Abstract
Summary
The adoption of the management pathway proposed by the National Osteoporosis Guideline Group (NOGG), UK applied using the Austrian FRAX® tool in a referral population of Austrian women categorises 22–29% of women age 40 years or more eligible for treatment of whom 28–34% are classified at very high risk.
Purpose
The aim of this study is to provide a reference document for the further development of existing guidelines for the management of osteoporosis in Austria, considering FRAX-based intervention thresholds for high and very high fracture risk.
Methods
The model development was based on two Austrian hospital referral cohorts. Baseline information was collected to compute the 10-year probability (using the Austrian FRAX model) of a major osteoporotic fracture (MOF) and hip fracture both with and without the inclusion of femoral neck bone mineral density (BMD). Assessment thresholds for BMD testing were defined, as well as intervention thresholds. In addition, thresholds that characterise men and women at high and very high fracture risk were established. The management pathway followed that currently recommended by the UK National Osteoporosis Guideline Group (NOGG).
Results
The two cohorts comprised a total of 1306 women and men with a mean age of 66.7 years. Slightly more than 50% were eligible for treatment by virtue of a prior fragility fracture. In those women without a prior fracture, 22% (n = 120) were eligible for treatment based on MOF probabilities. Of these, 28% (n = 33) were found to be at very high risk. When both MOF and hip fracture probabilities were used to characterise risk, 164 women without a prior fracture were eligible for treatment (29%). Of these, 34% (n = 56) were found to be at very high risk. Fewer men without prior fracture were eligible for treatment compared with women.
Conclusion
The management pathway as currently outlined is expected to reduce inequalities in patient management. The characterisation of very high risk may aid in the identification of patients suitable for treatment with osteoanabolic agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is defined as a systemic skeletal disease characterised by low bone mass and microarchitectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture [1]. Vertebral fractures, hip fractures and fractures of the proximal humerus and the distal forearm are together considered major osteoporotic fractures (MOF). They have been shown to be associated with an increased risk of subsequent fracture, reduced quality of life, disability and increased mortality [2,3,4]. The average lifetime risk of a 50-year-old woman to sustain an MOF has been estimated at close to 50%, and at 22% in women and men, respectively [5]. In general, osteoporotic fractures can occur also at many other anatomical sites, such as the pelvis, the tibia or the ribs [6].
The Republic of Austria is located in the southern part of Central Europe. In 2022, the population of Austria was 9.1 million, of whom 3.6 million were age 50 years or more [7]. Similar to other countries of the European Union, its age pyramid shows a narrow base and an increasing proportion of older individuals. The current trend of a growing and ageing population is expected to continue in the coming years and hence be accompanied by an increasing burden of osteoporosis and fragility fracture [8].
The epidemiology of fractures in Austria has been investigated extensively in the past decade. The incidence of hip fracture over the past 3 decades (1989–2018) indicated a steep increase in the first 20 years, which thereafter remained fairly stable over the last decade with a slight albeit significant downward trend [9]. Notwithstanding, hip fracture incidence in Austria has been shown to be among the highest worldwide, exceeded only by Sweden and Denmark [10].
Currently, osteoporosis treatment decisions in Austria are mainly based on country specific guidelines that have been authored and updated in 2017 by an expert group on behalf of the Austrian Bone and Mineral Society, the then Association of Austrian Social Insurance Institutions (Hauptverband der österreichischen Sozialversicherungsträger) and other stakeholders of the Austrian health care system [11]. In general, the recommendation is to initiate osteoporosis specific treatment in people age 50 years or more, with a prior fragility fracture, particularly at the hip or spine. In addition, assessment of 10-year fracture probability by using the country specific version of the fracture-risk assessment tool FRAX® is recommended. Similar to some other countries [12], the Austrian guidelines recommend osteoporosis treatment if the FRAX-based 10-year fracture probability is equal to or is above 20% for MOF, or 5% for hip fracture. The use of fixed intervention thresholds instead of age-specific thresholds raises some anomalies. For example, a person below the age of 65 years might not receive adequate osteoporosis treatment if his or her FRAX-based 10-year fracture probability for MOFs was below 20%, but above the probability of a person of the same age with a prevalent fracture.
Moreover, the treatment rates after osteoporotic fractures in Austria has been shown to be very low [13] despite the availability of national osteoporosis guidelines. Indeed, only 2 out of 10 women, and only 1 out of 10 men receive adequate osteoporosis treatment within 4–18 months after a fracture, irrespective of the fact that Austria’s Gross Domestic Product (GDP) per capita is among the top twenty-five countries worldwide [14] and has a generous social security system which ensures that all receive medical service free of charge.
