Abstract
Summary
This systematic review identified patients have unmet information needs about the nature of osteoporosis, medication, self-management and follow-up. Clinician knowledge and attitudes appear to be of key importance in determining whether these needs are met. Unmet information needs appear to have psychosocial consequences and result in poor treatment adherence.
Purpose
Patient education is an integral component of the management of osteoporosis, yet patients are dissatisfied with the information they receive and see this as an area of research priority. This study aimed to describe and summarise the specific expressed information needs of patients in previously published qualitative research.
Methods
Using terms relating to osteoporosis, fragility fracture and information needs, seven databases were searched. Articles were screened using predefined inclusion and exclusion criteria. Full-text articles selected for inclusion underwent data extraction and quality appraisal. Findings were drawn together using narrative synthesis.
Results
The search identified 11,024 articles. Sixteen empirical studies were included in the review. Thematic analysis revealed three overarching themes relating to specific information needs, factors influencing whether information needs are met and the impact of unmet information needs. Specific information needs identified included the following: the nature of osteoporosis/fracture risk; medication; self-management and understanding the role of dual energy x-ray absorptiometry and follow-up. Perceived physician knowledge and attitudes, and the attitudes, beliefs and behaviours of patients were important factors in influencing whether information needs were met, in addition to contextual factors and the format of educational resources. Failure to elicit and address information needs appears to be associated with poor treatment adherence, deterioration of the doctor-patient relationship and important psychosocial consequences.
Conclusion
This is the first study to describe the information needs of patients with osteoporosis and fracture, the impact of this information gap and possible solutions. Further research is needed to co-design and evaluate educational interventions with patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
UK government policy places emphasis on providing patients with good quality health information, in order to encourage patient participation in healthcare and ensure that patients have greater power, protection and choice in key aspects of their care [1]. As well as promoting patient-centred care, this policy is an important driver in the management of health resources, achieved through emphasis of the importance of self-management. Especially in the context of an ageing population, and with increasing prevalence of long-term conditions such as osteoporosis, a strategy is needed whereby patients accept more responsibility for managing their own conditions which in turn will reduce or thwart the increase in demand on healthcare resources.
Patient information is a key component of effective self-management [2] and specifically in relation to osteoporosis and fracture prevention, information and education interventions have been shown to improve outcomes including health-directed behaviours and positive and active engagement in life, skill and technique acquisition, and social integration and support [3]. Patient education centres on the assumption that patients who are better informed about their condition and management will be more likely to adopt positive health behaviours [4] and will therefore improve, maintain or slow deterioration of their health status [5]. However, this viewpoint of patient education does not acknowledge the role of patient opinions and choice and implies that health professionals set the education agenda and define optimal health behaviours [6].
Patients are often dissatisfied with the information they receive from health professionals. A recent national survey of 1088 supporters of the National Osteoporosis Society (NOS) rated ‘easy access to information from health professionals’ as the number one research priority for osteoporosis and fracture out of 40 domains [7]. The focus groups that preceded this survey emphasised the importance, yet the relative lack, of information given by healthcare professionals early on in the participant’s pathway, e.g. at time of diagnosis, and in ongoing consultations with primary care clinicians [8].
To date, studies that have attempted educational needs assessment in osteoporosis have done so by measuring patient knowledge and inferring educational unmet need based on inaccurate answers to factual surveys [9,10,11]. These surveys tell us nothing about what patients want to know. Furthermore, quantitative methods fail to capture the context which underlies the reported needs of patients; qualitative research methods facilitate the in depth understanding of the thoughts and perceptions that underlie and influence information needs of patients, facilitating informed approaches to target unmet need [7]. The aim of this study was therefore to describe and summarise patient expressed information needs in previously published qualitative research, to better understand the research agenda relating to information needs of patients with osteoporosis and/or fractures [7].
Methods
Literature search
The review was conducted based on a pre-established protocol (detailed eligibility criteria are presented in Table 1, and search terms and search strategy in supplementary material 1). A systematic search for qualitative studies on expressed information needs of patients with osteoporosis/fragility fracture was conducted in seven databases: Medline, EMBASE, PsychINFO, Web of science, CINAHL, HMIC and AMED from the start of each database to July 2016. De-duplication of citations and title screening were completed by JJ and GR. Screening of abstracts against eligibility criteria and subsequent full-text reviews were independently completed by pairs of reviewers (GR and either ZP or OB). Grey literature was sought by hand searching reference lists of included studies and those that satisfied most, but not all of the review’s eligibility criteria. Citation tracking of included studies was also conducted in Google Scholar. Disagreements regarding study eligibility were resolved via discussion until consensus is achieved by the team.
