to a predefined treatment algorithm of serial dilations using achalasia balloons, followed by a fully covered self-expanding metal stent (FCSEMS) if dilations were inadequate. Patients who did not respond or opted out of ongoing endoscopic therapy were offered revision Roux-en-Y gastric bypass (RYGB).
Results
Total of 17 patients underwent a median of 2 (range 1–4) balloon dilations. Twelve patients (70.6%) reported clinical improvement with balloon dilation alone, while 3 (17.6%) required subsequent FCSEMS placement. One patient suffered a tear to the muscularis propria with balloon dilation, which was managed conservatively. Overall, 15 (88.2%) reported clinical improvement with endoscopic management. PAGI-SYM scores revealed that the strongest response to therapy, based on mean reduction of score ± SD, was in the following items: nausea (3 ± 1.9, P < 0.001), heartburn during day (2.8 ± 1.5, P = 0.003), heartburn on lying down (3.4 ± 1.4, P < 0.001), reflux during day (2.8 ± 1.9, P < 0.001), and reflux on lying down (3.0 ± 1.9, P < 0.001). Two (11.8%) patients failed endoscopic therapy and underwent RYGB.
Conclusions
Endoscopic management of GS using the described algorithmic approach is safe and effective post-LSG. Patients with severe stenosis or helical stenosis are likely to require revision RYGB.





Similar content being viewed by others
References
Silecchia G, Boru C, Pecchia A, et al. Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients. Obes Surg. 2006;16(9):1138–44.
Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366(17):1567–76.
Moszkowicz D, Arienzo R, Khettab I, et al. Sleeve gastrectomy severe complications: is it always a reasonable surgical option? Obes Surg. 2013;23(5):676–86.
Parikh A, Alley JB, Peterson RM, et al. Management options for symptomatic stenosis after laparoscopic vertical sleeve gastrectomy in the morbidly obese. Surg Endosc. 2012;26(3):738–46.
Rebibo L, Hakim S, Dhahri A, et al. Gastric stenosis after laparoscopic sleeve gastrectomy: diagnosis and management. Obes Surg. 2016;26(5):995–1001.
Dapri G, Cadière GB, Himpens J. Laparoscopic seromyotomy for long stenosis after sleeve gastrectomy with or without duodenal switch. Obes Surg. 2009;19(4):495–9.
Burgos AM, Csendes A, Braghetto I. Gastric stenosis after laparoscopic sleeve gastrectomy in morbidly obese patients. Obes Surg. 2013;23(9):1481–6.
Eubanks S, Edwards CA, Fearing NM, et al. Use of endoscopic stents to treat anastomotic complications after bariatric surgery. J Am Coll Surg. 2008;206(5):935–8. discussion 938–9
Ogra R, Kini GP. Evolving endoscopic management options for symptomatic stenosis post-laparoscopic sleeve gastrectomy for morbid obesity: experience at a large bariatric surgery unit in New Zealand. Obes Surg. 2015;25(2):242–8.
Bellorin O, Lieb J, Szomstein S, et al. Laparoscopic conversion of sleeve gastrectomy to Roux-en-Y gastric bypass for acute gastric outlet obstruction after laparoscopic sleeve gastrectomy for morbid obesity. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2010;6(5):566–8.
Lacy A, Ibarzabal A, Obarzabal A, et al. Revisional surgery after sleeve gastrectomy. Surg Laparosc Endosc Percutan Tech. 2010;20(5):351–6.
Chouillard EK, Karaa A, Elkhoury M, et al. Intercontinental Society of Natural Orifice, endoscopic, and laparoscopic surgery (i-NOELS). Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for morbid obesity: case-control study. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2011;7(4):500–5.
Khashab MA, Besharati S, Ngamruengphong S, et al. Refractory gastroparesis can be successfully managed with endoscopic transpyloric stent placement and fixation (with video). Gastrointest Endosc. 2015;82(6):1106–9.
Rentz AM, Kahrilas P, Stanghellini V, et al. Development and psychometric evaluation of the patient assessment of upper gastrointestinal symptom severity index (PAGI-SYM) in patients with upper gastrointestinal disorders. Qual Life Res Int J Qual Life Asp Treat Care Rehabil. 2004;13(10):1737–49.
Revicki DA, Rentz AM, Tack J, et al. Responsiveness and interpretation of a symptom severity index specific to upper gastrointestinal disorders. Clin Gastroenterol Hepatol. 2004;2(9):769–77.
Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71(3):446–54.