Against this background, the aim of the present study was to provide a reference document that would help advance country specific osteoporosis guidelines for Austria. In this regard, the Austrian Society of Bone and Mineral Research wished to consider the following. First, the FRAX-based Austrian intervention threshold—which currently is more or less arbitrarily set at a fixed level of 20% for MOFs, and 5% for hip fracture, respectively—should be replaced by hybrid thresholds as recently developed by the UK National Osteoporosis Guideline Group (NOGG), whereby a fixed intervention threshold should be used from the age of 70 years, in order to achieve equity between individuals with versus without a prior fracture at this age [15]. Second, the category of a ‘very high fracture risk’ should be implemented into this hybrid model, as developed by the International Osteoporosis Foundation (IOF) and the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) [16], and incorporated into recent NOGG guidance [17].
Methods
The model development was based on two Austrian hospital referral cohorts (Cohorts A and B). Cohort A was recruited within the framework of the PoCOsteo study, a two-centre prospective study in Austria and Iran, which aimed to develop a point-of-care device for measurement of bone proteomic and genomic markers from a finger-prick whole blood sample [18]. The study population used for model development herein comprised the first consecutive 750 patients age 50 years or above (range 50–89 years) who were referred for skeletal assessment to a large tertiary hospital in the southern region of Austria during 2017–2020 (University Hospital of Graz).Cohort B comprised 89 men and 467 women referred for assessment of osteoporosis to a tertiary hospital in Vienna between 2009 and 2010 and followed up for 5 years or more [19]. This cohort was a pre-planned sample of the total referral population of 2789 patients (502 men and 2278 women). The cohort excluded patients with high-trauma fractures, premenopausal women, patients with malignancies or immobile individuals as well as patients who had previously received specific osteoporosis treatment (except calcium and/or vitamin D).
Baseline investigation
Baseline information was collected to enable computation of the 10-year probability of a MOF and hip fracture both with and without the inclusion of femoral neck bone mineral density (BMD) with the use of the Austrian FRAX model. BMD was measured with Lunar iDXA (Cohort A) and Lunar Prodigy (Cohort B), from which a standardised BMD was calculated for input into the FRAX model [20]. T-scores were calculated using the NHANES reference values for young Caucasian women as used in FRAX [21].
For Cohort A, age, sex and data on prior fragility fracture and secondary osteoporosis were available in all men and women. Body mass index (BMI) and BMD were missing in 12 and 34 patients, respectively (1.6% and 4.5%, respectively). With regard to the other dichotomous FRAX variables, information was incomplete for parental history of hip fracture (n missing = 49, 6.5%), exposure to glucocorticoids (n = 4, 0.5%), rheumatoid arthritis (n = 3, 0.4%), current smoking (n = 3, 0.4%) and high alcohol consumption (n = 3, 0.4%). For the purposes of this analysis, these variables were simulated to more closely represent the population from which the sample was drawn. In Cohort B, age, sex and body mass index (BMI) were available in all men and women. BMD was missing in 20 patients (3.6%). With regard to the other dichotomous FRAX variables, information was incomplete for prior fracture (n missing = 107, 19.2%)), parental history of hip fracture (n = 340, 61.2%)), exposure to glucocorticoids (n = 104, 18.7%), rheumatoid arthritis (n = 83, 14.9%), current smoking (n = 180, 32.4%), secondary osteoporosis (n = 105, 18.9%) and high alcohol consumption (n = 181, 32.6%). For the purposes of this analysis, these variables were simulated.
Simulation of risk variables
An analysis was performed where the missing values on clinical risk factors were simulated based on the cohort itself using associations between dichotomous FRAX variables to generate logistic regression equations as described previously [22, 23]. The equations were applied to the data in the present sample to predict the probability of having a positive value for the missing key risk factor for each individual. Next, a random number between 0 and 1 was generated using a computer program, which was then compared with the predicted probability for that variable for that individual. If the random number was less than or equal to the predicted probability, the individual was assigned a positive response for the risk factor. If the random number was larger than the predicted probability, the person was assigned a negative response for the risk factor. The simulations for femoral neck BMD and BMI were based on examining the conditional probability of the association of the risk factors. Probabilities in the cohorts following simulation did not differ from the subsets that had all variables (see Appendix).
Fracture probabilities
The 10-year probabilities of hip fracture and a major osteoporotic fracture (clinical spine, hip, humerus or distal forearm fracture) were calculated using the FRAX model for Austria (web version 4.1). Calculations were undertaken with and without the inclusion of femoral neck BMD.