Quality assessment
Eligible studies were independently appraised by pairs of reviewers (GR, AE and OB). Two tools were combined to support this (Supplementary Material 2). Firstly, the Hawker tool [12] was used to assess quality of the included studies as it can be used to evaluate qualitative research studies using different approaches. This tool includes nine domains (title/abstract; introduction/aims; methods/data; sampling; analysis; ethics/bias; results; transferability; usefulness). However, the Critical Appraisal Skills Programme tool for qualitative research was also used to further inform the appraisal of each article as this tool provided more detail about specific methodological issues relating to qualitative research [13]. For each study, individual items on the Hawker tool were judged as good, fair, poor or very poor. Variations in judgements regarding methodological appraisal of the quality of each studies were resolved through discussion with a third reviewer (ZP). No paper was excluded based on quality scores; it has been argued that excluding studies on the basis of quality criteria may exclude insightful studies [14]. However, study quality was considered during the synthesis stage to ensure themes were primarily based on the good or fair quality studies.
Data extraction
Using a customised data extraction form, information relating to author, title, date, country of origin, research question, method, sample and setting, year of publication, author’s findings and conclusions, from each study, was extracted. Extracted data was checked for consistency and accuracy.
Synthesis
Extracted data was tabulated and a thematic analysis was conducted. Findings relevant to our review objectives were grouped under the following headings:
-
Expressed information needs, i.e. where patient participant(s) was/were described as wanting to know more
-
Expressions of uncertainty, i.e. where patient participant(s) was/were described as being confused or unsure
-
Findings describing examples where information was given and was helpful
-
Inferred information needs (i.e. where authors deduce a need based on tested or assumed knowledge rather than patients expressing a need directly)
-
Anything else of relevance to giving and receiving of information
Inferred information needs were not included in subsequent stages of the analysis as it did not relate to our research question. We conducted thematic analysis on the data extracted, manually. The first stage was initially descriptive—to identify a taxonomy or classification of the types of information needs identified. Study quality was considered within each theme to ensure themes were not only informed by poor or very poor quality studies. Subsequently, a more interpretative level of coding was applied to explore and determine explanations for initial findings. Next, we revisited the original study findings to ensure our themes represented all the relevant findings. A higher level of abstraction was achieved by grouping subthemes into overarching themes, following an iterative mapping process and team discussions (ZP, GR, OB), through which a conceptual framework was developed.
Results
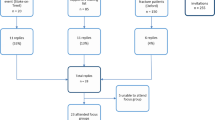
Eleven thousand seven unique citations were identified by the initial search and a further 17 by reference and citation checking. The review process and study flow is presented in Fig. 1. Sixteen studies were included for data extraction and quality appraisal.
Summary of included studies
The characteristics of the included studies are summarised in Table 2, including research question, country of origin and methods. Eleven studies utilised single semi-structured interviews [15, 17, 20,21,22,23, 25, 27,28,29,30] and focus groups were used as method in the remainder [16, 18, 19, 24, 26]. Eleven of the 16 included studies recruited patients from secondary care populations [15,16,17,18, 22,23,24,25,26, 29, 30], with the rest recruiting from primary care [20, 27], community or mixed settings [19, 21, 28]. Three studies included patients with specific fracture types (two hip and one vertebral) [22, 28, 30], and in these the research question and information needs related to the specific fracture care in addition to general issues pertaining to osteoporosis [22, 28, 30]. Seven studies were primarily concerned with attitudes and perceptions regarding medication or supplements [15,16,17,18,19,20, 27], with the others focused on experience of living with the condition more generally. Only three studies had research questions that were directly related to information needs [23, 25, 28]. One study aimed to explore knowledge after an education programme; although this was not directly relevant to our research question, the qualitative approach used did elicit directly expressed information needs [26]. For the remainder studies, only a small proportion of the total findings relating to information needs were relevant to our research question and extracted.
