Abstract
Background
Biliopancreatic diversion (BPD) is a bariatric technique burdened, in some instances, by clinical evidence of malabsorption and malnutrition, and by intractable diarrhea.
Objective
The objective of this study was to assess metabolic and nutritional effects on patients undergoing BPD and BPD plus revisional surgery because of side effects.
Methods
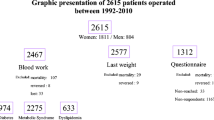
Thirty-five consecutive BPD patients underwent revisional surgery (elongation of the common limb from 50 to 200 cm and reduction of the gastric pouch from 500 to 40 ml) after a median 48-month period [48.3 ± 9.17 months (mean ± SD)] and were observed for a total period of 116.2 ± 6.21 months; 88 patients only undergoing BPD (controls) were observed for 120 months.
Results
Revisional surgery significantly improved side effects of BPD, with resolution of clinical symptoms in most instances. After revisional surgery, patients had a further decrease of body weight. The effect on disappearance of diabetes mellitus (DM) was remarkable, with no difference between revisional surgery and BPD. Triglycerides and transaminases decreased in a similar way, while cholesterol levels differed significantly. Estimated glomerular filtration rate improved. Nutritional parameters were similarly affected.
Conclusion
This study suggests that it is possible to maintain the clinical and metabolic effects of BPD after a revisional procedure that leads to lesser malabsorption and to a greater restriction of the stomach. In particular, the positive effects on DM still persist after revisional surgery. This approach should be kept in mind in the presence of significant side effects due, inter alia, to excessive malabsorption.



Similar content being viewed by others
References
Alvarez-Cordero R. Treatment of clinically severe obesity—a public health problem: introduction. World J Surg. 1998;22:905–6.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–56.
Keshishian A, Zahriya K, Willes EB. Duodenal switch has no detrimental effects on hepatic function and improves hepatic steatohepatitis after 6 months. Obes Surg. 2005;15:1418–23.
Alexandrides TK, Skroubis G, Kalfarentzos F. Resolution of diabetes mellitus and metabolic syndrome following Roux-en-Y gastric bypass and a variant of biliopancreatic diversion in patients with morbid obesity. Obes Surg. 2007;17:176–84.
Aller R, Pacheco D, Izaola O, et al. Effect on liver enzymes of biliopancreatic diversion: 4 years of follow-up. Ann Nutr Metab. 2015;66:132–6.
Dixon JB, Bhathal PS, O'Brien PE. Weight loss and non-alcoholic fatty liver disease: falls in gamma-glutamyl transferase concentrations are associated with histologic improvement. Obes Surg. 2006;16:1278–86.
Gastaldelli A, Perego L, Paganelli M, et al. Elevated concentrations of liver enzymes and ferritin identify a new phenotype of insulin resistance: effect of weight loss after gastric banding. Obes Surg. 2009;19:80–6.
Weiner RA. Surgical treatment of non-alcoholic steatohepatitis and non-alcoholic fatty liver disease. Dig Dis. 2010;28:274–9.
Hafeez S, Ahmed MH. Bariatric surgery as potential treatment for nonalcoholic fatty liver disease: a future treatment by choice or by chance? J Obes. 2013;2013:839275.
Burza MA, Romeo S, Kotronen A, et al. Long-term effect of bariatric surgery on liver enzymes in the Swedish Obese Subjects (SOS) study. PLoS One. 2013;8(3):e60495.
Folini L, Veronelli A, Benetti A, et al. Liver steatosis (LS) evaluated through chemical-shift magnetic resonance imaging liver enzymes in morbid obesity; effect of weight loss obtained with intragastric balloon gastric banding. Acta Diabetol. 2014;51:361–8.
Hassanian M, Al-Mulhim A, Al-Sabhan A, et al. The effect of bariatric surgeries on nonalcoholic fatty liver disease. Saudi J Gastroenterol. 2014;20:270–8.
Scopinaro N. Biliopancreatic diversion: mechanisms of action and long-term results. Obes Surg. 2006;16:683–9.
Scopinaro N, Adami GF, Marinari GM, et al. Biliopancreatic diversion. World J Surg. 1998;22:936–46.
Ceriani V, Pinna F, Lodi T, Gaffuri P. Revisional surgery: biliopancreatic diversion failure. In: M. Lucchese, N. Scopinaro (eds): Bariatric and Metabolic Mini-Invasive Surgery. Principles and Technical Aspects, Springer, 2015, pp 257–266.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes?. Diabetes Care. 2009;32:2133–5.
Levey AS, Coresh J, Greene T, et al. Chronic kidney disease epidemiology C. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–54.
Hakeam HA, O'Regan PJ, Salem AM, et al. Impact of laparoscopic sleeve gastrectomy on iron indices: 1 year follow-up. Obes Surg. 2009;19:1491–6.
Varma S, Baz W, Badine E, et al. Need for parenteral iron therapy after bariatric surgery. Surg Obes Relat Dis. 2008;4:715–9.