Intervention thresholds
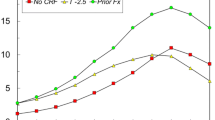
The use of FRAX in clinical practice demands a consideration of the fracture probability at which to intervene, both for treatment (an intervention threshold) and for BMD testing (assessment thresholds). The approach to the setting of intervention and assessment thresholds used the methodology adopted by NOGG for FRAX-based guidelines in the UK [24,25,26]. For men and women, the intervention threshold up to age 70 years is set at a risk equivalent to that of a woman of the same age with a prior fracture and therefore rises with age. At age 70 years and above, fixed thresholds are applied [15]. A threshold that characterises men and women at high and very high fracture risk has also been established; very high risk is identified as a FRAX-based fracture probability that exceeds the intervention threshold by 60% (Fig. 1) [17].
Assessment, intervention and risk thresholds for major osteoporotic fracture probability (MOF) in Austria with the use of FRAX. Individuals with probabilities below the lower assessment threshold (LAT) are considered for lifestyle advice. Those at intermediate risk (probabilities between the upper assessment threshold (UAT) and lower assessment threshold (LAT)) are further assessed with BMD measurement. Where probabilities calculated using BMD lie above or below the intervention threshold (IT), treatment or lifestyle advice, respectively, is recommended. Patients with probabilities above the upper assessment threshold (UAT) are considered for treatment. Those with probabilities above the very high-risk threshold (VHRT) might be considered for osteoanabolic therapy if clinically appropriate. Where BMD measurement is not practical, patients with probabilities above the IT are considered for treatment
Numerical values for thresholds are given in Table 1.
Assessment thresholds
Two assessment thresholds for making recommendations for the measurement of BMD were considered [24, 25]:
-
a)
A threshold probability below which neither treatment nor a BMD test should be considered (lower assessment threshold, LAT).
-
b)
A threshold probability above which treatment may be recommended irrespective of BMD (upper assessment threshold, UAT).
The LAT was set to exclude a requirement for BMD testing in men and women without clinical risk factors, as given in current European guidelines [27,28,29]. It was therefore set to the age-specific 10-year probability of a major fracture equivalent to women with no clinical risk factors. The UAT was chosen to minimise the probability that a patient, characterised to be at high risk using clinical risk factors alone, would be reclassified to be at low risk with additional information on BMD and vice versa [30]. The upper assessment threshold was set at 1.2 times the intervention threshold as used in the UK (see Table 1) [25].
Management pathway
The management pathway followed that currently recommended by NOGG [31]. Under the NOGG strategy, the risk of fracture is first assessed on clinical risk factors alone which in turn provides guidance whether a femoral neck BMD measurement or treatment is indicated, an approach that has been endorsed by the UK National Institute for Health and Care Excellence [32]. An exception is in the presence of a prior fragility fracture, in which case treatment is to be considered in such patients without necessarily undertaking a BMD measurement. For the present report, we assumed that treatment would be considered in all men and women with prior fracture. In those with clinical risk factors (but no prior fracture), the decision is based on the 10-year probability of major osteoporotic fracture with some individuals deemed at high risk or very high risk (treatment without BMD), some at or near the intervention threshold (intermediate risk; BMD indicated to finalise risk evaluation and stratification) and some at low risk (lifestyle advice, reassurance and re-evaluation in the future). Once BMD is entered into the calculation, the decision to treat or not is based on a comparison to age-specific thresholds for major osteoporotic fracture probability; a probability at or above the intervention threshold indicates eligibility for treatment.
The NOGG guidance also recommends, when BMD is included in a FRAX assessment, that hip fracture probability can be additionally taken into account and that high risk and very high risk be predicated the higher of the two (MOF and hip fracture) risk assessments. The impact of this additional assessment was also explored.
Prior assessment strategy
The previous Austrian guideline recommends osteoporosis specific treatment in individuals age 50 years or more, with a prior fragility fracture. In addition, it recommends osteoporosis treatment if the FRAX-based 10-year fracture probability is ≥ 20% for MOF, or ≥ 5% for hip fracture. Since patients with a prior fracture would be treated by either approach, we compared risk categorisation of the previous guideline (prior assessment strategy) with that investigated in the present study based on the 10-year probability of MOF with BMD included (NOGG assessment strategy). Concordance was assessed using Cohen’s kappa.
Sensitivity analysis
The Austrian Bone and Mineral Society have raised the view that in Austria no patient should be assessed for 10-year fracture probability without also measuring BMD. In this scenario, there would be no need for an ‘intermediate’ risk based on which BMD could be performed in order to stratify patients to either above or below the lower intervention threshold. The impact of this on the management pathway was explored as a sensitivity analysis.