Estimate of Bariatric Surgery Numbers, 2011-2015 [Internet]. American Society for Metabolic and Bariatric Surgery. [cited 2016]. Available from: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers
Srinivasa S, Hill LS, Sammour T, et al. Early and mid-term outcomes of single-stage laparoscopic sleeve gastrectomy. Obes Surg. 2010;20(11):1484–90.
Zundel N, Hernandez JD, Galvao Neto M, et al. Strictures after laparoscopic sleeve gastrectomy. Surg Laparosc Endosc Percutan Tech. 2010;20(3):154–8.
Baretta G, Campos J, Correia S, et al. Bariatric postoperative fistula: a life-saving endoscopic procedure. Surg Endosc. 2015;29(7):1714–20.
Werquin C, Caudron J, Mezghani J, et al. Early imaging features after sleeve gastrectomy. J Radiol. 2008;89(11 Pt 1):1721–8.
Keidar A, Appelbaum L, Schweiger C, et al. Dilated upper sleeve can be associated with severe postoperative gastroesophageal dysmotility and reflux. Obes Surg. 2010;20(2):140–7.
Musella M, Milone M, Bellini M, et al. Laparoscopic sleeve gastrectomy. Do we need to oversew the staple line? Ann Ital Chir. 2011;82(4):273–7.
Paluszkiewicz R, Kalinowski P, Wróblewski T, et al. Prospective randomized clinical trial of laparoscopic sleeve gastrectomy versus open Roux-en-Y gastric bypass for the management of patients with morbid obesity. Wideochirurgia Inne Tech Maloinwazyjne Videosurgery Miniinvasive Tech. 2012;7(4):225–32.
Binda A, Jaworski P, Tarnowski W. Stenosis after sleeve gastrectomy--cause, diagnosis and management strategy. Pol Przegl Chir. 2013;85(12):730–6.
Shnell M, Fishman S, Eldar S, et al. Balloon dilatation for symptomatic gastric sleeve stricture. Gastrointest Endosc. 2014;79(3):521–4.
Jones M, Healey AJ, Efthimiou E. Early use of self-expanding metallic stents to relieve sleeve gastrectomy stenosis after intragastric balloon removal. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2011;7(5):e16–7.
Willingham FF, Buscaglia JM. Endoscopic Management of Gastrointestinal Leaks and Fistulae. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2015;13(10):1714–21.
Kumar N, Thompson CC. Endoscopic therapy for postoperative leaks and fistulae. Gastrointest Endosc Clin N Am. 2013;23(1):123–36.
Vilallonga R, Himpens J, van de Vrande S. Laparoscopic management of persistent strictures after laparoscopic sleeve gastrectomy. Obes Surg. 2013;23(10):1655–61.
Rosenthal RJ, International Sleeve Gastrectomy Expert Panel, Diaz AA, et al. International sleeve gastrectomy expert panel consensus statement: best practice guidelines based on experience of >12, 000 cases. Surg Obes Relat Dis Off J Am Soc Bariatr Surg. 2012;8(1):8–19.
Author information
Authors and Affiliations
Contributions
The authors were involved in the writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Manoel Galvao Neto is a consultant for Apollo Endosurgery, consultant and SAB member of GI Dynamics, consultant and SAB member of Fractyl Labs, consultant of GI Windows, consultant and SAB member of Ethicon EndoSurgery.
Mouen A Khashab is a consultant for Boston Scientific and Olympus America.
Vivek Kumbhari is a consultant for Boston Scientific and Apollo Endosurgery.
All other authors have no conflicts of interest to declare.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Funding Sources or Institutional or Corporate Affiliations
None
Electronic supplementary material
Initial endoscope being advanced through the gastro-esophageal junction with healed staple line visible to the left leading to the site of stenosis (0:10). Endoscope passed through stenotic segment and into the fourth part of duodenum. Savary Guidewire (Cook Medical, Boomington, Indiana) being introduced through the scope into the fourth part of the duodenum (0:30). Inspecting the deflated achalasia balloon (0:50). Achalasia balloon (Rigiflex™ II Single-Use Achalasia Balloon Dilators, Boston Scientific, Natick, MA, USA) being inserted over the wire, situated with the middle of the balloon across the stenotic segment (1:06). Balloon inflated to 20 psi pneumatic pressure which is maintained for 1 min. There is visible relative tissue ischemia at the site of the stenosis (1:24). Balloon deflated and withdrawn followed by re-inspection of stenosis segment (2:00). (MP4 232,436 kb)
Rights and permissions
About this article
Cite this article
Agnihotri, A., Barola, S., Hill, C. et al. An Algorithmic Approach to the Management of Gastric Stenosis Following Laparoscopic Sleeve Gastrectomy. OBES SURG 27, 2628–2636 (2017). https://doi.org/10.1007/s11695-017-2689-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2689-3