Abstract
Summary
This narrative review summarises ongoing challenges and progress in the care and prevention of fragility fractures across the Asia Pacific region since mid-2019. The approaches taken could inform development of national bone health improvement Road Maps to be implemented at scale during the United Nations ‘Decade of Healthy Ageing’.
Purpose
This narrative review summarises recent studies that characterise the burden of fragility fractures, current care gaps and quality improvement initiatives intended to improve the care and prevention of fragility fractures across the Asia Pacific region.
Methods
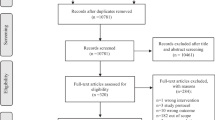
The review focuses on published studies, reports and quality improvement initiatives undertaken during the period July 2019 to May 2022.
Results
Epidemiological studies conducted in countries and regions throughout Asia Pacific highlight the current and projected increasing burden of fragility fractures. Recent studies and reports document a persistent and pervasive post-fracture care gap among people who have sustained fragility fractures. Global initiatives developed by the Fragility Fracture Network and International Osteoporosis Foundation have gained significant momentum in the Asia Pacific region, despite the disruption caused by the COVID-pandemic. The Asia Pacific Fragility Fracture Alliance has developed educational resources including a Hip Fracture Registry Toolbox and a Primary Care Physician Education Toolkit. The Asia Pacific Osteoporosis and Fragility Fractures Society—a new section of the Asia Pacific Orthopaedic Association—is working to engage orthopaedic surgeons across the region in the care and prevention of fragility fractures. The Asia Pacific Consortium on Osteoporosis developed a framework to support national clinical guidelines development groups. Considerable activity at the national level is evident in many countries across the region.
Conclusion
Development and implementation of national Road Maps informed by the findings of this review are urgently required to respond to the epidemiological emergency posed by fragility fractures during the United Nations ‘Decade of Healthy Ageing’.
Similar content being viewed by others
Introduction
At the beginning of the twenty-first century, the human population worldwide was 6 billion, with the 8 billion threshold projected to be crossed in 2023 [1]. While there is ongoing debate among researchers regarding the likely peak global population, and when this will occur [2], the declaration by the United Nations of the ‘Decade of Healthy Ageing’ 2021 to 2030 illustrates a consensus shared by national governments and international institutions that the pace of demographic shift will have an impact on almost all aspects of society [3].
More than 4.6 billion people live in the Asia Pacific region [4], where, as shown in Table 1, 10 of the 20 most populous countries globally are located, accounting for half of the world’s population [5]. In 2017, the United Nations projected that the population aged 65 years or over in Asia and Oceania combined would increase from 417 million in 2020 to 589 million and 947 million in 2030 and 2050, respectively [6]. In the absence of systematic interventions throughout the region, the number of older people living with chronic diseases will increase substantially during the next 30 years, including osteoporosis and the fragility fractures that result from this condition.
The Global Burden of Disease (GBD) 2019 Fracture Study provides the first estimate of the burden of fractures in 204 countries and territories, by age, sex, and year, from 1990 to 2019 [7]. The GBD Study estimated in 2019 that there were 178 million new fractures, 455 million prevalent cases of acute or long-term symptoms of a fracture and 25.8 million years lived with disability. The majority of fractures occurred in older adults, with increases in age-specific incidence becoming evident around age 50 to 54 years in females and 65 to 69 years in males. Substantial increases in age-specific incidence occurred from age 80 years onwards for both sexes. Of the 4 sets of recommendations made by the GBD Study authors, the first and third relate to older adults:
-
Firstly, efforts should be made to:
-
Expand screening and treatment of osteoporosis in older people.
-
Encourage exercise and diet that promotes bone strength throughout the life course.
-
Provide educational materials, assistive devices and other products to reduce the risk of falls.
-
-
Thirdly, particularly in countries with the highest age-standardised disability burdens due to fractures, there should be a focus on development of evidence-based policies to prevent fractures.
During the 2010s, considerable efforts were undertaken at the global, regional, national and local levels throughout the world to address the challenge presented by fragility fractures. In December 2019, Ebeling et al. published a comprehensive review on attempts to improve the care and prevention of fragility fractures in the Asia Pacific region [8]. In the 2 years since that work was published, the world has been engulfed by the greatest public health crisis in a century. However, throughout the pandemic, the fragility fracture and osteoporosis community has been very active in the publication of new evidence on the burden of fragility fractures, and development of new initiatives to improve outcomes for patients, healthcare systems and national economies.
The purpose of this narrative review is to characterise the current burden of fragility fractures and care gaps across the Asia Pacific region, and summarise recent quality improvement initiatives. While the emergence of SARS-CoV-2 has impacted every country on Earth, as noted by the Fragility Fracture Network (FFN) [9] and the International Osteoporosis Foundation (IOF) [10], humankind is en route to a new demographic era. A critical component of our response to this transition must be to prevent as many fragility fractures as possible, and to restore and maintain mobility for the many millions of people who will continue to sustain these injuries in the years to come.
The burden of fragility fractures in the Asia Pacific region
In 2018, the Asian Federation of Osteoporosis Societies (AFOS) published an update to hip fracture projections for 2018 and 2050 for mainland China, Hong Kong Special Administrative Region (SAR), India, Japan, Malaysia, Singapore, South Korea, Taiwan and Thailand [11]. The total incidence and associated costs were estimated to be as follows:
-
In 2018, 1.1 million hip fractures at a direct cost of US$7.4 billion.
-
In 2050, 2.5 million hip fractures at a direct cost of US$13 billion.
The purpose and summaries of key findings from more recent epidemiological studies conducted in countries and regions in Asia Pacific are provided in Table 2. Recent reviews have also been published on the burden of hip fracture by Ong et al. for Malaysia [12] and Pandey et al. for Nepal [13]. As noted previously, the GBD Study provides for the first time estimates for 204 countries and territories on the total fracture burden [7]. While not specifically focused on fragility fractures, the source tables for each country and territory could provide useful estimates of the burden of disease among individuals aged 50 years or over, where the majority of fractures are likely to be a consequence of low-trauma incidents. The conclusion of an editorial by Dare and Hu [14] that commented upon the first major publication from the China National Fracture Study in 2017 sums up the key findings of studies in Table 2:
“In emerging economies, transport injuries have occupied centre place in research and policy efforts directed towards unintentional injuries. By contrast, fragility fractures from minor trauma have been completely absent from injury prevention dialogue. This study shows that fragility fractures are an important contributor to injury burden in China, and will continue to be as the population ages. Primary and secondary prevention of osteoporosis and fragility fracture using proven lifestyle, medication, and environmental measures targeted to at-risk groups must be included within China’s injury control strategies, and should be considered by other middle-income countries facing similar health and demographic changes.”
Post-fracture care in the Asia Pacific region
In 2019, the review published by Ebeling et al. [8] summarised studies that described the secondary fracture prevention care gap across the Asia Pacific region. The following reports and peer-reviewed studies published after the 2019 review suggest that the care gap continues to be widespread.
Australia and New Zealand
The Australian and New Zealand Hip Fracture Registry (ANZHFR) [30] enables hospitals to benchmark the care that they provide against the bi-national Hip Fracture Care Clinical Care Standard [31] published jointly in 2016 by the national healthcare quality organisations in both countries. The ANZHFR Annual Report for 2021 [32] documented the care of 14,816 hip fractures in 86 hospitals during calendar year 2020. Key findings relating to secondary fracture prevention included the following:
-
In Australia:
-
Overall, 26% of individuals with hip fracture left hospital on a bisphosphonate, denosumab or teriparatide, compared with 10% that were taking treatment on admission.
-
At 120 days, follow-up rates were low and 36% of patients reported receiving bone protection.
-
During their inpatient stay, 69% of patients were reported to have undergone a falls assessment.
-
-
In New Zealand:
-
Overall, 29% of individuals with hip fracture left hospital on a bisphosphonate, denosumab or teriparatide, compared with 9% that were taking treatment on admission.
-
At 120 days, follow-up was over 90%, and 40% of patients reported receiving bone protection medication.
-
During their inpatient stay, 79% of patients were reported to have undergone a falls assessment.
-
In response to the sub-optimal level of osteoporosis treatment on discharge, ANZHFR conducted a ‘sprint audit’ in late 2021 to examine the issues relating to osteoporosis treatment that was published in 2022 [33]. Further, as described in the next section of this publication, a new Australian and New Zealand Fragility Fracture Registry [34, 35] has been established to benchmark the care provided by Fracture Liaison Services for individuals who sustain fragility fractures at all skeletal sites.
China
In 2020, Wang et al. [36] investigated anti-osteoporosis drug treatment rates among individuals aged over 50 years (n = 27,342) who had presented with fractures to 37 hospitals in Fujian during the period 2010 to 2016. Overall, 22.1% of women and 9.5% of men received treatment within 12 months of fracture. Notably, use of bisphosphonates was particularly low, at just 5.3% for women and 1.5% for men. The majority of individuals (90.5%) who received anti-osteoporosis treatment received calcitonin.
In 2021, Wang et al. [18] described the prevalence of osteoporosis and clinical and vertebral fractures among adults aged 40 years or over (n = 20,164) in mainland China. Osteoporosis was diagnosed if the individual met at least one of the following criteria:
-
A bone mineral density (BMD) T-score of − 2.5 or less at any site (L1 to L4, femoral neck or total hip).
-
The individual had a vertebral fracture of grade 2 or higher based on radiographic findings.
-
The individual had sustained a clinical fracture during the previous 5 years based on a questionnaire.
Osteoporosis-specific treatments were considered to include bisphosphonates, calcitonin, oestrogen, parathyroid hormone analogues, selective oestrogen receptor modulators or an active form of vitamin D or an analogue. On this basis, among men and women, 0.3% (95% confidence interval [CI], 0.0–0.7%) and 1.4% (95% CI, 0.8–2.0%), respectively, diagnosed with osteoporosis were treated with an osteoporosis specific treatment.