Summary of findings relating to quality appraisal
The findings related to quality appraisal are summarised in Table 3. Individual scores for quality appraisal by authors GR, AE and OB were congruent in 115/144 (79.9%) domains. Nine studies were scored as ‘fair’ or ‘good’ in all domains [15, 17, 19,20,21,22, 24, 25, 27]. Studies scoring ‘poor’ or ‘very poor’ did so in domains relating to sampling, ethics and bias, analysis, results, transferability and implications. The most common limitation of the included studies was failure to adequately describe the characteristics of the participants. For example, age was discussed regarding eligibility criteria, but the ages of included participants were not included [26, 28]. Limitations of the sampling or recruitment also affected the transferability and implications of the findings [26].
Main findings
The main findings are summarised in Table 4. Of the 16 included studies, 13 discussed directly expressed information needs and 12 studies discussed uncertainties. Thematic analysis of the findings revealed three overarching themes discussed individually below, and displayed in the conceptual framework in Fig. 2.
Specific information needs
Information needs were illustrated in all of the studies. The needs related to some or all of the following: the nature of osteoporosis and fracture risk; medication; self-management and/or the role of dual-energy X-ray absorptiometry (DXA) and follow up.
The nature of osteoporosis and fracture risk
The relationship between osteoporosis and age was a topic of uncertainty, causing some to question the need for medication for a condition that maybe considered normal for age [25, 27]. Doubt was expressed that osteoporosis was asymptomatic with participants in one study attributing a range of symptoms to the condition including pain, rotting teeth and flaking nails [15]. Findings from a further focus group study suggested that participants felt musculoskeletal pain experienced on activity was a signal of an imminent fracture [26]. Participants sampled from a study of screening for osteoporosis described uncertainty regarding communication of fracture risk, leading some to question the validity of the assessment [27]. The prognosis of osteoporosis, and the seriousness of osteoporosis, was a cause of uncertainty, which resulted in fear of the future [15, 30]. In a similar vein, patients recovering from hip fracture wanted to know in more detail what recovery would like and what the key ‘milestones’ would be [28].
Medication
Uncertainty about the purpose of medication was described in several studies [15, 18,19,20] and half of the participants in the interviews reported in a study published in 2012 had not considered that medication would reduce fracture risk [15]. In one study, a participant described a perception that bisphosphonates would reduce risk of falls [27]. One study focused on views on medication, participants described wanting to know more about the ‘pros’ of treatment [20]. Information regarding medications was described as too complex to understand [15]. Participants wanted more information on how to take bisphosphonates [18, 19], and in two studies, participants stated that they wanted to understand the reasons why there were specific instructions on how to take bisphosphonate medication [15, 20]. Men described wanting to know what medication was specifically suitable for them [29].
Sale et al. reported that some participants confused their bisphosphonate medication with their supplements [26]. Participants expressed a lack of guidance regarding recommended supplements [23], and the correct dose, explaining they were conflicted when choosing different sources of information to follow [26].
Self-management
A recurrent theme across seven studies in patients with osteoporosis was the expressed view that consultations contained too much of a focus on pharmacological interventions, with advice for other non-pharmacological management, e.g. diet and exercise being relatively neglected [15, 19,20,21,22, 26, 28]. In particular, the aim of one study was to explore the level of perceived support for physical activity and supplements given by participants’ general practitioners (GPs) [21]. Many participants in this study felt their needs relating to self-management were better met by the NOS charity rather than within the DXA consultation [21]. Participants felt unsure with regard to the type and duration of activity they should be doing to help osteoporosis generally [21]. In terms of fracture recovery, patients with hip fracture described that physiotherapists were good at explaining the purpose of exercises and which exercises to do [22]. Patients valued information on mobilisation and exercise programmes [28] and particularly valued feedback on their individual progress [22]. In contrast, in a study of women’s experiences of living with vertebral fractures, participants did not feel they were given any advice on self-care, with the exception of pain relief and advice to rest, which resulted in feelings of resentment and frustration [30].
Dietary sources of calcium and vitamin D were another area of uncertainty for participants, explaining they were unsure what to eat and whether dietary sources replaced their supplements [26].