Results
The baseline characteristics are given in Table 2. The prevalence of the clinical risk factors was high as would be expected from referral populations. Fracture probabilities rose with age (Fig. 2). For both MOF and hip fracture probabilities, the inclusion of BMD in the calculation was associated with a decrease in fracture probability in men and women age 60 or more years. The effect was particularly marked for hip fracture probability.
Management pathway
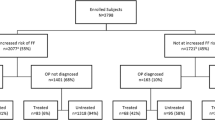
A prior fragility fracture was recorded in 562 of 1116 women (50.4%) and 102 of 190 men (53.7%), and these patients would be eligible for treatment on this basis. For those without a prior fracture (554 women and 88 men), the assessment of fracture probability and the categorisation of fracture risk is undertaken on the basis of age, sex, BMI and the clinical risk factors. In women, 69 (6.2%) would be eligible for treatment in that their fracture probability for MOF exceeded the intervention threshold for Austria (Fig. 3). Of these, 26 (2.3%) were categorised at very high risk. At the other extreme, 86 women were categorised as low risk individuals (7.7%) and would not normally be eligible for further assessment in that their fracture probability lay below the lower assessment threshold. The intermediate category of risk in Fig. 3 comprised 399 women (35.8%) in whom FRAX would be recalculated with the inclusion of femoral neck BMD. Of these, 348 women were categorised at low risk (31.2%) and 44 women at high risk (3.9%) and 7 women at very high risk (0.6%). In brief, of 554 women with no prior fracture, 22% (n = 120) were eligible for treatment. Of these, 28% (n = 33) were found to be at very high risk.
Where eligibility for treatment was based on hip fracture probabilities (in addition to MOF probabilities), 164 women without a prior fracture were eligible for treatment. Of these, 38% (n = 3) were found to be at very high risk.
In men with no prior fracture, the initial assessment (FRAX without BMD) categorised 34% at low risk and 13% at intermediate risk. Of those at intermediate risk, all but two male patients (1%) fell into the low-risk category when assessed using MOF probabilities. Where eligibility for treatment was based on hip fracture probabilities (in addition to MOF probabilities), 8 men without a prior fracture were eligible for treatment. Of these, 34% (n = 56) were found to be at very high risk.
The overall disposition of the cohort is summarised in Table 3.
Prior fracture
A total of 102 men and 562 women had a history of a prior fracture and would thus be eligible for treatment without necessarily having a BMD test. If a BMD were to be undertaken and the probability of a MOF calculated, then 12 men and 117 women (12% and 21% of men and women with a prior fracture, respectively) would be categorised at very high risk. If hip fracture probability were additionally evaluated, then 27 men and 215 women would be categorised at very high risk (26% of men and 38% of women with a prior fracture).
Sensitivity analysis
The impact of undertaking BMD measurements in all patients alongside FRAX is summarised in Table 4 for individuals without a prior fracture. In the case of women, 458 of 554 (83%) would be characterised at low risk, 76 (14%) at high risk and 20 (4%) at very high risk. These data can be compared with the classic NOGG strategy summarised in Fig. 3 and Table 3. Of 554 women with no prior fracture, the number in the low risk category decreased by 24 with the universal use of BMD. Conversely, the number of high risk women increased by 11 and very high risk women by 13. As expected, if hip fracture probability were additionally evaluated, then an additional 6 men and 4 women would be categorised at high risk and an additional 7 men and 7 women would be categorised at very high risk.
When both MOF and hip fracture probability were used to characterise risk the ‘BMD in all’ strategy identified 9.1% of men at high risk and 8.0% at very high risk. With the NOGG strategy, the respective proportions were lower (5.7% and 3.4%, respectively). In women, the ‘BMD in all’ strategy identified 16.4% at high risk and 11.0% at very high risk. With the NOGG strategy, the respective proportions were lower (19.5% and 10.1%, respectively).
A principal difference in the two strategies lies in the requirement for BMD testing. Testing all patients (without prior fragility fracture) with a BMD measurement and using MOF intervention thresholds require 6.4 scans to identify one patient for treatment, whereas the NOGG strategy requires 3.5 scans to identify one patient for treatment.
The impact of testing BMD in all patients (with or without a prior fracture) is given in Table 5. The number of individuals identified at high or very high risk varied according to the criteria used to characterise high and very high risk. When assessed from the 10-year probability of MOF, 15.8% of men and 26.5% of women were at high risk and 6.3% and 22.9%, respectively, at very high risk (Table 5). The proportion of individuals characterised at very high risk increased to 13.7 and 28.1% in men and women, respectively, when additionally based on hip fracture probability.