Japan
In 2020, Shimodan et al. [37] evaluated post-fracture care during the period 2008 to 2017 for individuals (n = 4764) who presented with hip fracture to seven hospitals in Hokkaido prefecture. Overall, prior to hip fracture, 8.4% of individuals had taken an osteoporosis specific treatment, which increased to 34.2% after hip fracture. In 2012, one hospital introduced an Osteoporosis Liaison Service (OLS) [38], as did two other hospitals in 2015. Post-fracture osteoporosis treatment rates were approximately four times higher in the hospitals with an OLS compared to those without this service.
In 2021, Nakatoh et al. [39] described BMD testing and osteoporosis treatment rates among a very large sample of individuals with hip fractures (n = 677,480 women and 264,003 men), vertebral fractures (n = 703,247 women and 251,542 men) and mixed fractures, i.e. the individual had sustained two fractures on the same day (n = 3614 women and 1055 men). The investigators utilised medical insurance data from the National Database of Health Insurance Claims and Specific Health Check-ups of Japan for the period April 2012 to March 2019. Key findings included:
-
BMD testing after fracture was undertaken for 22.3%, 43.6% and 28.1% of the hip fracture, vertebral fracture and mixed fracture groups, respectively.
-
Osteoporosis treatment within 12 months of fracture was received by 31.9%, 61.7% and 46.6% of the hip fracture, vertebral fracture and mixed fracture groups, respectively.
Singapore
In 2020, Chau et al. [40] sought to identify factors that contributed to initiation of osteoporosis treatment among individuals aged over 50 years (n = 347) who were admitted with hip fracture to the National University Hospital during the period 2014 to 2016. Overall, 40.3% of individuals were prescribed an osteoporosis medication within 12 months of fracture, defined as a bisphosphonate, denosumab or teriparatide. Individuals who underwent BMD testing post-fracture were almost four times as likely to be initiated on osteoporosis treatment (odds ratio [OR], 3.97; 95% CI, 2.24–7.03), and individuals who had 25-hydroxyvitamin D measured post-fracture were more than twice as likely to receive treatment (OR, 2.16; 95% CI, 1.09–4.27).
South Korea
In 2019, Kim et al. [41] analysed the rate of diagnosis of osteoporosis among individuals aged over 50 years with newly diagnosed distal radius fractures (DRF). A search of the national Korean Health Insurance Review and Assessment Service identified 77,209 DRFs from 2011 to 2016 that met all study inclusion criteria. Within 6 months after the fracture, one quarter (n = 19,305) underwent diagnostic examinations for osteoporosis. Higher rates were evident among patients aged 70 to 79 years (39.9%) and among those who attended a tertiary hospital (32.9%), while males were less likely to be assessed than women (10% vs 30%).
Global, regional, national and local quality improvement initiatives
Since 2019, a broad array of initiatives has been launched with the intention of improving various aspects of the care of individuals who sustain fragility fractures. A summary of initiatives at the global, regional, national and local levels in Asia Pacific follows.
Global initiatives
Global Call to Action on Fragility Fractures
From 2016 to 2018, the following six organisations collaborated to develop the Global Call to Action on Fragility Fractures [42]:
-
European Federation of National Associations of Orthopaedics and Traumatology (EFORT)
-
European Geriatric Medicine Society (EuGMS)
-
Fragility Fracture Network (FFN)
-
International Collaboration of Orthopaedic Nursing (ICON)
-
International Geriatric Fracture Society (IGFS)
-
International Osteoporosis Foundation (IOF)
The Call to Action called for urgent improvement in three so-called clinical pillars, those being acute multidisciplinary care, rehabilitation and secondary fracture prevention. The fourth pillar was political in nature, calling for the assembly of multidisciplinary national alliances to advocate policy change that supports implementation of the three clinical pillars.
Since publication, FFN has focused on supporting efforts to turn the Call to Action into actual action at the national level. In this regard, FFN has developed a comprehensive suite of resources in collaboration with colleagues throughout the world that are available in several languages, including the following:
-
Textbooks:
In 2020, FFN and IOF signed a Memorandum of Understanding which established a framework to optimise collaboration, including mutual endorsement of flagship initiatives.
Capture the Fracture®
The IOF Capture the Fracture® programme was launched with publication of the 2012 World Osteoporosis Day thematic report [47] and has become an IOF flagship initiative during the ensuing decade. The aims of the Capture the Fracture® programme are as follows:
-
1.
To be the global voice for secondary fracture prevention
-
2.
To drive national/international policy and prioritisation of secondary fracture prevention
-
3.
To ensure quality in secondary fracture prevention
-
4.
To provide support for FLS implementation, improvement and sustainability
In 2013, an international expert panel developed and published a Best Practice Framework with 13 internationally endorsed standards that, for the first time, set an international benchmark for FLS which defines essential and aspirational elements of service delivery [48]. In 2020, the IOF Capture the Fracture® Working Group in collaboration with the FFN Secondary Fragility Fracture Prevention Special Interest Group and the Bone Health and Osteoporosis Foundation (formerly the National Osteoporosis Foundation, USA) published a patient-level key performance indicator set [49] to measure the effectiveness of FLS and guide quality improvement.
In late 2019, an expansion of the Capture the Fracture® initiative was launched, the Capture the Fracture® Partnership programme [50], which represented the largest partnership to date between a non-governmental organisation, focused on osteoporosis as well as secondary fracture prevention, academics and global corporate stakeholders. This partnership focuses on five key pillars of action across 18 countries in Asia Pacific, Europe, Latin America and the Middle East:
-
Pillar 1—Policy: drive fracture prevention policy changes that will prioritise bone health and post-fracture care through the implementation of FLS.
-
Pillar 2—Coalitions: creation of international/regional/national fracture prevention coalitions to support the Capture the Fracture® mission, i.e. to make secondary fracture prevention a top health priority.
-
Pillar 3—Mentorship: FLS Best Practice Mentorship and Workshops to help promote the implementation of new FLS programmes, improve existing FLS programmes and ensure sustainability.
-
Pillar 4—Scalable solutions: establish scalable solutions to support FLS with quality improvement and scalability.
-
Pillar 5—FLS Digital Tool: creation of a global FLS database comparative tool which will help hospitals to develop quality improvement plans, facilitate the management of the patient pathways and achieve sustainable FLS.
As of August 2022, 762 FLS from 50 countries featured on the IOF Capture the Fracture® Map of Best Practice [51].
Regional initiatives in Asia Pacific
Asia Pacific Fragility Fracture Alliance
Launched in November 2018, the Asia Pacific Fragility Fracture Alliance (APFFA) [52] comprises the following seven regional and global organisations:
-
Asian Federation of Osteoporosis Societies (AFOS)
-
Asia-Oceanian Society for Physical and Rehabilitation Medicine (AOSPRM)
-
Asia Pacific Geriatric Network (APGN)
-
Asia Pacific Orthopaedic Association (APOA)
-
Fragility Fracture Network (FFN)
-
International Osteoporosis Foundation (IOF)
-
International Society for Clinical Densitometry (ISCD)
The primary purpose of APFFA is to drive policy change, improve awareness and change political and professional mindsets to facilitate optimal fracture management across Asia Pacific. The ‘engine room’ of APFFA is the three Working Groups that are focused on Hip Fracture Registries, Education and Evidence Generation.
In 2020 and 2021, the APFFA Hip Fracture Registry Working Group collaborated with the FFN Hip Fracture Audit Special Interest Group to develop a Hip Fracture Registry Toolbox [53]. The Toolbox provides a distillation of learning from established registries throughout the world and summarises essential components of national quality improvement programmes for hip fracture care. As of August 2022, the Toolbox is available in English, both simplified and traditional Chinese, Japanese and Korean. In 2022, a Feasibility Study has been initiated to document ongoing initiatives to improve hip fracture care across the region, facilitate widespread dissemination of existing resources and understand enablers and barriers at the national level to inform development of new hip fracture registries. In addition, in 2022, the Working Group will publish comprehensive literature reviews on the epidemiology of hip fracture, and mortality and outcomes after hip fracture in the Asia Pacific region.
In 2020, the APFFA Education Working Group launched the APFFA Primary Care Physician (PCP) Education Toolkit [54] designed to provide PCPs with practical resources to improve the identification, assessment and ongoing management of individuals at risk of fractures. A major communications effort was undertaken to disseminate the Toolkit to relevant professional organisations throughout the Asia Pacific region.
Additional activities of the APFFA Education Working Group include:
-
Education directory: A curated collection of existing educational materials relating to the management of acute care, rehabilitation and secondary prevention of fragility fractures, accessible through a user-friendly, readily searchable interface [55].
-
Systematic literature review: An outgrowth of the congress presentations is a comprehensive literature review to determine perceptions about the importance of treating fragility fractures and osteoporosis among the various stakeholder groups. This includes the general public, patients, primary care, specialist physicians, administrators and government officials. A manuscript is in development that will be submitted to a peer-reviewed journal for publication in 2022.
-
Congress Participation: Throughout the pandemic, APFFA Working Group activities have been presented at global and regional congresses.
The APFFA Evidence Generation Working Group has led drafting of this narrative review and is undertaking a survey of awareness and attitudes to the management of fragility fractures among the membership of the Asia Pacific Orthopaedic Association, in collaboration with the Asia Pacific Osteoporosis and Fragility Fracture Society, a recently established section of the Asia Pacific Orthopaedic Association.
Asia Pacific Orthopaedic Association
The Asia Pacific Orthopaedic Association (APOA) is one of the largest orthopaedic associations in the world with a unique membership structure [56]. This includes 700 individual members from 16 national chapters, 12 speciality sections and 21 federation members (i.e. national orthopaedic associations or societies) with more than 60,000 federation fellows in total. In 2021, IOF Asia Pacific and APOA collaboratively developed and published a Call to Action for orthopaedic surgeons and physicians to close the care gap in secondary fracture prevention [57]. Two APOA sections are concerned with fragility fractures, those being the recently established Asia Pacific Osteoporosis and Fragility Fracture Society (APOFFS) [58] and the Asia Pacific Trauma Society (APTS) [59]. The objectives of APOFFS are as follows:
-
1.
To recognise the increased burden of osteoporosis and fragility fractures in the Asia Pacific region.
-
2.