Obinwanne KM, Fredrickson KA, Mathiason MA, et al. Incidence, treatment, and outcomes of iron deficiency after laparoscopic Roux-en-Y gastric bypass: a 10-year analysis. J Am Coll Surg. 2014;218:246–52.
Ferrer R, Pardina E, Rossell J, et al. Haematological parameters and serum trace elements in “healthy” and “unhealthy” morbidly obese patients before and after gastric bypass. Clin Nutr. 2015;34:276–83.
Schuster DP, Teodorescu M, Mikami D, et al. Effect of bariatric surgery on normal and abnormal renal function. Surg Obes Relat Dis. 2011;7:459–64.
Agrawal V, Krause KR, Chengelis DL, et al. Relation between degree of weight loss after bariatric surgery and reduction in albuminuria and C-reactive protein. Surg Obes Relat Dis. 2009;5:20–6.
Iaconelli A, Panunzi S, De Gaetano A, et al. Effects of bilio-pancreatic diversion on diabetic complications: a 10-year follow-up. Diabetes Care. 2011;34:561–7.
Jose B, Ford S, Super P, et al. The effect of biliopancreatic diversion surgery on renal function—a retrospective study. Obes Surg. 2013;23:634–7.
Ruiz-Tovar J, Giner L, Sarro-Sobrin F, et al. Laparoscopic sleeve gastrectomy prevents the deterioration of renal function in morbidly obese patients over 40 years. Obes Surg. 2015;25:796–9.
Ballesteros-Pomar MD, González de Francisco T, Urioste-Fondo A, et al. Biliopancreatic diversion for severe obesity: long-term effectiveness and nutritional complications. Obes Surg. 2016;26:38–44.
Marceau P, Biron S, Marceau S, et al. Long-term metabolic outcomes 5 to 20 years after biliopancreatic diversion. Obes Surg. 2015;25:1584–93.
Thurnheer M, Bisang P, Ernst B, et al. A novel distal very long Roux-en Y gastric bypass (DVLRYGB) as a primary bariatric procedure—complication rates, weight loss, and nutritional/ metabolic changes in the first 355 patients. Obes Surg. 2012;22:1427–36.
Svanevik M, Risstad H, Hofsø D, et al. Perioperative outcomes of proximal and distal gastric bypass in patients with BMI ranged 50-60 kg/m2. A double-blind, randomized controlled trial. Obes Surg. 2015;25:1788–95.
Sugerman HJ, Kellum JM, DeMaria EJ. Conversion of proximal to distal gastric bypass for failed gastric bypass for superobesity. J Gastrointest Surg. 1997;1:517–24.
Brolin RE, LaMarca LB, Kenler HA, et al. Malabsorptive gastric bypass in patients with super-obesity. J Gastrointest Surg. 2002;6:195–203.
Ceriani V, Cetta F, Pinna F, et al. Abnormal calcium, 25(OH)vitamin D, and parathyroid hormone after biliopancreatic diversion; correction through elongation of the common tract and reduction of the gastric pouch. Surgery for Obesity and Related Diseases, Surg Obes Relat Dis. 2016;12:805–12.
Busetto L, Sbraccia P, Frittitta L, et al. The growing role of bariatric surgery in the management of type 2 diabetes: evidences and open questions. Obes Surg. 2011;21:1451–7.
Salehi M, D'Alessio DA. Effects of glucagon like peptide-1 to mediate glycemic effects of weight loss surgery. Rev Endocr Metab Disord. 2014;15:171–9.
Frige' F, Laneri M, Veronelli A, et al. Bariatric surgery in obesity: changes of glucose and lipid metabolism correlate with changes of fat mass. Nutr Metab Cardiovasc Dis. 2009;19:198–204.
Pontiroli AE, Laneri M, Veronelli A, et al. Biliary pancreatic diversion and laparoscopic adjustable gastric banding in morbid obesity: their long-term effects on metabolic syndrome and on cardiovascular parameters. Cardiovasc Diabetol. 2009;8:37.
Benetti A, Del Puppo M, Crosignani A, et al. Cholesterol metabolism after bariatric surgery in grade 3 obesity: differences between malabsorptive and restrictive procedures. Diabetes Care. 2013;36:1443–7.
Currò G, Centorrino T, Cogliandolo A, et al. A clinical and nutritional comparison of biliopancreatic diversion performed with different common and alimentary channel lengths. Obes Surg. 2015;25:45–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest. Informed consent was obtained from all individual participants included in the study. There was no funding for this study. The paper is not based on a previous communication to a society or meeting.
Rights and permissions
About this article
Cite this article
Ceriani, V., Cetta, F., Lodi, T. et al. Clinical and Metabolic Effects of Biliopancreatic Diversion Persist After Reduction of the Gastric Pouch and Elongation of the Common Alimentary Tract. Preliminary Report in a Series of Patients with a 10-Year Follow-Up. OBES SURG 27, 1493–1500 (2017). https://doi.org/10.1007/s11695-016-2479-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2479-3