Comparison with prior assessment strategy
In those without a fragility fracture, the number of individuals eligible for treatment identified using the NOGG approach was fewer than that using the prior assessment strategy. For example, using the NOGG approach based on MOF probability, 19.0% of the cohort were identified for treatment, whereas 25.4% were identified by the prior Austrian guidance. As would be expected, there were differences in the individuals identified using the two assessment algorithms. Cohen’s Kappa was 0.574 signifying only moderate concordance in the categorisation of patients. The distribution of concordant and discordant classification is shown in Table 6. As would be expected, 10-year MOF probabilities were high in the 95 individuals characterised as eligible for treatment using both algorithms (24.3%), low in 452 individuals characterised at low risk by both algorithms (7.7%) and intermediate where characterisation was discordant (14.6 an 16.5%). The major difference between the two approaches was in the age of those identified at high risk. With the prior guideline approach, the mean age of those eligible for treatment was 73.9 years, whereas with the NOGG strategy in the present study included more younger individuals (mean age 68.9 years).
Discussion
The aim of the present study was to provide a reference document that would help advance existing country specific osteoporosis guidelines for Austria, considering a management pathway following that currently recommended by the National Osteoporosis Guideline Group (UK). In particular, the Austrian Bone and Mineral Society defined three aspects that should be integrated into the existing guidelines. First, the currently more or less arbitrarily fixed intervention threshold based on FRAX probabilities should be replaced by age-specific thresholds up to the age of 70 years. Second, a fixed intervention threshold should be used from the age of seventy. And third, the category of a ‘very high risk’, as recommended recently by the IOF and the ESCEO, should be implemented into this hybrid model.
The categorisation of risk is widely accepted within medicine as an appropriate mechanism to direct decisions on treatment; examples include the fields of cardiovascular disease, hypertension and diabetes [33,34,35].The further sub-categorisation of those meriting treatment into high risk and very high risk is predicated on the same principle as it aids in choosing the type of treatment to be recommended. The increasing availability of anabolic therapies in osteoporosis and their superiority to anti-resorptive treatments in head-to-head randomised clinical trials has influenced discussions about the setting of threshold values [36,37,38,39]. Such considerations justify the need for dichotomy but are less helpful in its operationalisation, which by nature will always be somewhat arbitrary. With regard to the development of thresholds between high and very high fracture risk NOGG, ESCEO and the IOF identify approximately 10% at very high risk with a risk threshold consistent with patients included in phase 3 studies of anabolic agents considered precedent and appropriate [16, 17].
The present study examines the impact of categorising fracture risk in two referral cohorts using the methodology developed by NOGG but applied to the Austrian FRAX model. Fracture probabilities were higher than those which would be expected in the general population because of the high frequency of clinical risk factors consistent with a referral population. It is of interest that for both MOF and hip fracture probabilities the inclusion of BMD in the FRAX calculation was associated with a decrease in fracture probability at older ages. This suggests a referral bias towards excluding individuals with low BMD, perhaps because of immobility, institutionalized residence or multiple comorbidities.
The increase in the numbers in the very high risk category when both the MOF and hip fracture thresholds are used needs consideration in guideline development. A further option examined was to undertake BMD testing in all patients, rather than in those in the ‘intermediate’ category of risk. This increased modestly the proportion of individuals detected at very high risk using the MOF intervention thresholds but had a more marked effect when hip fracture and MOF thresholds were applied. As noted in the results, testing all patients (without prior fragility fracture) with a BMD measurement and using MOF intervention thresholds required 6.4 scans to identify one patient for treatment whereas the NOGG strategy required 3.5 scans to identify one patient for treatment. These differences also need consideration in guideline development.
This analysis has a number of strengths and limitations. A potential consideration is that some of the risk factor information needed was missing in the cohorts and had to be simulated. The weakness of simulation is that there is a loss of accuracy for those individuals in whom missing variables were simulated. However, this is less relevant for populations, and summary data more closely reflect the sample from which data were drawn with a benefit of optimising sample size. In this context, we checked whether probabilities in the two cohorts studied following simulation differed from the subsets that had all variables. There was no difference in fracture probabilities indicating the adequacy of the simulation. The present analysis was conducted in two referral cohorts and does not necessarily represent the impact of categorisation in the entire population at risk. Moreover, there was evidence of some referral bias. Notwithstanding, the present assessment is not inconsistent with findings from a population-based simulated cohort in the UK [17]. Also, the cohorts were drawn from a different decade, though there was little difference in baseline characteristics between the two cohorts. It should be noted that our analysis could not take into account the recency of a prior fracture. Were this to be taken into account, then the prevalence of very high risk would be expected to increase. There are no empirical data to calculate the quantum of effect but has been indirectly estimated to categorise an additional 2.9% of women age 50 years or more [24].