To recognise that among the orthopaedic community, osteoporosis is often underdiagnosed and undertreated in patients being treated for fragility fractures.
-
3.
To play a more important role to ensure early diagnosis, fracture risk assessment, appropriate pharmacological intervention to prevent fragility fractures.
-
4.
To recognise the challenges in fragility fracture management, in particular appropriate surgical treatment, to allow early rehabilitation and to achieve best functional status possible.
-
5.
To equip orthopaedic surgeons with knowledge, interest and confidence to initiate and continue pharmacological treatments for osteoporosis.
-
6.
To promote orthogeriatric care in order to achieve best possible outcome for patients presenting with fragility fracture.
-
7.
To encourage orthopaedic surgeons to lead the development and implementation of Fracture Liaison Services and Hip Fracture Registries.
-
8.
To collaborate with both orthopaedic and non-orthopaedic organisations at the regional and global level to promote osteoporosis and fragility fracture care.
Asia Pacific Consortium on Osteoporosis
Launched in May 2019, the Asia Pacific Consortium on Osteoporosis (APCO) currently comprises 46 osteoporosis specialists from 20 countries and regions across Asia Pacific, representing multiple medical and surgical specialties [60]. The primary aim of APCO is to develop regionally relevant strategies for improving osteoporosis management and reducing rates of fragility fractures. In 2021, APCO published a framework [61] to support national clinical guidelines development groups to draft new, or revise existing, osteoporosis clinical guidelines to be consistent with a set of clear, concise, relevant and pragmatic clinical standards. The 16 clinical standards are organised in accordance with so-called 5IQ approach used previously by other groups to develop national clinical standards for Fracture Liaison Services [62,63,64]:
-
Identification: Statements relating to which individuals should be identified.
-
Investigation: Description of the types of investigations that will be undertaken.
-
Information: Description of the types of information to be provided to patients and families.
-
Intervention: Description of pharmacological interventions and falls prevention.
-
Integration: Statements on the need for integration between primary and secondary care.
-
Quality: Description of professional development, audit and peer-review activities.
To facilitate peer-to-peer education among healthcare professionals on the APCO Framework, a comprehensive suite of education modules has been developed [65]. This educational resource includes modules relating to each of the 16 APCO Framework clinical standards and an additional module on recently emerging themes in osteoporosis care. Each module provides an overview of the evidence base that underpins the clinical standards including epidemiological data, examples of best practice and discussion questions. Translations are ongoing into other languages including Chinese, Korean and Japanese. In May 2022, the APCO Bone Health Quality Improvement (QI) Tool Kit was launched, which focuses on seven selected standards from the APCO Framework that are applicable to the clinical setting, and is available from the APCO website [60].
National and local initiatives in Asia Pacific
Australia and New Zealand
In late 2019, the Department of Health of the Australian Government published the National Strategic Action Plan for Osteoporosis with the following priorities [66]:
-
Priority Area 1: Awareness and education with a focus on prevention
-
Priority Area 2: Improved diagnosis, management and care
-
Priority Area 3: Data collection, monitoring and strategic research
During the period 2020 to 2022, to complement the established Australian and New Zealand Hip Fracture Registry [30], a new Australian and New Zealand Fragility Fracture Registry has been developed in both countries [34, 35]. This initiative is being led by the SOS Fracture Alliance in Australia [67] and Osteoporosis New Zealand [68].
In 2021, Osteoporosis New Zealand published the second edition of Clinical Standards for Fracture Liaison Services in New Zealand [64]. The launch of the New Zealand-arm of the Fragility Fracture Registry in 2022 will enable Fracture Liaison Services across the country to benchmark the care that they provide against the clinical standards. This is a central component of a national quality improvement programme being undertaken collaboratively between Osteoporosis New Zealand, the Accident Compensation Corporation (ACC, the government agency responsible for injury prevention in New Zealand) and the health sector [69], and represents the most recent phase of the national Live Stronger for Longer programme [70].
China
In October 2021, Professor Maoyi Tian delivered a webinar on recent progress in hip fracture care in China [71]. The webinar summarised a major body of work conducted at Beijing Jishuitan Hospital to evaluate multidisciplinary approaches to hip fracture management, including:
-
A comparison of delivery of care at Beijing Jishuitan Hospital with benchmarking against clinical standards for UK hospitals reported by the UK National Hip Fracture Database [72].
-
A ‘pre- and post-’ analysis of implementation of a multidisciplinary model of hip fracture care at Beijing Jishuitan Hospital which demonstrated highly favourable results for the new model [73].
-
A qualitative study using normalisation process theory and mapping to understand implementation aspects of multidisciplinary programmes in the Chinese context [74].
-
A cost-effectiveness analysis of the multidisciplinary co-management programme at Beijing Jishuitan Hospital which reported a 78% chance that the model was cost-effective in relation to the Chinese willingness-to-pay threshold [75].
-
A multicentre study to evaluate the effectiveness of the multidisciplinary model in three urban and three suburban hospitals, which demonstrated significant improvements in undertaking surgery within 48 h, osteoporosis assessment, rehabilitation, length of hospital stay, in-hospital mortality and cumulative mortality at 12 months [76].
In January 2021, a policy round table meeting was held to disseminate the findings of the studies described above to government officials from the National Health Commission of the People’s Republic of China [77]. In April 2021, the National Health Commission delegated Beijing Jishuitan Hospital to develop a national clinical management guideline for hip fracture, which will be informed by national guidelines from Australia and New Zealand [78], Scotland [79], UK [80] and USA [81].
Development of a Chinese National Hip Fracture Registry is also underway. A Delphi consultation is in process to achieve an expert consensus of the core variables to be collected in the registry, which is being informed by variables captured within 13 national hip fracture registries worldwide. Development of a technology platform is ongoing, which will be subject to pilot testing in selected hospitals to evaluate feasibility.
The webinar concluded with a summary of the following plans for future work:
-
A large-scale randomised clinical trial to provide definitive evidence on the benefits of the multidisciplinary approach in the Chinese context.
-
Application of implementation science to bridge the gaps between the evidence base and routine clinical practice.
-
Promotion of the integrated care model for older people.
-
Engagement with consumers, communities, governments and other partners to identify ongoing approaches to improvement.
Hong Kong SAR, China
In 2019, Wong et al. evaluated secondary fracture incidence for individuals who presented with a hip, proximal humerus or distal radius fragility fracture to all public acute hospitals in Hong Kong SAR from 2004 to 2018 [19]. For the period 2009 to 2013, the average cumulative incidence of secondary fractures was 3.9% and 6.5% at 1 and 2 years after the index fracture, respectively. Almost half (49.5%) of patients with secondary fractures sustained these fractures within 2 years of the index fracture. An analysis of 2286 hip fracture patients in Hong Kong SAR by Wong et al. also showed that those with good premorbid function, increased age, lower pre-operative American Society of Anaesthesiologists (ASA) grade and male patients correlated with mobility deterioration at 1-year post surgery [82], reinforcing the importance of prompt rehabilitation. Therefore, Wong et al. also proposed a model for FLS in Hong Kong SAR [83] that would be adherent with the IOF Capture the Fracture® Best Practice Framework [48]. In 2021, the same group described a new FLS model focused on vertebral compression fractures [84]. The Fragility Fracture Network Hong Kong SAR was also established in 2021.
Japan
In 2019, Clinical Standards for Fracture Liaison Services in Japan were developed by a multidisciplinary Working Group of experts and published by the Fragility Fracture Network Japan and the Japan Osteoporosis Society [63]. The clinical standards were endorsed by the following learned societies and organisations:
-
Bone and Joint Japan
-
Japan Osteoporosis Foundation
-
Japan Society for Musculoskeletal Nursing
-
Japanese Society for Fracture Repair
-
Japanese Association on Sarcopenia and Frailty
-
Japanese Orthopaedic Association
-
Japanese Society for Falls Prevention
-
Japan Geriatrics Society
In 2021, Shigemoto et al. described a 5-year experience of implementation of a multidisciplinary care model for hip fracture patients at Toyama City Hospital in Japan [85, 86]. Notably, the mean time to surgery achieved was 1.7 days, as compared to the national average of 4.5 days in 2014 [87]. Given that recent estimates suggest that 226,000 hip fractures occurred in Japan in 2020 [88], if the national average time to surgery has not changed since 2014, 632,800 pre-operative bed days could be saved if the Toyama model was implemented nationwide. Additional benefits of the model included very high osteoporosis treatment rates on discharge (90.7%) and at 12-month follow-up (84.7%), and 14% lower total hospitalisation costs per person during the 5-year study period compared to the average for about 400 other hospitals in Japan.
In April 2022, the Ministry of Health, Welfare and Labour introduced a new reimbursement scheme for hip fracture patients that incentivises hospitals to undertake surgery within 48 h and deliver evidence-based secondary fracture prevention [89].
Malaysia
Recent initiatives in Malaysia are summarised below.
Formation of Fragility Fracture Network Malaysia
The Fragility Fracture Network Malaysia (FFN-M) was formed in August 2018 [90]. The FFN-M Council is multidisciplinary, with representation from orthopaedic surgery, geriatric medicine, rehabilitation medicine, physiotherapy, emergency medicine and anaesthesiology. The objectives of FFN-M are as follows:
-
1.
To create a national network of fragility fracture experts from different states throughout Malaysia.
-
2.
To generate priority for fragility fracture care in all hospitals throughout Malaysia.
-
3.
To spread the best multidisciplinary practice (orthogeriatrics and rehabilitation) and systems of care for managing fragility fractures nationwide.
-
4.
To ensure that every fragility fracture becomes an opportunity for preventing further fractures by promoting Fracture Liaison Services nationwide.
-
5.
To promote research aimed at improving the quality of fragility fracture care.
-
6.
To establish a fragility fracture registry, in particular a National Fragility Fracture Registry for hip and non-hip fractures.
-
7.
To establish guidelines and standard of best practice in managing various fragility fractures.
-
8.
To allow patients presenting with fragility fractures to return to their best functional status possible.