Role of bone densitometry (DXA) and follow-up
In one study, some participants expressed confusion regarding the purpose of bone mineral density (BMD) scanning, who it was for and why only certain parts of the skeleton were measured [26]. This viewpoint was echoed in a study of outpatients from a secondary care clinic, where participants described a need for a better understanding of DXA scans and more feedback on their results [15]. In the interview study conducted by Salter et al., the lack of follow-up was described, with a participant describing the contrast between follow-up for anti-hypertensive medication consisting of blood pressure checks to ensure medication is effective, with the absence of follow-up for bisphosphonates [27]. The authors suggest that specific medication follow-up would increase confidence in medication [27], which is supported by findings in another study where participants expressed that follow-up was needed to support persistence [19].
Factors influencing whether information needs are met
Perceived attitudes and knowledge of healthcare professionals
Many participants in the included studies perceived their physicians felt osteoporosis should be accepted as part of normal ageing, and that there physicians were uninterested in the condition in general [25, 30]. In addition to lack of interest, some studies reported the perception that their physicians had a poor knowledge of osteoporosis, in secondary [15] and in primary care [18]. Related to this was the perception that primary care physicians underestimated the impact of osteoporosis on their patient’s quality of life, calling for suggestions that patients need to be more involved in education programmes [21]. Where knowledge was perceived to be poor, study participants described a lack of confidence in their GP’s advice, particularly relating to physical activity [21]. In the study of patients with vertebral fractures, participants described a feeling of not being taken seriously by their doctors and a feeling that osteoporosis and vertebral fractures were of low priority [30].
The attitudes, beliefs and behaviours of patients
Information needs and information-seeking behaviours differed across the included studies in respect to self-efficacy, gender, age and ethnicity. McKenna et al. explored South Asian and Caucasian perceptions of support from their GP regarding non-pharmacological management [21]. The authors reported that South Asian participants differed from Caucasian participants in their information preferences in terms of tendency to consult the NOS, family members or whether they asked questions of their GP [21]. In addition, McKenna et al. consistently describe younger patients as being more proactive in seeking information, with older patients being more resigned to having osteoporosis, feeling that their actions could not change their prognosis [21]. However, in this study, the definition of ‘younger’ is not clear: the study included participants aged from 43 to 82 and quotes from two patients aged 74 and 76 are used to illustrate proactive information seeking [21].
Some studies reported that participants found it difficult to formulate questions [20]. The need for a baseline knowledge, in order to ask questions, was also described; a participant’s experience is described where she only felt confident to ask her GP questions after visiting NOS support groups [21]. The problem of lack of confidence was also acknowledged in a study of experiences of people with hip fracture, with a carer suggesting that patient advocates who can support patients in asking questions may be useful to overcome this [28].
Very little information needs were directly expressed in the studies of men [24, 29]. Male participants with osteoporosis in one study described themselves as having ‘no problems’ despite reporting daily pain or restricted activities; downplaying their symptoms or needs appeared to be part of a strategy to retain identity and a sense of masculinity [24]. Male participants in this study also described hesitation to consult their physician due to fear of receiving an osteoporosis diagnosis and how this would impact employment [24]. Efforts to consult or ask questions were sometimes to meet the information needs of female partners, rather than their own.
Context of information giving
Information given at one point in time, e.g. in a busy fracture clinic, may be too much to take in [26] and therefore some participants with osteoporosis (although not all) expressed preference for multiple opportunities to receive information through a series of consultations in primary care [21, 25]. Similarly, a busy ward environment was described as not conducive for information giving, or asking questions by patients with hip fracture, with the opportunity for multiple, repeated messages to be given during a stay in an intermediate care unit post fracture being valued [22]. This same study which investigated experiences of people with hip fracture emphasised the importance of involving relatives and carers in post-fracture information giving [22].
Types of information support
Participants wanted both written and verbal information [19, 22], and in a study where participants were asked to draw diagrams to explain their own bone health, those interviewed felt the use of more visual images would aid explanations in their routine healthcare [15]. As has been previously mentioned, ensuring that written information is understandable is key [15, 19]. Whilst many study participants already utilised other sources of information such as the NOS, participants in a Canadian study expressed a need for more community sources of information [28]. Two studies included participants that had attended support groups or group education programmes: in these studies, participants who both had and had not attended these spoke of the importance of having opportunities to meet people with similar experiences, of similar age and of similar gender [24, 25]. Others expressed an interest in being able to speak to people at a more advanced stage of osteoporosis to gain an insight into how their disease might progress, although one participant felt this might be depressing [25].