Finally, it will be important to place the upper intervention thresholds in a health economic perspective. In the context of osteoporosis and fracture risk, the intervention threshold that is relevant for payers can be defined as the probability of fracture at which intervention becomes cost-effective. Whilst NOGG thresholds are driven by clinical appropriateness rather than health-economics, it is still important to underpin the chosen intervention thresholds by cost-effectiveness [40]. The lower intervention threshold (LIT) used in the NOGG guidance provides strategies that are highly cost-effective [26]. The upper intervention thresholds examined in this report require health economic validation using models that can accommodate the heightened risk associated with the recency of fracture [41].
In summary, the present study provides a reference document for further development and updating of country specific osteoporosis guidelines in Austria. It considers the recently recommended category of ‘very high fracture risk’, as well as age-dependent intervention thresholds up to an age of 70 years, and a fixed intervention threshold thereafter. The implementation of an improved case-finding strategy together with less arbitrary but more scientifically driven age-specific FRAX-based intervention thresholds will help improve management of osteoporosis patients in Austria and reduce the marked osteoporosis treatment gap in this country. Furthermore, the characterisation of very high risk may aid in the identification of patients suitable for treatment with osteoanabolic agents.
References
Anonymous (1993) Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med 94:646–650
Svedbom A, Borgström F, Hernlund E, Strom O, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jurisson M, Uuskula A, Lember M, Kallikorm R, Lesnyak O, McCloskey E, Ershova O, Sanders KM, Silverman S, Tamulaitiene M, Thomas T, Tosteson ANA, Jonsson B, Kanis JA (2018) Quality of life after hip, vertebral, and distal forearm fragility fractures measured using the EQ-5D-3L, EQ-VAS, and time-trade-off: results from the ICUROS. Qual Life Res 27:707–716
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780
Tran T, Bliuc D, Hansen L, Abrahamsen B, van den Bergh J, Eisman JA, van Geel T, Geusens P, Vestergaard P, Nguyen TV, Center JR (2018) Persistence of excess mortality following individual nonhip fractures: a relative survival analysis. J Clin Endocrinol Metab 103:3205–3214
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(Suppl 2):S3-7
Warriner AH, Patkar NM, Curtis JR, Delzell E, Gary L, Kilgore M, Saag K (2011) Which fractures are most attributable to osteoporosis. J Clin Epidemiol 64:46–53
United Nations (2022) World population prospects. https://population.un.org/wpp/ Accessed 12 July 2022
Willers C, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, McCloskey EV, Borgström F, Kanis JA and the SCOPE review panel of the IOF (2022) Osteoporosis in Europe: a compendium of country-specific reports. Arch Osteoporos 17:23. https://doi.org/10.1007/s11657-021-00969-8
Dimai HP, Reichardt B, Zitt E, Concin H, Malle O, Fahrleitner-Pammer A, Svedbom A, Brozek W (2022) Thirty years of hip fracture incidence in Austria: is the worst over? Osteoporos Int 33:97–104
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl D, Cyrus Cooper C on behalf of the IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Arznei und Vernunft (2017) Osteoporose—Einatz in Therapie und Prophylaxe. http://www.arzneiundvernunft.at/uploads/171012_Leitlinie_Osteoporose_Onlineversion_580_DE.pdf Accessed 12 July 2022
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV and The Advisory Board of the National Osteoporosis Guideline Group (2016) A systematic review of intervention thresholds based on FRAX. A report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11:25. DOI https://doi.org/10.1007/s11657-016-0278-z
Malle O, Borgstroem F, Fahrleitner-Pammer A, Svedbom A, Dimai SV, Dimai HP (2021) Mind the gap: incidence of osteoporosis treatment after an osteoporotic fracture—results of the Austrian branch of the International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS). Bone 142:115071
The World Bank (2022) GDP growth (annual %)—Austria. https://data.worldbank.org/indicator/NY.GDP.MKTP.KD.ZG?locations=AT Accessed 12 July 2022.