Implementation of Fracture Liaison Services
A series of FLS workshops, webinars and training courses have been carried out nationwide, both in-person and virtual. Many orthopaedic surgeons, geriatricians, paramedics and nurses participated in the programme, which has generated considerable interest to learn about FLS and initiate services in participants’ hospitals. A Mentor–Mentee programme was also initiated following the programme. The most important part of the FLS programme is the initiation and near completion of the FFN-M FLS Framework, scheduled for launch in the second half of 2022. The FLS Framework is intended to guide existing FLS to improve their performance and facilitate initiation of new FLS in hospitals without a service.
As part of the FLS programme, the orthogeriatric service model [43] was strongly promoted in hospitals with geriatricians. However, with the rarity of geriatricians in the country, FFN-M has promoted ‘Orthogeriatric services’ with other physicians working closely with orthopaedic surgeons and other supporting team members.
Collaboration of Fragility Fracture Network Malaysia and Malaysian Orthopaedic Association
The first FFN-M–Malaysian Orthopaedic Association (MOA) Collaboration virtual meeting was held in February 2022. Subsequently, an FFN-M-MOA Task Force was formed with three members from each organisation. The following objectives of the collaboration were discussed:
-
1.
To recognise the ageing population, increased burden of osteoporosis and fragility fractures in Malaysia.
-
2.
To recognise that osteoporosis is under-diagnosed and under-treated in patients being treated for fragility fractures among the orthopaedic community.
-
3.
To equip orthopaedic surgeons with knowledge, interest and confidence, and to promote a more important role among orthopaedic surgeons to ensure early diagnosis, fracture risk assessment, appropriate pharmacological intervention to prevent primary and secondary fragility fractures.
-
4.
To close the care gap for patients with fragility fracture by closing the gap between orthopaedic surgeons and physicians and provide multidisciplinary care to allow early rehabilitation.
-
5.
To promote orthogeriatric care, with or without geriatricians in order to achieve the best functional outcome possible for patients presenting with fragility fracture.
-
6.
To encourage orthopaedic surgeons to lead the development and implementation of FLS and a Malaysian Hip Fracture Registry.
The combined efforts will include dissemination of the FFN-M FLS Framework, promoting webinars and live sessions of FLS training, promoting the FLS Mentor–Mentee Program, working together towards establishing a Malaysian Hip Fracture Registry, a hip fracture clinical pathway and promoting orthogeriatric services with and without geriatricians in various hospitals.
The 51st MOA Annual Scientific Meeting held in June 2022 had the theme ‘Greying Gracefully: The New Paradigm for Orthopaedics in An Ageing Population’ [91]. This was the first time that MOA organised the Annual Scientific Meeting with the theme of orthopaedics and ageing. There were two symposia on orthogeriatric care and also other symposia on spine surgery for the older person, arthroplasty for the ageing population and others. The meeting intended to raise awareness among all members of MOA and prepare them to consider problems associated with the ageing population in Malaysia. This will also be the best platform for the collaboration between FFN-M and MOA.
Formation of Bone Health Alliance Malaysia
The Bone Health Alliance Malaysia (BHAM) was officially launched in January 2021. BHAM consists of three organisations: the Malaysian Osteoporosis Society (MOS), Osteoporosis Awareness Society of Kuala Lumpur and Selangor (OASKLS) and FFN-M. BHAM is mainly focused on raising awareness among the general public about various aspects of osteoporosis and fragility fractures. Materials on public education, including articles and videos have been posted on Facebook, relating to the importance of prevention, risk identification, early diagnosis, treatments, primary and secondary fracture prevention, as well as post fracture care.
Philippines
In 2020, the University of the Philippines-Philippine General Hospital (UP-PGH) Orthogeriatric Multidisciplinary Fracture Management Model and Fracture Liaison Service, the first FLS programme in the country, received its bronze level recognition in the IOF Capture the Fracture® programme [92]. The combined Orthogeriatric and FLS multidisciplinary unit aims to bridge the gap in the care of elderly patients with fragility hip fractures, in both the in-hospital and outpatient services in a country with low resource settings. The National University Hospital’s Orthogeriatric-FLS unit set an example to other hospitals in the country on how to improve the management of fragility hip fractures despite the economic challenges of being a country with an emerging economy.
Since its establishment, immediate impact of the combined Orthogeriatric-FLS model of care was seen, as it resulted in a decrease in the time from admission to surgery, as well as the overall length of stay of elderly patients with fragility hip fractures. Patient follow-up rates and compliance to anti-osteoporosis medications are at 96% and 72% respectively [93]. A single-centre retrospective study, using the UP-PGH Orthogeriatric-FLS programme database, also revealed a computed economic burden of patients with acute fragility hip fractures in the Philippines to be at PhP 1,094,048,363 (US$ 22,595,007) per annum, with a median cost of treatment showing to be less in the group of early hospitalised patients compared to those with delayed hospitalisation [94].
The Philippines now has six hospitals with a FLS on the IOF Capture the Fracture® map. Despite the challenges brought about by the COVID pandemic, an expansion of the combined Orthogeriatric-FLS model undertaken in the second quarter of 2022. This expansion project was supported by a start-up Hip Fracture Registry which initially involved 14 hospitals in the country. Learnings from the FFN Clinical [9] and Policy [46] Toolkits, the IOF Capture the Fracture® programme [92], the Asia Pacific Bone Academy (APBA) FLS educational initiative [95] and the Asia Pacific Fragility Fracture Alliance-FFN Hip Fracture Registry Toolbox [53] were all major influences in the formation and implementation of this planned programme. The programme is funded by the Department of Science and Technology (DOST)-Philippine Council for Health Research and Development. The hope is that this will expand the hospitals with orthogeriatric centres and FLS, as well as lay the seeds for a sustainable Hip Fracture Registry in the Philippines.
South Korea
In 2018, the Fragility Fracture Network of Korea (FFN-Korea) was organised under the leadership of the FLS Committee supported by the Korean Society of Bone and Mineral Research (KSBMR). The inaugural meeting was held in the form of the FLS Educational Symposium in October 2018. The first FLS Guidebook, aimed at developing a Korean ‘Blue Book’ by benchmarking against the British Blue Book [96], was published in January 2019. In 2019, FLS coordinator education symposiums were held on four occasions supported by KSBMR. Since 2020, various virtual forms of coordinator education programmes have been provided to maintain training and educational activities for coordinators’ education despite the pandemic. A multicentre observational trial to investigate the effect of FLS on awareness of osteoporosis and its treatment improvement has been conducted in 11 regional hospitals across the country. Cha et al. reported current efforts to establish FLS in Korea and highlighted implementation challenges, such as the lack of awareness regarding the importance of this system and the lack of support by healthcare systems and health policies [97].
From 2019, the clinical practice guideline for postoperative rehabilitation after hip fracture in older patients with hip fractures was developed based on the level of evidence of relevant literature and the consensus of multidisciplinary experts. This guideline was published in 2021 and presented comprehensive recommendations for the rehabilitation of adult patients after hip fracture surgery [98].
In 2021, the Korea Ministry of Health and Welfare launched the pilot programme of home-based medical care, which is linked between acute hospital care and home-based care. The fees for education, discharge care plan and home-based monitoring are funded by the National Health Insurance system. Patients who receive major orthopaedic surgeries following fragility fractures are the target of this model as one of the indications. Given the potential restrictions and patients’ fear of face-to-face visits during the pandemic, this system allows patient education and home-based monitoring to be provided with telemonitoring and online communication. This pilot programme is a meaningful start to reimburse the coordinator-led clinical activities including patient education and home-based monitoring. It is expected to contribute to the implementation of integrated fragility fracture care in the clinical setting.
In addition to these improvements in care delivery and the two studies described in Table 2, large-scale epidemiological studies have been published during the pandemic on risk factors for second hip fractures [99] and secondary fragility fractures [100].
Taiwan
In 2020, Hsu et al. evaluated the impact of osteoporosis medication persistence on subsequent fractures and all-cause mortality in hip fracture patients (n = 946) in Taiwan [101]. Medication persistence was defined as ‘… the continuous use of the same categorical medication from initiation to the first discontinuation of medication (at least 60 days without any refill) or the end of follow-up’. Discontinuation was defined specifically for each treatment to reflect the frequency of dosing for the particular treatment. Further, medication persistence was categorised as Yes (i.e. ≥ 12 months) or No (i.e. < 12 months). The persistent group of patients had a 36% lower fracture risk (adjusted hazard ratio [aHR] = 0.64; 95% CI, 0.41–0.99; p = 0.043) during the follow-up period. No significant effect on all-cause mortality was observed.
In 2021, Huang et al. described the impact of a rehabilitation-based multidisciplinary care model for hip fracture patients (n = 185) [102]. The Integrated Hip Fracture and Osteoporosis Rehabilitation Program for the Elderly (i-HOPE) devised an individualised rehabilitation plan, which included osteoporosis treatment and promotion of self-care techniques to improve the home environment. Statistically significant reductions during the first year after fracture were reported for falls (absolute risk reduction [ARR], 8%; p = 0.02), refractures (ARR, 7%; p = 0.03) and all-cause mortality (ARR, 11%; p = 0.01).
In 2021, Chang et al. evaluated 1-year outcomes of an OLS, comprised of a FLS and medication management services (MMS) to improve adherence with medication [103]. The FLS programme enrolled patients with new hip fractures or untreated vertebral fractures (n = 600) and the MMS programme enrolled patients with osteoporosis medication issues (n = 499). Care coordinators contacted patients by telephone every 4 months for a year to evaluate ongoing care based on an adaptation of the IOF Capture the Fracture® Best Practice Framework standards [48]. Key findings included the following:
-
FLS Cohort: The proportion of patients receiving osteoporosis-specific treatment increased from 10.7% before enrolment to 78.8% after enrolment (p < 0.05) and was 81.9% at 12-month follow-up.
-
MMS Cohort: The proportion of patients receiving osteoporosis-specific treatment increased from 40.9% before enrolment to 100% after enrolment and was 90.5% at 12-month follow-up.
Significant benefits for the entire cohort were also observed in relation to fall rates, exercise rates, calcium intake, vitamin D intake and adequate protein intake.