Impact of information needs being met/unmet
Initiation and adherence to treatment
In two studies, the viewpoint that osteoporosis was normal for age was cited as the principle reason for non-adherence with bisphosphonates; this viewpoint (that osteoporosis was normal for age) was either reported as being directly expressed by a health professional [25] or the patient participant’s own reflection [27]. In a focus group study by Sale et al., participants reported discontinuing medication if it did not improve symptoms [26].
DXA feedback aided medication adherence by providing evidence that the medication was working [15]. Uncertainties related to side effects and harm from the medication were reported by one participant who described being anxious as to whether they were making the ‘right choice’ to take medication [17].
Doctor-patient relationship
Maintaining a good doctor-patient relationship is reported as being integral to the promotion of adherence with drug treatment, in a secondary care study [15]. The same study discussed how poor communication, and unmet information needs, may result in a negative perception of the doctor, and resulting break-down in doctor-patient relations [15]. The strongest narrative relating to the clinician-patient relationship was described in the study of women with vertebral fractures, although this study did not present any participant quotations, nor did it make clear who the ‘healthcare providers’ were [30]. The authors report how participants described repeated feelings that their needs were not elicited by their healthcare providers, that they felt not trusted by their doctors and that this resulted in a reluctance to then talk about their situation or seek further help [30].
Social and psychological consequences
In a study of patients with hip fracture, those that were considered to have unmet educational needs appeared to have an intensified fear of falling and to be ‘emotionally floundering’, ‘grasping to understand’ and ‘more likely to miscalculate risks’ [22]. In this study, tension in relationships was also described when relatives had unmet information needs. Women with vertebral fractures were described as having feelings of helplessness, underpinned by doubt and fear of an uncertain future [30]. In this study, fear of fracture and further pain influenced participant behaviour, leading to the avoidance of activities, social withdrawal and feelings of loneliness [30]. Marked anxiety and fear of fracture was also described in the study by Hansen et al., underpinned by questions not being answered by the participant’s GP [17]. The perception of osteoporosis as a female disease, reinforced by imagery on patient information leaflets, was associated with feelings of shame and embarrassment in men with the condition [24]. The authors of two included studies compare this degree of mortification to that experienced by men diagnosed with breast cancer [24, 29].
Discussion
This review aimed to understand the information needs of patients with osteoporosis and/ or fragility fractures in order to refine research questions in this area, which is a priority for patients. The findings illustrate that one size does not fit all with a wide range of needs and preferences regarding information, as might be expected. However, the finding that core information needs prevail regarding the nature of osteoporosis, including the relationship with ageing and pain, the purpose of drug treatment, and the nature of non-pharmacological treatment, is of concern. We identified a number of barriers to information needs being met, including the perceived knowledge and attitudes of health professionals, the context in which information is given and the nature of resources supporting information exchange. Finally, we have shown that unmet information needs can have far-reaching consequences in terms of adherence to treatment, relationships with health professionals and augmenting the physical and psychosocial morbidity associated with the condition.
Wluka et al. have previously conducted an extensive review of health information needs across a range of musculoskeletal conditions [31]. This review reported that patients with rheumatoid arthritis (RA) and osteoarthritis (OA) also want to know more about the nature of the condition, as we have found. Osteoarthritis and osteoporosis are often confused [31] and both are strongly associated with ageing; however, the findings in this review and work in OA illustrate the negative impact on engagement with treatment if patients (and/or their clinicians) attribute their condition solely to ageing [31, 32]. The finding that fracture risk assessments were questioned aligns with large multicentre epidemiological study that demonstrates that postmenopausal women most at risk underestimate their own fracture risk [33]. How best to communicate fracture risk is not well established; although treatment decision aids which communicate fracture risk have been shown to improve rates of treatment adherence in small studies, they have not been qualitatively evaluated [34,35,36]. The review by Wluka et al. also reported that more information on self-management was wanted across all musculoskeletal conditions, with patients with OA also wanting more information on prognosis, and those with RA also needing more explanation about the purpose of medication [31]. Unique to osteoporosis it would seem is the need for more education and support around long-term treatment, to improve communication around the monitoring of the so-called silent disease and the effects of treatment. This may not be solely an issue around information as it is likely to be influenced by models of care for patients with osteoporosis, and the lack of formal procedures for monitoring the condition.
