Abstract
Background
Well-documented clinical data registers are valuable for assessing the effectiveness of surgical interventions.
Objective
The aim of this study was to present our initial experience with the implementation of a local register documenting patients with arthroscopic rotator cuff tear reconstruction (ARCR).
Materials and methods
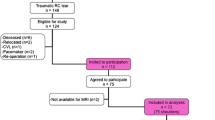
Standardized documentation of demographic, baseline, and surgery characteristics of ARCR patients was initiated in February 2010. Patient follow-up at 6 months postsurgery began in June 2014 using various objective and subjective patient-reported outcomes (PROs) including the Constant–Murley Score (CS), Oxford Shoulder Score (OSS) and Subjective Shoulder Value (SSV). An additional 2- to 4-year postoperative evaluation of PROs and level of satisfaction was made by postal questionnaire. The proportion of cases documented in the register and the initial patient outcomes were examined.
Results
The overall documentation rate of ARCR patients was 59 % (1,092/1,860) with 11 of 19 surgeons achieving 76 % altogether. Ninety-eight percent (45/46) of patients were documented at 6 months; the mean CS, OSS, and SSV improved significantly by 17.0 points, 11.4 points, and 35.6 %, respectively (p < 0.001). There were 58 % (174/301) postal questionnaire respondents showing similar improvements in OSS and SSV, with 91 % of patients rating 8 points or more on a 0–10 satisfaction scale.
Conclusion
The implementation of an ARCR clinical register is achievable by motivated surgeons with adequate support for data collection and control. Long-term postsurgery PROs show treatment effectiveness associated with high patient satisfaction.
Zusammenfassung
Hintergrund
Gut dokumentierte klinische Datenregister sind wertvoll, um die Wirksamkeit chirurgischer Eingriffe zu evaluieren.
Ziel der Studie
Präsentation unserer Erfahrung mit der Entwicklung eines lokalen Registers zur Dokumentation von Patienten mit arthroskopischer Rekonstruktion der Rotatorenmanschette (ARCR).
Material und Methoden
Seit Februar 2010 wurden bei allen ARCR-Patienten die präoperativen Baseline-Daten sowie die operativen Details systematisch erfasst. Im Juni 2014 wurden zusätzlich objektive und subjektive Ergebnismessungen 6 Monate postoperativ eingeführt (Constant-Score, CS; Oxford Shoulder Score, OSS; Subjective Shoulder Value, SSV). Eine postalische Befragung der Patienten erfolgte zudem 2–4 Jahre postoperativ. Die Vollständigkeit der im Register erfassten Fälle sowie erste funktionelle Ergebnisse der Patienten und deren Zufriedenheit wurden untersucht.
Ergebnisse
Die Gesamtdokumentationsrate der ARCR-Patienten lag bei 59 % (1092/1860), wobei 11 von 19 beteiligten Chirurgen zusammen eine Rate von 76 % erreichten. Bei den 6-Monats-Kontrollen wurden 98 % (45/46) der Fälle dokumentiert. Der mittlere CS, OSS und SSV verbesserten sich signifikant um 17,0 bzw. 11,4 Punkte und 35.6 % (p < 0,001). Die 58 % Rückmeldungen (174/301) der postalischen Befragung zeigten ähnliche Verbesserungen im OSS und SSV, mit 91 % der Patienten, die 8 oder mehr Punkte auf der Zufriedenheitsskala (0–10) angekreuzt hatten.
Schlussfolgerung
Die Einführung eines klinischen Registers für ARCR kann mit motivierten Chirurgen und entsprechender Unterstützung bei Datenerfassung und -management erreicht werden. Langzeitbefragungen zeigen den Behandlungserfolg und die damit verbundene Patientenzufriedenheit.