In 2022, Chien et al. undertook a real-world cost-effectiveness evaluation of the FLS model of care for hip fracture patients in Taiwan [104]. The FLS Group (n = 174) managed at the National Taiwan University Hospital were compared to propensity score-matched patients (n = 1697) from the National Health Insurance claim-based data who received usual care (UC Group). Based on a willingness-to-pay of US$65 per gross domestic product per day, the probability of the FLS being cost-effective exceeded 80%.
The Taiwanese Osteoporosis Association celebrates its 25th anniversary during 2022. Policy priorities this year include securing reimbursement from the National Health Insurance scheme for primary fracture prevention for individuals aged 75 years or over, those with a DXA T-Score of ≤ − 2.5 standard deviations relative to the young adult normal, and those with chronic conditions such as diabetes mellitus and rheumatoid arthritis.
As of August 2022, 31 hospitals from Taiwan feature on the IOF Capture the Fracture® Map of Best Practice [51].
Thailand
The so-called old-age dependency ratio is the ratio of the population aged 65 years or over to the population aged 15–64 years, who are considered to be of working age. In Fig. 1, these ratios are presented as the number of dependents per 100 persons of working age in Thailand for the period 1950 to 2100 [105]. This step-change in the age structure of the Thai population will result in an inevitable increase in the incidence of hip and other fragility fractures, in the absence of a systematic approach to prevention.
Old-age dependency ratio for Thailand for the period 1950 to 2100. From World Population Prospects: Volume II: Demographic Profiles 2017 Revision. ST/ESA/SER.A/400, by Department of Economic and Social Affairs, Population Division, ©2017 United Nations. Reprinted with the permission of the United Nations
In 2019, Sucharitpongpan et al. reported the incidence of hip fractures in Nan province (Northern part of Thailand) from 2015 to 2017 of approximately 211.6, 214.9 and 238.5 per 100,000 person-years, respectively [106]. In 2020, as noted in Table 2 previously, the same group of investigators reported that the 1-year mortality of fragility hip fracture was approximately 19% [28]. Compared with the age-matched population in Nan province, hip fractures increased the mortality rate by 6.2 times. This information highlights the importance of the hip fracture situation in Thailand and encourages each centre to develop an effective strategy for fracture prevention, as well as pathway development to improve post-hip fracture management.
In 2021, Sura-amonrattana et al. compared outcomes of hip fracture patients before and after implementation of the fast-track programme [107] at the Faculty of Medicine Siriraj Hospital and found that time to surgery and length of hospital stay were improved in the fast-track protocol; however, outcome benefits were not demonstrated. A stratified analysis by dementia status showed a trend in delirium reduction for all patients and a pressure injury reduction among those with dementia after the fast-track programme has been implemented, although the differences were not statistically significant.
As noted by Ebeling et al. [8], in 2018, the government of Thailand developed a policy to implement a nationwide secondary fracture prevention programme. This initiative was launched with the first Thailand FLS Forum and Workshop held in Bangkok. Subsequently, annual in-person meetings were held in 2019 and 2020. Due to the COVID-19 pandemic, the 2021 FLS Forum and Workshop was conducted via an online meeting platform. Since then, many hospitals in Thailand have implemented an FLS multidisciplinary team approach for secondary fracture prevention. As of August 2022, 17 Thai hospitals feature on the IOF Capture the Fracture® Map of Best Practice [51].
In 2020, Amphansap et al. described the effectiveness of the Police General Hospital’s FLS after 5 years of implementation [108]. The rate of osteoporosis assessment increased from 28.3% pre-implementation to 85.8% post-FLS implementation. In addition, the rate of osteoporosis treatment either with calcium and vitamin D alone or with an anti-osteoporosis agent was increased from 40.8 to 89.4% after FLS implementation.
In 2021, Chotiyarnwong et al. demonstrated that video-based osteoporosis education was equally effective to the traditional lecture-based education [109]. Since then, video-based osteoporosis education has been used as part of the investigators’ FLS to provide essential information about osteoporosis to both patients and caregivers.
In 2021, the Thai Osteoporosis Foundation revised and updated the Thai osteoporosis guidelines for assessment and management of osteoporosis [110]. This guideline was drafted and reviewed by osteoporosis experts from many specialties including orthopaedic surgeons, endocrinologists, rheumatologists, geriatricians, obstetricians and gynaecologists, physiatrists, physical nutrition specialists, radiologists and maxillofacial surgeons. The updated Thai osteoporosis guideline was then endorsed by a number of organisations including the Royal College of Orthopaedic Surgeons of Thailand, the Royal College of Physicians of Thailand, the Royal College of Physiatrists of Thailand, the Royal Thai College of Obstetricians and Gynaecologists and the Endocrine Society of Thailand.
The Decade of Healthy Ageing: Road Maps for countries in Asia Pacific
The approaches to quality improvement summarised in this review and the following bodies of work share many consistent themes that could inform development of national bone health improvement ‘Road Maps’ in countries across the Asia Pacific region.
As described previously, the Global Call to Action on Fragility Fractures [42] published in 2018 called for urgent improvements in the acute care, rehabilitation and secondary fracture prevention for individuals who sustain fragility fractures. The Call to Action also proposed formation of multidisciplinary national alliances to advocate with a unified voice to policymakers, to secure the financial resources needed to implement models of best clinical practice, at scale.
In 2019, IOF published the second edition of the IOF Compendium of Osteoporosis [10] that proposed nine key priorities for the period 2020 to 2025:
-
1.
Secondary fracture prevention
-
2.
Osteoporosis induced by medicines
-
3.
Primary fracture prevention
-
4.
Nutrition and exercise
-
5.
Healthcare professional education
-
6.
Public awareness and education
-
7.
Improving access and reimbursement for diagnosis and treatment
-
8.
Development of national hip fracture registries
-
9.
Formation of national falls and fracture prevention alliances
Since publication in 2017 of a report titled Demystifying ageing: Lifting the burden of fragility fractures and osteoporosis in Asia Pacific [111], the Economist Intelligence Unit has undertaken a body of work to explore challenges and solutions relating to improving bone health based on interviews with a broad range of stakeholders:
-
Ageing with strength: Addressing fragility fractures in Asia–Pacific (2019) [112]
-
Building alliances against osteoporosis and fragility fractures (2020) [113]
-
Integrated pathways for bone health: An overview of global policies (2021) [114]
In 2021, Bussell reviewed this work and proposed an approach to transform the agenda for bone health [115]. This was predicated on an integrated care pathway encompassing the following elements:
-
A lifespan approach encompassing primary and secondary care
-
Coordination and comprehensive care delivery and service offerings
-
Pharmacological and non-pharmacological approaches to improve bone health outcomes
-
Social determinants of health to inform strategies to improve bone health
In 2022, a case study in multidisciplinary, multisector, multinational collaboration describes quality improvement, advocacy and government agency engagement to transform the management of fragility fractures in New Zealand during the period 2012 to 2022 [116]. The strategy underpinning this decade-long approach is illustrated in Fig. 2.
A systematic approach to fragility fracture care and prevention for New Zealand [117]. Reproduced with kind permission of Osteoporosis New Zealand
A Delphi process [118] could be applied to engage a diverse group of stakeholders in each country to achieve consensus on priority themes for each national Road Map. A national evaluation of current levels of implementation of identified priorities, and preparedness to implement new priorities, could be undertaken in 2022 or 2023. A timeframe for measurement of quality improvement could be established, with a view to conduct interim national analyses in 2026 and 2030.
Conclusion and Call to Action on Fragility Fractures in Asia Pacific
As the demography of the population of the Asia Pacific region shifts rapidly in the coming decades, the already enormous burden imposed by osteoporosis and associated fragility fractures is set to increase substantially. There is a pressing need for governments across the region to embed the care and prevention of fragility fractures into national injury prevention strategies. While the COVID pandemic has disrupted the region and the world in ways unimaginable in late 2019, since the ‘time before COVID’, numerous initiatives to improve the care received by individuals who sustain fragility fractures have been established at the global level and regional level in Asia Pacific, and in many countries and hospitals across the region. This review provides a summary of recent progress that could inform development of national Road Maps to improve bone health for the populations served. The adage that ‘Failing to plan is planning to fail’ is apposite with respect to prevention of the serious and costly injuries that result from the most common bone disease in humans. As the Asia Pacific region is set to bear the brunt of the global burden of fragility fractures by mid-century, clear, measurable national action plans must be devised and implemented at scale throughout the United Nations ‘Decade of Healthy Ageing’ [3].
In 2018, the Global Call to Action on Fragility Fractures called upon diverse stakeholder sectors to undertake specific actions [42]. As the ageing of the population of the Asia Pacific region gains pace, the need for widespread implementation of these actions becomes increasingly urgent. Accordingly, we call upon governments, healthcare professional organisations and individual healthcare professionals in Asia Pacific to prioritise the following actions during the remainder of 2022 and beyond:
-
Governments:
-
To recognise and respond to the threat posed to their societies from fragility fractures
-
To prioritise acute and long-term fragility fracture care and prevention in National Health Strategies
-
To increase funding available to implement—at scale—proven models of care including Orthogeriatric Services and Fracture Liaison Services to improve outcomes for people with fragility fractures
-
-
Healthcare professional organisations:
-
To collaborate nationally and locally to form alliances to speak with a unified voice to policy makers
-
To produce consensus guidelines setting clear standards for adequate care using the best available research evidence, and propose metrics to evaluate performance
-
To expand education and research programmes that can establish best practice
-
-
Individual healthcare professionals:
-
To seek, create and follow evidence-based best practice
-
To form multidisciplinary teams with colleagues to identify and address the needs of people with fragility fractures
-
In day-to-day clinical practice, to participate in quality improvement programmes to continuously improve care provided to people with fragility fractures
-
Data availability
Not applicable.
Code availability
Not applicable.
Change history
05 September 2022
References are updated.