The factors we identified influencing whether information needs are met include the observation that some reported health information was too complex for some to understand, indicating low health literacy, which is likely to be a major contributor to unmet need. Health literacy is defined as the personal characteristics and social resources needed for individuals and communities to access, understand, appraise and use information and services to make decisions about health; in the UK, the majority of patient health information is too complex for 43% of the population who have limited health literacy [37, 38].
We also identified perceptions that osteoporosis was not of interest to clinicians; there is little qualitative research exploring the perceptions of primary care providers regarding osteoporosis but the limited evidence available does suggest the condition may carry a low priority when compared to other long-term conditions such as cardiovascular disease [39], and that these clinicians may have their own educational needs regarding osteoporosis [39, 40]. Furthermore, research with primary and secondary care clinicians suggest they underestimate the impact of the condition on their patients [41]. Not all information needs of patients need to be met by clinicians or specifically doctors, and many of the studies in this review describe how people use allied health professionals, e.g. pharmacists and dieticians, their social networks and other organisations to gain information. Participants expressed great satisfaction with information resources available from third sector organisations such as the NOS in previous focus groups conducted by our group [8]. However, the information giving in healthcare settings may need to be given a greater priority and be consistent with that given in other contexts.
We have described the impact of unmet information needs. We have inferred that psychosocial morbidity has occurred as a result of information needs being unmet, although in practice it is impossible to completely disentangle the impact of unmet information needs from the physical effects of the condition, e.g. vertebral fractures. However, unmet informational needs are very likely to be a determinant of health, evidenced by the association with health literacy and poor health outcomes which is well documented [42, 43]. Furthermore, and of relevance to osteoporosis, those with limited health literacy skills receive an inefficient mix of healthcare services, with care biased toward acute and emergency care rather than planned and preventative care [44, 45]. Adherence and persistence with bisphosphonates is known to be suboptimal and presents a major barrier to treating osteoporosis in a clinically and cost-effective manner. The findings of this synthesis reinforce the notion that addressing the beliefs and motivations of patients is of central importance in improving adherence [27]. In a systematic review of interventions designed to promote adherence, educational interventions targeted at patients had mixed results [46]. However, the content of these interventions and the theoretical basis on which they were framed is not well described, with only one study reporting attempts to elicit beliefs which may represent barriers to treatment [47].
Strengths and limitations
Augmented by the help of an information specialist, this review involved a comprehensive search of available literature on expressed information needs of patients with osteoporosis/fragility fractures. The use of multiple researchers to identify relevant literature, undertake quality assessments and code data also strengthened the review. The use of very broad search terms resulted in a large number of studies to review but also meant that relevant studies were not missed. The included studies cover a wide range of different experiences, including a range of gender, age, ethnicity and nationality, thus giving a full overview of currently available evidence on information needs among patients with osteoporosis. A further strength of this review is the exclusion of studies that tested knowledge to ensure that the findings relate to patient expressed needs, unlike previous reviews in this area [31]. We used quality assessment to both inform results and underpin conclusions. However, no study was excluded based on methodological quality and the heterogeneity of studies may limit the robustness of the synthesis.
A number of other limitations are worthy of mention. First, the population of the included studies was relatively diverse including patients with or without fracture, and either with osteoporosis or deemed at high fracture risk, reflecting the change in clinical practice over the last decade to recommend fracture prevention treatments based on fracture risk rather than the presence or absence of osteoporosis. It is possible that these clinical characteristics may influence information needs. In particular, how patients make sense of being given treatment for a condition they may not have needs to be determined. One factor which limited interpretation of the findings was that it was not always clear whether authors and/or participants were referring to primary or secondary care healthcare professionals in their descriptions [30]. Issues relating to information needs may vary considerably across countries and different healthcare contexts which may limit the generalisability of our findings. While we noted that all included studies were published within the last 10 years, changes in clinical practice may make some issues more or less relevant to contemporary healthcare settings. In particular, our findings do not cover the use of the internet or the influence of the many and multiple media reports regarding osteoporosis and the safety of osteoporosis treatments that have emerged over recent years [48]. This is of particular importance because fear of side effects is an important deterrent to patients initiating treatment [49], and there is some evidence to suggest that these media stories are influencing clinicians as well as patients [50]. Finally, as only three included studies were focused on information giving and needs, and in some studies, little data was relevant for extraction, it is possible that there remain issues not covered by this review.