Similar content being viewed by others
References
Allom R, Colegate-Stone T, Gee M et al (2009) Outcome analysis of surgery for disorders of the rotator cuff: a comparison of subjective and objective scoring tools. J Bone Joint Surg Br 91:367–373
Arce G, Bak K, Bain G et al (2013) Management of disorders of the rotator cuff: proceedings of the ISAKOS upper extremity committee consensus meeting. Arthroscopy 29:1840–1850
Black N (1996) Why we need observational studies to evaluate the effectiveness of health care. BMJ 312:1215–1218
Carr AJ, Rees JL, Ramsay CR et al (2014) Protocol for the United Kingdom Rotator Cuff Study (UKUFF): a randomised controlled trial of open and arthroscopic rotator cuff repair. Bone Joint Res 3:155–160
Chung SW, Oh JH, Gong HS et al (2011) Factors affecting rotator cuff healing after arthroscopic repair: osteoporosis as one of the independent risk factors. Am J Sports Med 39:2099–2107
Constant CR, Gerber C, Emery RJ et al (2008) A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg 17:355–361
Dawson J, Fitzpatrick R, Carr A (1996) Questionnaire on the perceptions of patients about shoulder surgery. J Bone Joint Surg Br 78:593–600
Dawson J, Rogers K, Fitzpatrick R et al (2009) The Oxford shoulder score revisited. Arch Orthop Trauma Surg 129:119–123
Fuchs B, Weishaupt D, Zanetti M et al (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 8:599–605
Gilbart MK, Gerber C (2007) Comparison of the subjective shoulder value and the Constant score. J Shoulder Elbow Surg 16:717–721
Guttzwiller F, Biller-Andorno N, Harnacke C et al (2012) Methoden zur Bestimmung von Nutzen bzw. Wert medizinischer Leistungen und deren Anwendung in der Schweiz und ausgewählten europäischen Ländern. Akademien der Wissenschaften Schweiz, Basel, p 111
Harris PA, Taylor R, Thielke R et al (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Herdman M, Gudex C, Lloyd A et al (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20:1727–1736
Ho WP, Huang CH, Chiu CC et al (2013) One-stage arthroscopic repair of rotator cuff tears with shoulder stiffness. Arthroscopy 29:1283–1291
Huber W, Hofstaetter JG, Hanslik-Schnabel B et al (2004) The German version of the Oxford Shoulder Score—cross-cultural adaptation and validation. Arch Orthop Trauma Surg 124:531–536
Imhoff A, Ticker J, Fu F (2003) An atlas of shoulder arthroscopy. Informa Healthcare, London
Jung C, Buchmann S, Flury M (2012) Die arthroskopische Rotatorenmanschetten- Rekonstruktion—Von der Aussnahme zum Standard. Swiss J Med Med Technol (Swiss Med) 34:35–39
Karas V, Hussey K, Romeo AR et al (2013) Comparison of subjective and objective outcomes after rotator cuff repair. Arthroscopy 29:1755–1761
Katolik LI, Romeo AA, Cole BJ et al (2005) Normalization of the Constant score. J Shoulder Elbow Surg 14:279–285
Kolling C, Simmen BR, Labek G et al (2007) Key factors for a successful National Arthroplasty Register. J Bone Joint Surg Br 89:1567–1573
Le B, Wu X, Murrell G (2012) Factors predicting rotator cuff re-tear rate: an analysis of 1000 consecutive rotator cuff repairs. J Sci Med Sport 15:S337
Lin EC, Mall NA, Dhawan A et al (2013) Arthroscopic primary rotator cuff repairs in patients aged younger than 45 years. Arthroscopy 29:811–817
Lindley K, Jones GL (2010) Outcomes of arthroscopic versus open rotator cuff repair: a systematic review of the literature. Am J Orthop (Belle Mead NJ) 39:592–600
Lupo R, Rapisarda S, Palmisciano G et al (2012) Lesions of the rotator cuff. Arthroscopic versus open mini: our experience. J Orthop Traumatol 13:13S31–13S32
Olley LM, Carr AJ (2008) The use of a patient-based questionnaire (the Oxford Shoulder Score) to assess outcome after rotator cuff repair. Ann R Coll Surg Engl 90:326–331
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res 254:81–86
Raftery J, Roderick P, Stevens A (2005) Potential use of routine databases in health technology assessment. Health Technol Assess 9:1–92, iii–iv
Ross S, Grant A, Counsell C et al (1999) Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiology 52:1143–1156
Simmen BR, Angst F, Schwyzer HK et al (2009) A concept for comprehensively measuring health, function and quality of life following orthopaedic interventions of the upper extremity. Arch Orthop Trauma Surg 129:113–118
Acknowledgments
The authors would like to thank D. Rickenbacher for supporting in the preparation of study documents and M. Wilhelmi, PhD, for the preparation and proofreading of this manuscript.
Support for this research was provided by
Schulthess Clinic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Flury is a paid consultant for and receives royalties from Arthrex Inc. C. Kolling, C. Grobet, S. Kunz and L. Audigé state that they have no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Flury, M., Kolling, C., Grobet, C. et al. Implementation of a local outcome register for arthroscopic rotator cuff tear repair. Obere Extremität 10, 33–40 (2015). https://doi.org/10.1007/s11678-014-0299-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11678-014-0299-4