References
Wikipedia (2022) World population. https://en.wikipedia.org/wiki/World_population. Accessed 16 Aug 2022
Adam D (2021) How far will global population rise? Researchers can’t agree. Nature 597:462–465
World Health Organization (2020) The decade of healthy ageing: a new UN-wide initiative. https://www.who.int/news/item/14-12-2020-decade-of-healthy-ageing-a-new-un-wide-initiative. Accessed 16 Aug 2022
Worldometers.info (2022) Current world population. https://www.worldometers.info/world-population/. Accessed 16 Aug 2022
Wikipedia (2022) List of countries and dependencies by population. https://en.wikipedia.org/wiki/List_of_countries_and_dependencies_by_population. Accessed 16 Aug 2022
United Nations, Department of Economic and Social Affairs, Population Division (2017) World population prospects: the 2017 revision, volume I: comprehensive tables (ST/ESA/SER.A/399), New York. https://esa.un.org/unpd/wpp/Publications/Files/WPP2017_Volume-I_Comprehensive-Tables.pdf
Wu A-M, GBD 2019 Fracture Collaborators (2019) Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev 2:e580–e592
Ebeling PR, Chan DC, Lau TC, Lee JK, Songpatanasilp T, Wong SH, Hew FL, Sethi R, Williams M (2020) Secondary prevention of fragility fractures in Asia Pacific: an educational initiative. Osteoporos Int 31:805–826
Mitchell PJ, Magaziner J, Costa M, Seymour H, Marsh D, Falaschi P, Beaupre L, Tabu I, Eleuteri S, Close J, Agnusdei D, Speerin R, Kristensen MT, Lord S, Rizkallah M, Caeiro JR, Yang M (2020) FFN clinical toolkit, 1st edn. Fragility Fracture Network, Zurich. https://fragilityfracturenetwork.org/. Accessed 16 Aug 2022
Cooper C, Ferrari S, on behalf of the IOF Board and Executive Committee (Reginster JY, Chair of Committee of National Societies; Dawson-Hughes B, General Secretary; Rizzoli R, Treasurer; Kanis J, Honorary President; Halbout P, CEO) (2019) IOF compendium of osteoporosis. 2nd edition. Writer: Mitchell P. reviewers: Harvey N and Dennison E. International Osteoporosis Foundation, Nyons. https://www.osteoporosis.foundation/educational-hub/files/iof-compendium-osteoporosis-2nd-edition
Cheung CL, Ang SB, Chadha M et al (2018) An updated hip fracture projection in Asia: the Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia 4:16–21
Ong T, Khor HM, Kumar CS, Singh S, Chong E, Ganthel K, Lee JK (2020) The current and future challenges of hip fracture management in Malaysia. Malays Orthop J 14:16–21
Pandey D, Barakoti R, Upreti A, Hamal PK (2021) A retrospective look at fragility hip fractures in elderly. J Orthop Dis 4:1–3
Dare AJ, Hu G (2017) China’s evolving fracture burden. Lancet Glob Health 5:e736–e737
Tatangelo G, Watts J, Lim K et al (2019) The cost of osteoporosis, osteopenia, and associated fractures in Australia in 2017. J Bone Miner Res 34:616–625
Giummarra MJ, Ekegren CL, Gong J, Simpson P, Cameron PA, Edwards E, Gabbe BJ (2020) Twelve month mortality rates and independent living in people aged 65 years or older after isolated hip fracture: a prospective registry-based study. Injury 51:420–428
Lv H, Chen W, Zhang T et al (2020) Traumatic fractures in China from 2012 to 2014: a National Survey of 512,187 individuals. Osteoporos Int 31:2167–2178
Wang L, Yu W, Yin X et al (2021) Prevalence of osteoporosis and fracture in China: the China Osteoporosis Prevalence Study. JAMA Netw Open 4:e2121106
Wong RMY, Ho WT, Wai LS, Li W, Chau WW, Chow KS, Cheung WH (2019) Fragility fractures and imminent fracture risk in Hong Kong: one of the cities with longest life expectancies. Arch Osteoporos 14:104
Takusari E, Sakata K, Hashimoto T, Fukushima Y, Nakamura T, Orimo H (2021) Trends in hip fracture incidence in Japan: estimates based on nationwide hip fracture surveys from 1992 to 2017. JBMR Plus 5:e10428
Hagino H, Jackson M, Gitlin M, Wessler Z (2021) Estimating the future clinical and economic benefits of improving osteoporosis diagnosis and treatment among women in Japan: a simulation projection model from 2020 to 2040. Arch Osteoporos 16:156
Yong EL, Ganesan G, Kramer MS, Logan S, Lau TC, Cauley JA, Tan KB (2019) Hip fractures in Singapore: ethnic differences and temporal trends in the new millennium. Osteoporos Int 30:879–886
Chandran M, Lau TC, Gagnon-Arpin I, Dobrescu A, Li W, Leung MYM, Patil N, Zhao Z (2019) The health and economic burden of osteoporotic fractures in Singapore and the potential impact of increasing treatment rates through more pharmacological options. Arch Osteoporos 14:114
Yoo JI, Ha YC, Park KS, Kim RB, Seo SH, Koo KH (2019) Incidence and mortality of osteoporotic refractures in Korea according to Nationwide Claims Data. Yonsei Med J 60:969–975
Jackson M, Yang KH, Gitlin M, Wessler Z (2021) Estimating the future clinical and economic benefits of improving osteoporosis diagnosis and treatment among women in South Korea: a simulation projection model from 2020 to 2040. Arch Osteoporos 16:115
Abeygunasekara T, Lekamwasam S, Lenora J, Alwis G (2020) Current incidence and future projections of fragility hip fractures in Sri Lanka. Arch Osteoporos 15:178
Abeygunasekara T, Lekamwasam S, Alwis G, Lenora J (2020) Factors associated with one-year mortality of patients admitted with fragility hip fracture: a follow-up study in Southern Sri Lanka. Arch Osteoporos 15:95
Daraphongsataporn N, Saloa S, Sriruanthong K, Philawuth N, Waiwattana K, Chonyuen P, Pimolbutr K, Sucharitpongpan W (2020) One-year mortality rate after fragility hip fractures and associated risk in Nan, Thailand. Osteoporos Sarcopenia 6:65–70
Hoang DK, Doan MC, Mai LD, Ho-Le TP, Ho-Pham LT (2021) Burden of osteoporosis in Vietnam: an analysis of population risk. PLoS ONE 16:e0252592
Australian and New Zealand Hip Fracture Registry (2022) Australian and New Zealand hip fracture registry website. http://www.anzhfr.org/. Accessed 16 Aug 2022
Australian Commission on Safety and Quality in Health Care, Health Quality & Safety Commission New Zealand (2016) Hip fracture care clinical care standard. https://www.safetyandquality.gov.au/standards/clinical-care-standards/hip-fracture-care-clinical-care-standard. Accessed 16 Aug 2022
ANZHFR Annual Report of Hip Fracture Care (2021) Australian and New Zealand Hip Fracture Registry, Sydney. https://anzhfr.org/registry-reports/. Accessed 16 Aug 2022
Australian and New Zealand Hip Fracture Registry (2022) Bone medication protection: ANZHFR sprint audit (2021). https://anzhfr.org/sprintaudits/. Accessed 16 Aug 2022
Australian Fragility Fracture Foundation (2022) Australian fragility fracture registry website. https://fragilityfracture.com.au/. Accessed 16 Aug 2022
Australian and New Zealand Fragility Fracture Registry Steering Group (2022) New Zealand fragility fracture registry website. https://fragilityfracture.co.nz. Accessed 16 Aug 2022
Wang X, Li C, He Y, Wang T, Zhang H, Ma Z, Ma H, Zhao H (2020) Anti-osteoporosis medication treatment pattern after osteoporotic fracture during 2010–2016 in Fujian. China Arch Osteoporos 15:134
Shimodan S, Sato D, Takahashi K et al (2020) Ten years change in post-fracture care for hip fracture patients. J Bone Miner Metab 38:222–229
Hagino H, Wada T (2019) Osteoporosis liaison service in Japan. Osteoporos Sarcopenia 5:65–68
Nakatoh S, Fujimori K, Ishii S, Tamaki J, Okimoto N, Ogawa S, Iki M (2021) Insufficient increase in bone mineral density testing rates and pharmacotherapy after hip and vertebral fracture: analysis of the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Arch Osteoporos 16:130
Chau YT, Nashi N, Law LS, Goh RKH, Choo SX, Seetharaman SK (2020) Undertreatment of osteoporosis following hip fracture: a retrospective, observational study in Singapore. Arch Osteoporos 15:141
Kim DG, Seo GW, Nam HW (2019) Trends in the diagnosis of osteoporosis in patients with distal radius fractures based on a National Claims Database. J Bone Metab 26:247–252
Dreinhofer KE, Mitchell PJ, Begue T et al (2018) A global call to action to improve the care of people with fragility fractures. Injury 49:1393–1397
Marsh D, Mitchell PJ, Falaschi P et al (2020) Orthogeriatrics: the management of older patients with fragility fractures. Springer International Publishing, Cham, Switzerland
van Oostwaard M, Marques A, Queirós C et al (2018) In: Hertz K, Santy-Tomlinson J (eds) Fragility fracture nursing - holistic care and management of the orthogeriatric patient. Springer International Publishing AG, Cham. https://www.springer.com/gp/book/9783319766805
Geirsdóttir OG, Hertz K, Santy-Tomlinson J et al (2021) Interdisciplinary nutritional management and care for older adults - an evidence-based practical guide for nurses. In: Geirsdóttir OG, Bell J (eds). Springer International Publishing AG, Cham. https://link.springer.com/book/10.1007/978-3-030-63892-4. Accessed 16 Aug 2022
Tate J, Harding E, Krishnaswamy P, Rizkallah M, Caeiro JR, Yang M (2020) FFN policy toolkit. 1st Edition. Fragility fracture network, Zurich. https://fragilityfracturenetwork.org/. Accessed 16 Aug 2022
Akesson K, Mitchell PJ (2012) In: Stenmark J, Misteli L (eds) Capture the fracture: a global campaign to break the fragility fracture cycle. Reviewers: Marsh D, Cooper C, Edwards M, Harvey N. International Osteoporosis Foundation, Nyons. https://www.osteoporosis.foundation/sites/iofbonehealth/files/2019-06/2012_CaptureTheFracture_ThematicReport_English.pdf
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C, Group IOFFW (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152