Implications for practice and research
These findings raise important implications for clinical practice at the level of individual clinicians, services and wider organisations. First, health professionals (including doctors, pharmacists and nurses) involved in the care of patients with osteoporosis should reflect on to what extent they elicit or facilitate the expression of information needs and to what extent their core explanations relating to osteoporosis address issues about the nature of the condition, the purpose of medication and holistic approach to management. Second, at a service level, primary and secondary care services might consider the follow-up pathways for these patients and how these pathways are communicated to patients. Third, we suggest there is an urgent need for organisations and other providers of written information relating to osteoporosis and osteoporosis medication to ensure that material is easily understandable to those with limited health literacy. There are a number of freely available online tools that can evaluate ease of readability.
In terms of implications for research, our review has not addressed the way osteoporosis and its treatment is conceptualised in the media, and the implications of this for patient care and this remains an area where further study is needed. Understanding this societal context is critical to inform the design of public health messages. In terms of the clinician-patient encounter, the findings highlight the need to understand further healthcare professionals’ attitudes to osteoporosis, particularly that of GPs and primary care providers, and to understand the barriers to the provision of information in healthcare settings. The findings support the hypothesis that educational interventions may promote treatment adherence, but any further research in this area needs to ensure interventions are co-designed with patients, to ensure they are relevant to their needs, are applicable to a range of health literacy abilities and that the content of the interventions is explicitly mapped to the important health beliefs associated with non-adherence. Furthermore, evaluation of educational interventions should include outcomes that are patient-centred including satisfaction, self-efficacy and psychological measures. Finally, we suggest that further research is needed into the optimum ways of explaining osteoporosis and fracture risk to promote clear messages, avoid ambiguity and promote treatment persistence.
References
Department of Health. (2012) The power of information: putting all of us in control of the health and care information we need. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213689/dh_134205.pdf Accessed 02 Jan 2018
de Iongh A, Fagan P, Fenner J, Kidd L. (2015) A practical guide to self-management support: key components for successful implementation. London: The Health Foundation
Francis KL, Matthews BL, Van Mechelen W, Bennell KL, Osborne RH (2009) Effectiveness of a community-based osteoporosis education and self-management course: a wait list controlled trial. Osteoporos Int 20(9):1563–1570
Kinghan D, Carson P, Flanagan A, Megaw M. (2017) Patient education / self management programmes for people with long term conditions (2016/17). https://www.health-ni.gov.uk/sites/default/files/publications/health/pesmp-ltc-ni-16-17_0.pdf. Accessed 02 Jan 2018
Superio-Cabuslay E, Ward MM, Lorig KR (1996) Patient education interventions in osteoarthritis and rheumatoid arthritis: a meta-analytic comparison with nonsteroidal antiinflammatory drug treatment. Arthritis Care Res 9(4):292–301
Thompson B (2011) Education and learning for people with ankylosing spondylitis. Newcastle University, Newcastle, UK
Paskins Z, Jinks C, Mahmood W, Jayakumar P, Sangan CB, Belcher J, Gwilym S (2017) Public priorities for osteoporosis and fracture research: results from a general population survey. Arch Osteoporos 12(1):45
Mahmood W, Jinks C, Jayakumar P, Gwilym S, Paskins Z. (2016) 115. Public priority setting for research in osteoporosis. Rheumatology
Gemalmaz A, Oge A (2008) Knowledge and awareness about osteoporosis and its related factors among rural Turkish women. Clin Rheumatol 27(6):723–728
Matthews HL, Laya M, DeWitt DE (2006) Rural women and osteoporosis: awareness and educational needs. J Rural Health 22(3):279–283
Kasper MJ, Peterson MG, Allegrante JP (2001) The need for comprehensive educational osteoporosis prevention programs for young women: results from a second osteoporosis prevention survey. Arthritis Rheum 45(1):28–34