McCloskey E, Kanis JA, Johansson H, Harvey N, Oden A, Cooper A, Cooper C, Francis RM, Reid DM, Marsh D, Selby P, Thompson F, Hewitt S, Compston J (2015) FRAX-based assessment and intervention thresholds—an exploration of thresholds in women aged 50 years and older in the UK. Osteoporos Int 26:2091–2099
Kanis JA, Harvey NC, McCloskey E, Bruyere O, Veronese N, Lorentzon M, Cooper C, Rizzoli R, Adib G, Al-Daghri N, Campusano C, Chandran M, Dawson-Hughes B, Javaid K, Jiwa F, Johansson H, Lee JK, Liu E, Messina D, Mkinsi O, Pinto D, Prieto-Alhambra D, Saag K, Xia W, Zakraoui L, Reginster J (2020) Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int 31:1–12
Kanis JA, Johansson H, Harvey NC, McCloskey EV Lorentzon M, Liu E, Vandenput L, McCloskey EV ∙ National Osteoporosis Guideline Group (2021) An assessment of intervention thresholds for very high risk applied to the NOGG guidelines. A report for the National Osteoporosis Guideline Group (NOGG). Osteoporos Int 32:1951–1960
Khashayar P, Dimai HP, Moradi N, Fahimfar N, Gharibzadeh S, Ostovar A, Nabipour I, Larijani B (2020) Protocol for a multicentre, prospective cohort study of clinical, proteomic and genomic patterns associated with osteoporosis to develop a multidimensional fracture assessment tool: the PoCOsteo Study. BMJ Open 10(e035363):2019–035363
Muschitz C, Dimai HP, Kocijan R, Kaider A, Zendeli A, Kuhne F, Trubrich A, Lung S, Waneck R, Resch H (2013) The discriminatory capacity of BMD measurements by DXA and dual X-ray and laser (DXL) at the calcaneus including clinical risk factors for detecting patients with vertebral fractures. Osteoporos Int 24:2181–2190
Lu Y, Fuerst T, Hui S, Genant HK (2001) Standardization of bone mineral density at femoral neck, trochanter and Ward’s triangle. Osteoporos Int 12:438–444
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC Jr, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. Osteoporos Int 8:468–489
Dawson-Hughes B, Looker AC, Tosteson AN, Johansson H, Kanis JA, Melton LJ,3rd (2010) The potential impact of new National Osteoporosis Foundation guidance on treatment patterns. Osteoporos Int 21:41-52
Kanis JA, Chandran M, Chionh SB, Ganeson G, Harvey NC, Koh WP, Kwok T, Lau TC, Liu E, Lorentzon M, McCloskey EV, Tan KB, Vandenput L, Johansson H (2020) Use of age-dependent FRAX-based intervention thresholds for Singapore. Arch Osteoporos 15(104):020–00782-9
Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M, National Osteoporosis Guideline Group (NOGG) (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62:105–108
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A, National Osteoporosis Guideline Group (2008) Case finding for the management of osteoporosis with FRAX—assessment and intervention thresholds for the UK. Osteoporos Int 19:1395–1408
Kanis JA, Adams J, Borgstrom F, Cooper C, Jonsson B, Preedy D, Selby P, Compston J (2008) The cost-effectiveness of alendronate in the management of osteoporosis. Bone 42:4–15
Kanis JA, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF) (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N, Hope S, Kanis JA, McCloskey EV, Poole KES, Reid DM, Selby P, Thompson F, Thurston A, Vine N, National Osteoporosis Guideline Group (NOGG) (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(43):017–0324-5
Lekamwasam S, Adachi JD, Agnusdei D, Bilezikian J, Boonen S, Borgstrom F, Cooper C, Diez Perez A, Eastell R, Hofbauer LC, Kanis JA, Langdahl BL, Lesnyak O, Lorenc R, McCloskey E, Messina OD, Napoli N, Obermayer-Pietsch B, Ralston SH, Sambrook PN, Silverman S, Sosa M, Stepan J, Suppan G, Wahl DA, Compston JE, Joint IOF-ECTS GIO Guidelines Working Group (2012) A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int 23:2257–2276
Johansson H, Oden A, Johnell O, Jonsson B, de Laet C, Oglesby A, McCloskey EV, Kayan K, Jalava T, Kanis JA (2004) Optimization of BMD measurements to identify high risk groups for treatment—a test analysis. J Bone Miner Res 19:906–913
Gregson CL, Armstrong DJ, Bowden J, Cooper C, Edwards J, Gittoes NJL, Harvey N, Kanis J, Leyland S, Low R, McCloskey E, Moss K, Parker J, Paskins Z, Poole K, Reid DM, Stone M, Thomson J, Vine N, Compston J (2022) Correction: UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 17(1):58. https://doi.org/10.1007/s11657-022-01061-5 (Erratum. In: Arch Osteoporos. 2022 May 19;17(1):80)
National Institute for Health and Care Excellence (2012) NICE clinical guideline 146. Osteoporosis: assessing the risk of fragility fracture. NICE, London.