Javaid MK, Sami A, Lems W et al (2020) A patient-level key performance indicator set to measure the effectiveness of fracture liaison services and guide quality improvement: a position paper of the IOF Capture the Fracture Working Group, National Osteoporosis Foundation and Fragility Fracture Network. Osteoporos Int 31:1193–1204
International Osteoporosis Foundation (2022) Capture the fracture® partnership. https://www.osteoporosis.foundation/capture-the-fracture. Accessed 16 Aug 2022
International Osteoporosis Foundation (2022) IOF capture the fracture® map of best practice. https://www.capturethefracture.org/map-of-best-practice
Asia Pacific Fragility Fracture Alliance (2022) Asia Pacific fragility fracture Alliance website. http://www.apfracturealliance.org/. Accessed 16 Aug 2022
Close JC, Seymour H, Mitchell PJ, Ahern E, Costa M, Magaziner J, Lee JK, Chan D-C, Ang SB, Mercado-Asis LB, Flicker L, Leung E, Choon D, Kumar CSK, Rey-Matias R, Chen W-S, Halbout P, Cooper C, Blank RD, Zhao Y, on behalf of the Asia Pacific Fragility Fracture Alliance and the Fragility Fracture Network (2021) Hip fracture registry toolbox - a collaboration between the APFFA hip fracture registry working group and the FFN hip fracture audit special interest group. Asia Pacific fragility fracture Alliance. In: Lee JK, Chan D-C (eds). Asia Pacific Orthopaedic Association, Kuala Lumpur. https://apfracturealliance.org/hfr-toolbox/. Accessed 16 Aug 2022
Asia Pacific Fragility Fracture Alliance (2020) Primary care physician education toolkit. Asia Pacific fragility fracture Alliance, Kuala Lumpur. https://apfracturealliance.org/education-toolkit/. Accessed 16 Aug 2022
Asia Pacific Fragility Fracture Alliance (2022) Education Directory. https://apfracturealliance.org/education-directory/. Accessed 16 Aug 2022
Asia Pacific Orthopaedic Association (2022) Asia Pacific Orthopaedic Association website. https://www.apoaonline.com/. Accessed 16 Aug 2022
Lee JK, Ebeling P, Hagino H, Songpatanasilp T, Choon DS-W, Korskusuz F, Leung F, Theis J-C (2021) Closing the gap between orthopaedic surgeons and physicians in secondary fracture prevention - a call to action: an Asia-Pacific initiative from the international Osteoporosis Foundation and Asia Pacific Orthopaedic association. Reviewers: Lee JK, Choon DS-W, Pierroz DD, Ferrari S, Harvey N, Halbout P, Cooper C. International Osteoporosis Foundation - Asia Pacific Orthopaedic Association, Nyons and Kuala Lumpur. https://www.apoaonline.com/pdf/apoa-brochure.pdf. Accessed 16 Aug 2022
Asia Pacific Orthopaedic Association (2022) Asia Pacific osteoporosis and fragility fracture society website. https://www.apoaonline.com/asia-pacific-osteoporosis-fragility-fracture-society.php. Accessed 16 Aug 2022
Asia Pacific Orthopaedic Association (2022) Asia Pacific Trauma Society website. https://www.apoaonline.com/trauma-section.php. Accessed 16 Aug 2022
Asia Pacific Consortium on Osteoporosis (2022) Asia Pacific consortium on osteoporosis website. https://apcobonehealth.org/. Accessed 16 Aug 2022
Chandran M, Mitchell PJ, Amphansap T et al (2021) Development of the Asia Pacific Consortium on Osteoporosis (APCO) Framework: clinical standards of care for the screening, diagnosis, and management of osteoporosis in the Asia-Pacific region. Osteoporos Int 32:1249–1275
Gallacher SJ, Alexander S, Beswetherick N et al (2019) Effective secondary prevention of fragility fractures: clinical standards for fracture liaison services. Royal Osteoporosis Society, Camerton
Arai H, Ikeda S, Okuro M et al (2019) Clinical Standards for Fracture Liaison Services (FLS) in Japan. Japan Osteoporosis Society and FFN Japan, Tokyo
Fergusson K, Gill C, Harris R, Kim D, Mackenzie D, Mitchell PJ, Ward N (2021) Clinical standards for fracture liaison Services in New Zealand. 2nd Edition. Osteoporosis New Zealand, Wellington. https://osteoporosis.org.nz/wp-content/uploads/ONZ-FLS-Clinical-Standards-Sept-2021-1.pdf. Accessed 16 Aug 2022
Asia Pacific Consortium on Osteoporosis (2021) The APCO HCP peer to peer education modules. https://apcobonehealth.org/apco-education-modules/. Accessed 16 Aug 2022
Australian Government Department of Health (2019) National strategic action plan for osteoporosis October 2019. https://www.health.gov.au/resources/publications/national-strategic-action-plan-for-osteoporosis-2019. Accessed 16 Aug 2022
SOS Fracture Alliance (2022) SOS Fracture Alliance website. https://www.sosfracturealliance.org.au/. Accessed 16 Aug 2022
Osteoporosis New Zealand (2022) Osteoporosis New Zealand website. https://osteoporosis.org.nz/. Accessed 16 Aug 2022
Accident Compensation Corporation (2021) Preventing fragility fractures web page. https://www.acc.co.nz/newsroom/stories/preventing-fragility-fractures/. Accessed 16 Aug 2022
Accident Compensation Corporation, Ministry of Health, Health Quality & Safety Commission New Zealand, New Zealand Government (2022) Live stronger for longer - prevent falls and fractures website. http://livestronger.org.nz/. Accessed 16 Aug 2022
Tian M (2021) Injury prevention sessions - developing better care for older hip fracture patients in China. The George Institute for Global Health. https://www.georgeinstitute.org/events/injury-prevention-sessions-developing-better-care-for-older-hip-fracture-patients-in-china
Tian M, Gong X, Rath S, Wei J, Yan LL, Lamb SE, Lindley RI, Sherrington C, Willett K, Norton R (2016) Management of hip fractures in older people in Beijing: a retrospective audit and comparison with evidence-based guidelines and practice in the UK. Osteoporos Int 27:677–681
Wu X, Tian M, Zhang J et al (2019) The effect of a multidisciplinary co-management program for the older hip fracture patients in Beijing: a “pre- and post-” retrospective study. Arch Osteoporos 14:43
Peng K, Liu H, Zhang J, Yang M, Liu Y, Tian M, Chu H, Wu X, Ivers R (2020) Applying normalization process theory and process mapping to understand implementation of a co-management program for older hip fracture patients in China: a qualitative study. Arch Osteoporos 15:92
Peng K, Yang M, Tian M, Chen M, Zhang J, Wu X, Ivers R, Si L (2020) Cost-effectiveness of a multidisciplinary comanagement program for the older hip fracture patients in Beijing. Osteoporos Int 31(8):1545–1553
Zhang J, Yang M, Zhang X et al (2022) The effectiveness of a co-management care model on older hip fracture patients in China – a multicentre non-randomised controlled study. Lancet Region Health - Western Pacific 19:100348
National Health Commission of the People’s Republic of China (2022) National Health Commission of the People’s Republic of China website. http://en.nhc.gov.cn/. Accessed 16 Aug 2022
Australian and New Zealand Hip Fracture Registry (ANZHFR) Steering Group (2014) Australian and New Zealand Guideline for Hip Fracture Care: improving outcomes in hip fracture management of adults. Australian and New Zealand Hip Fracture Registry Steering Group, Sydney
Scottish Government (2020) Scottish standards of care for hip fracture patients. Scottish Government, Edinburgh. https://www.shfa.scot.nhs.uk/_docs/2020/Scottish-standards-of-care-for-hip-fracture-patients-2020.pdf
National Institute for Health and Care Excellence (2017) Hip fracture: management - Clinical guideline [CG124]. National Institute for Health and Care Excellence, London. https://www.nice.org.uk/guidance/cg124
Roberts KC, Brox WT (2015) AAOS Clinical Practice Guideline: management of hip fractures in the elderly. J Am Acad Orthop Surg 23:138–140
Wong RMY, Qin J, Chau WW, Tang N, Tso CY, Wong HW, Chow SK, Leung KS, Cheung WH (2021) Prognostic factors related to ambulation deterioration after 1-year of geriatric hip fracture in a Chinese population. Sci Rep 11:14650
Wong RMY, Law SW, Lee KB, Chow SKH, Cheung WH (2019) Secondary prevention of fragility fractures: instrumental role of a fracture liaison service to tackle the risk of imminent fracture. Hong Kong Med J 25:235–242
Wong RMY, Ko SY, Chau W-W, Lee LCY, Chow SKH, Cheung WH, Law SW (2021) The first reported fracture liaison service (FLS) for vertebral fractures in China: is muscle the missing gap? Arch Osteoporos 16:168
Shigemoto K, Sawaguchi T, Goshima K, Iwai S, Nakanishi A, Ueoka K (2019) The effect of a multidisciplinary approach on geriatric hip fractures in Japan. J Orthop Sci 24:280–285
Shigemoto K, Sawaguchi T, Horii T, Goshima K, Iwai S, Higashikawa T, Okuro M (2021) Multidisciplinary care model for geriatric patients with hip fracture in Japan: 5-year experience. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03933-w
Hagino H, Endo N, Harada A, Iwamoto J, Mashiba T, Mori S, Ohtori S, Sakai A, Takada J, Yamamoto T (2017) Survey of hip fractures in Japan: recent trends in prevalence and treatment. J Orthop Sci 22:909–914
Hagino H (2021) Current and future burden of hip and vertebral fractures in Asia. Yonago Acta Med 64:147–154
Ministry of Health Labour and Welfare (2022) Ministry of health labour and welfare website. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000188411_00037.html. Accessed 16 Aug 2022
Fragility Fracture Network Malaysia (2022) Fragility fracture network Malaysia website. https://ffnmalaysia.wixsite.com/ffnm. Accessed 16 Aug 2022
Malaysian Orthopaedic Association (2022) Greying gracefully: the new paradigm for orthopaedics in an ageing population – 51st Malaysian Orthopaedic Association Annual Scientific Meeting 9th–11th June 2022 website. https://moaasm.com/. Accessed 16 Aug 2022