National Institute for Health and Care Excellence (2012b) Type 2 diabetes: prevention in people at high risk. Public health guideline [PH38] updated 2017 https://www.nice.org.uk/guidance/ph38, accessed 16 June 2021
National Institute for Health and Care Excellence (2020b) British National Formulary (BNF): hypertension https://bnf.nice.org.uk/treatment-summary/hypertension.html, accessed 16 June 2021
National Institute for Health and Care Excellence (2020a) British National Formulary (BNF): cardiovascular disease risk assessment and prevention. https://bnf.nice.org.uk/treatment-summary/cardiovascular-disease-risk-assessment-and-prevention.html, accessed June 2021
Kanis JA, Johansson H, Harvey NC, Lorentzon M, Liu E, Vandenput L, McCloskey EV (2021) An assessment of intervention thresholds for very high fracture risk applied to the NOGG guidelines: a report for the National Osteoporosis Guideline Group (NOGG). Osteoporos Int 32:1951–1960
McClung MR (2021) Role of bone-forming agents in the management of osteoporosis. Aging Clin Exp Res 33:775–791
Camacho PM, Petak SM, Binkley N, Diab DL, Eldeiry LS, Farooki A, Harris ST, Hurley DL, Kelly J, Lewiecki EM, Pessah-Pollack R, Mcclung M, Wimalawansa SJ, Watts NB (2020) American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract 26(Suppl 1):1–46
Curtis EM, Reginster JY, Al-Daghri N, Biver E, Brandi ML, Cavalier E, Hadji P, Halbout P, Harvey NC, Hiligsmann M, Javaid MK, Kanis JA, Kaufman JM, Lamy O, Matijevic R, Perez AD, Radermecker RP, Rosa MM, Thomas T, Thomasius F, Vlaskovska M, Rizzoli R, Cooper C (2022) Management of patients at very high risk of osteoporotic fractures through sequential treatments. Aging Clin Exp Res 34:695–714
Harvey NC, McCloskey E, Kanis JA, Compston J, Cooper C (2018) Cost-effective but clinically inappropriate: new NICE intervention thresholds in osteoporosis (Technology Appraisal 464). Osteoporos Int 29:1511–1513
Soreskog E, Borgstrom F, Lindberg I, Strom O, Willems D, Libanati C, Kanis JA, Stollenwerk B, Charokopou M (2021) A novel economic framework to assess the cost-effectiveness of bone-forming agents in the prevention of fractures in patients with osteoporosis. Osteoporos Int 32:1301–1311
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
HP Dimai has received lecture and consultancy fees from Amgen, Braincon, Daiichi-Sankyo, Eli Lilly, Gedeon Richter, Genericon, Medtronic, Merck Sharp & Dohme, Novartis, Nycomed, Sanabo, Servier, Sinapharm, Stada, UCB, all outside the presented work.
NC Harvey has received consultancy, lecture fees and honoraria from Alliance for Better Bone Health, AMGEN, MSD, Eli Lilly, Servier, Shire, UCB, Kyowa Kirin, Consilient Healthcare, Radius Health and Internis Pharma.
C Muschitz has received speaker honoraria from Amgen, Novartis, Servier, Eli Lilly, Nycomed Pharma/Takeda, Kwizda Pharma, Boehringer Ingelheim, Actavis and Daiichi Sankyo, all outside the presented work.
M Lorentzon has received lecture fees from Amgen, Lilly, Meda, Renapharma, UCB Pharma, and consulting fees from Amgen, Radius Health, UCB Pharma, Renapharma and Consilient Health, all outside the presented work.
A Fahrleitner-Pammer has received research grants from Amgen and Roche, and lecture fees from Amgen, Alexion, EliLilly, Gedeon Richter, Fresenius, Stada, UCB, all outside the presented work.
C Muschitz has received speaker honoraria from Amgen, Novartis, Servier, Eli Lilly, Nycomed Pharma/Takeda, Kwizda Pharma, Boehringer Ingelheim, Actavis and Daiichi Sankyo, all outside the presented work.
EV McCloskey has received consultancy/lecture fees/grant funding/honoraria from AgNovos, Amgen, AstraZeneca, Consilient Healthcare, Fresenius Kabi, Gilead, GSK, Hologic, Internis, Lilly, Merck, Novartis, Pfizer, Radius Health, Redx Oncology, Roche, SanofiAventis, Servier, Synexus, UCB, Viiv, Warner Chilcott, I3 Innovus and Unilever.
JA Kanis is the architect of FRAX but has no financial interest.
P Pietschmann, E Liu, L Vandenput and H Johansson have no competing interests to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dimai, H.P., Johansson, H., Harvey, N.C. et al. Osteoporosis treatment in Austria—assessment of FRAX-based intervention thresholds for high and very high fracture risk. Arch Osteoporos 17, 141 (2022). https://doi.org/10.1007/s11657-022-01175-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01175-w