International Osteoporosis Foundation (2022) Capture the fracture® program website. https://www.capturethefracture.org/. Accessed 16 Aug 2022
Reyes PVSJ, Tabu IA, Sandoval MAS, Mangubat AAS, Bing-Agsaoay DDC (2021) Does adopting a multidisciplinary approach in the management of acute hip fractures in orthopedic geriatric patients lead to better outcomes? A Preliminary Report of the University of the Philippines - Philippine General Hospital (UP-PGH) Orthogeriatric Multidisciplinary Fracture Management Model and Fracture Liaison Service. Acta Med Philipp 55:1–7
Cortez KA, Lai JGL, Tabu IA (2021) Economic burden and the effects of early versus delayed hospitalization on the treatment cost of patients with acute fragility hip fractures under the UPM-PGH Orthogeriatric Multidisciplinary Fracture Management Model and Fracture Liaison Service. Osteoporos Sarcopenia 7:63–68
Ebeling P, Chan D-C, Lau TC, Lee JK, Songpatanasilp T, Wong SH, Hew FL, Sethi R, Williams M (2020) Secondary prevention of fragility fractures in Asia Pacific: an educational initiative. Osteoporos Int 31(5):805–826
British Orthopaedic Association, British Geriatrics Society (2007) The care of patients with fragility fracture, 2nd edn. British Orthopaedic Association, London. https://www.bgs.org.uk/resources/care-of-patients-with-fragility-fracture-blue-book
Cha YH, Ha Y-C, Lim J-Y (2019) Establishment of Fracture Liaison Service in Korea: where is it stand and where is it going? J Bone Metabolism 26:207–211
Min K, Beom J, Kim BR et al (2021) Clinical Practice Guideline for Postoperative Rehabilitation in Older Patients With Hip Fractures. Ann Rehabil Med 45:225–259
Yoo J-I, Kim H-Y, Jang S, Lee Y-K, Ha Y-C (2020) Risk factors for subsequent hip fractures and fatality after an initial hip fracture in Korea: using nationwide claims data. Arch Osteoporos 15:165
Shim YB, Park JA, Nam JH, Hong SH, Kim JW, Jeong J, Shin JY (2020) Incidence and risk factors of subsequent osteoporotic fracture: a nationwide cohort study in South Korea. Arch Osteoporos 15:180
Hsu CL, Chen HM, Chen HJ, Chou MY, Wang YC, Hsu YH, Liang CK, Chu CS (2020) A national study on long-term osteoporosis therapy and risk of recurrent fractures in patients with hip fracture. Arch Gerontol Geriatr 88:104021
Huang CF, Pan PJ, Chiang YH, Yang SH (2021) A rehabilitation-based multidisciplinary care model reduces hip fracture mortality in older adults. J Multidiscip Healthc 14:2741–2747
Chang CB, Yang RS, Chang LY, Peng JK, Tsai KS, Huang WJ, Yang TH, Chan DC (2021) One-year outcomes of an osteoporosis liaison services program initiated within a healthcare system. Osteoporos Int 32(11):2163–2172
Chien LN, Li YF, Yang RS, Yang TH, Chen YH, Huang WJ, Tsai HY, Li CY, Chan DC (2021) Real-world cost-effectiveness analysis of the fracture liaison services model of care for hip fracture in Taiwan. J Formos Med Assoc 121(1(Pt 2)):425–433
United Nations, Department of Economic and Social Affairs, Population Division (2017) World population prospects: the 2017 revision, volume II: demographic profiles 2017 (ST/ESA/SER.A/400), New York. https://population.un.org/wpp/Publications/Files/WPP2017_Volume-II-Demographic-Profiles.pdf
Sucharitpongpan W, Daraphongsataporn N, Saloa S, Philawuth N, Chonyuen P, Sriruanthong K, Waiwattana K (2019) Epidemiology of fragility hip fractures in Nan, Thailand. Osteoporos Sarcopenia 5:19–22
Sura-Amonrattana U, Tharmviboonsri T, Unnanuntana A, Tantigate D, Srinonprasert V (2021) Evaluation of the implementation of multidisciplinary fast-track program for acute geriatric hip fractures at a University Hospital in resource-limited settings. BMC Geriatr 21:548
Amphansap T, Stitkitti N, Arirachakaran A (2020) The effectiveness of Police General Hospital’s fracture liaison service (PGH’s FLS) implementation after 5 years: a prospective cohort study. Osteoporos Sarcopenia 6:199–204
Chotiyarnwong P, Boonnasa W, Chotiyarnwong C, Unnanuntana A (2021) Video-based learning versus traditional lecture-based learning for osteoporosis education: a randomized controlled trial. Aging Clin Exp Res 33:125–131
Thai Osteoporosis Foundation (2021) Clinical practice guideline on management of osteoporosis 2021. Thai Osteoporosis Foundation, Bangkok
Kielstra P (2017) In: Gold M (ed) Demystifying ageing - lifting the burden of fragility fractures and osteoporosis in Asia Pacific. Economist Intelligence Unit, London. https://impact.economist.com/perspectives/sites/default/files/Demystifying_ageing_Lifting_the_burden_of_fragility_fractures_and_osteoporosis_in_Asia_Pacific.pdf
Murray S (2019) In: Dalai R, Gold M, Kielstra P (eds) Ageing with strength - addressing fragility fractures in Asia-Pacific. Economist Intelligence Unit, London. https://impact.economist.com/perspectives/sites/default/files/ageing_with_strength.pdf
Economist Intelligence Unit (2020) Building alliances against osteoporosis and fragility fractures. Economist Intelligence Unit, London. https://impact.economist.com/perspectives/sites/default/files/eco114_building_alliances_osteoporosis_fractures_1_4.pdf
Puhl T, Bussell M (2021) In: Clapton J (ed) Integrated pathways for bone health - an overview of global policies. Economist Intelligence Unit Healthcare, London. https://impact.economist.com/perspectives/sites/default/files/eiu_amgen_bone_health_global_policy_overview_final_2021_3_5.pdf
Bussell ME (2021) Improving bone health: addressing the burden through an integrated approach. Aging Clin Exp Res 33:2777–2786
Gill CE, Mitchell PJ, Clark J et al (2022) Experience of a systematic approach to care and prevention of fragility fractures in New Zealand. Arch Osteoporos 17(1):108–117
Osteoporosis New Zealand (2012) Bone care 2020 - a systematic approach to hip fracture care and prevention for New Zealand. Osteoporosis New Zealand, Wellington. https://osteoporosis.org.nz/wp-content/uploads/Bone-Care-2020-web.pdf
Wikipedia (2022) Delphi method web page. https://en.wikipedia.org/wiki/Delphi_method. Accessed 16 Aug 2022
Acknowledgements
The authors express their sincere thanks to the numerous investigators whose work has been summarised in this review. The Asia Pacific Orthopaedic Association received sponsorship from Amgen Asia to support the activities of the Asia Pacific Fragility Fracture Alliance (APFFA). This publication was drafted independently by APFFA.
Funding
The Asia Pacific Orthopaedic Association received sponsorship from Amgen Asia to support the activities of the Asia Pacific Fragility Fracture Alliance (APFFA). This publication was drafted independently by APFFA.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Adjunct Associate Professor Paul James Mitchell (PJM) has undertaken consultancy for governments, national and international osteoporosis societies, healthcare professional organisations and private sector companies relating to systematic approaches to fragility fracture care, and prevention since 2005. PJM is a paid consultant and project manager for the Asia Pacific Fragility Fracture Alliance. Adjunct Assistant Professor Seng Bin Ang has no disclosures relating to this work. Professor Leilani Basa Mercado-Asis reports no conflicts of interest. Professor Reynaldo Rey-Matias has no disclosures relating to this work. Professor Wen-Shiang Chen has no disclosures relating to this work. Professor Leon Flicker reports no conflicts of interest. Dr. Edward Leung has no disclosures relating to this work. Professor David Choon has no disclosures relating to this work. Dr. Sankara Kumar Chandrasekaran has no disclosures relating to this work. Professor Jacqueline Clare Therese Close has no disclosures relating to this work. Dr. Hannah Seymour has no disclosures relating to this work. Professor Cyrus Cooper has received consulting fees and honoraria from Amgen, Danone, Eli Lilly, GSK, Medtronic, Merck, Nestle, Novartis, Pfizer, Roche, Servier, Shire, Takeda and UCB. Dr. Philippe Halbout is the Chief Executive Officer of the International Osteoporosis Foundation and has no disclosures relating to this work. Professor Robert Daniel Blank: Consulting, Bristol Myers Squibb; advisory board, Amgen; ownership, Abbott Labs, Abbvie, Amgen, JangoBio, Procter & Gamble; editorial stipend, Elsevier; authorship royalties, Wolters Kluwer. Dr. Yanling Zhao reports no conflicts of interest. Professor Jae-Young Lim reports no disclosures relating to this work. Associate Professor Irewin Tabu reports no disclosures relating to this work. Professor Maoyi Tian reports no conflicts of interest. Professor Aasis Unnanuntana has no disclosures relating to this work. Assistant Professor Ronald Man Yeung Wong has no disclosures relating to this work. Professor Noriaki Yamamoto has no disclosures relating to this work. Professor Ding-Chen (Derrick) Chan reports personal fees (consulting fees) from Amgen, Lotus, Eli-Lilly and Harvester Trading Co, Ltd. Dato’ Dr. Joon Kiong Lee has received honoraria from Amgen, Mylan, and Zuellig Pharma for speaking at symposia, as member of advisory board and educational programmes and workshops.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ding-Cheng (Derrick) Chan and Joon Kiong Lee are co-corresponding authors.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mitchell, P.J., Ang, S.B., Mercado-Asis, L.B. et al. Quality improvement initiatives in the care and prevention of fragility fractures in the Asia Pacific region. Arch Osteoporos 17, 115 (2022). https://doi.org/10.1007/s11657-022-01153-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-022-01153-2