Hawker S, Payne S, Kerr C, Hardey M, Powell J (2002) Appraising the evidence: reviewing disparate data systematically. Qual Health Res 12(9):1284–1299
Critical Appraisal Skills Programme (CASP). (2013) CASP Qualitative Checklist. 31.05.13. http://docs.wixstatic.com/ugd/dded87_25658615020e427da194a325e7773d42.pdf Accessed 02 Jan 2018
Campbell R, Pound P, Morgan M, Daker-White G, Britten N, Pill R, Yardley L, Pope C, Donovan J (2011) Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess 15(43):1–164
Besser SJ, Anderson JE, Weinman J (2012) How do osteoporosis patients perceive their illness and treatment? Implications for clinical practice. Arch Osteoporos 7:115–124
French MR, Moore K, Vernace-Inserra F, Hawker GA (2005) Factors that influence adherence to calcium recommendations. Can J Diet Pract Res 66(1):25–29
Hansen C, Konradsen H, Abrahamsen B, Pedersen BD (2014) Women’s experiences of their osteoporosis diagnosis at the time of diagnosis and 6 months later: a phenomenological hermeneutic study. Int J Qual Stud Health Well-being 9:22438
Iversen MD, Vora RR, Servi A, Solomon DH (2011) Factors affecting adherence to osteoporosis medications: a focus group approach examining viewpoints of patients and providers. J Geriatr Phys Ther 34(2):72–81
Lau E, Papaioannou A, Dolovich L, Adachi J, Sawka AM, Burns S, Nair K, Pathak A (2008) Patients’ adherence to osteoporosis therapy: exploring the perceptions of postmenopausal women. Can Fam Physician 54(3):394–402
Mazor KM, Velten S, Andrade SE, Yood RA (2010) Older women’s views about prescription osteoporosis medication. Drugs Aging 27(12):999–1008
McKenna J, Ludwig AF (2008) Osteoporotic Caucasian and South Asian women: a qualitative study of general practitioners’ support. J R Soc Promot Heal 128(5):263–270
McMillan L, Booth J, Currie K, Howe T (2014) ‘Balancing risk’ after fall-induced hip fracture: the older person’s need for information. Int J Older People Nursing 9(4):249–257
Meadows LM, Mrkonjic L, Lagendyk L (2005) Women’s perceptions of future risk after low-energy fractures at midlife. Ann Fam Med 3(1):64–69
Nielsen DS, Brixen K, Huniche L (2011) Men’s experiences of living with osteoporosis: focus group interviews. Am J Mens Health 5(2):166–176
Nielsen DS, Huniche L, Brixen K, Sahota O, Masud T (2010) Handling osteoporosis: the importance of patient education and knowledge—a qualitative study. Bone 47:S212
Sale JE, Beaton DE, Sujic R, Bogoch ER (2010) ‘If it was osteoporosis, I would have really hurt myself.’ Ambiguity about osteoporosis and osteoporosis care despite a screening programme to educate fragility fracture patients. J Eval Clin Pract 16(3):590–596
Salter C, McDaid L, Bhattacharya D, Holland R, Marshall T, Howe A (2014) Abandoned acid? Understanding adherence to bisphosphonate medications for the prevention of osteoporosis among older women: a qualitative longitudinal study. PLoS One 9(1):e83552
Schiller C, Franke T, Belle J, Sims-Gould J, Sale J, Ashe MC (2015) Words of wisdom—patient perspectives to guide recovery for older adults after hip fracture: a qualitative study. Patient Prefer Adherence 9:57–64
Solimeo SL (2011) Living with a ‘women’s disease’: risk appraisal and management among men with osteoporosis. J Mens Health 8(3):185–191
Svensson HK, Olofsson EH, Karlsson J, Hansson T, Olsson LE (2016) A painful, never ending story: older women’s experiences of living with an osteoporotic vertebral compression fracture. Osteoporos Int 27(5):1729–1736
Wluka, AE., Chou L, Briggs A, Cicuttini F. (2016) Understanding the needs of consumers with musculoskeletal conditions: consumers’ perceived needs of health information, health services and other non-medical services: a systematic scoping review. Melbourne: MOVE muscle, bone & joint health
Paskins Z, Sanders T, Croft PR, Hassell AB (2015) The identity crisis of osteoarthritis in general practice: a qualitative study using video-stimulated recall. Ann Fam Med 13(6):537–544
Gregson CL, Dennison EM, Compston JE, Adami S, Adachi JD, Anderson FA et al (2014) Disease-specific perception of fracture risk and incident fracture rates: GLOW cohort study. Osteoporos Int 25(1):85–95
Montori VM, Shah ND, Pencille LJ, Branda ME, Van Houten HK, Swiglo BA et al (2011) Use of a decision aid to improve treatment decisions in osteoporosis: the osteoporosis choice randomized trial. Am J Med 124(6):549–556
Montori VM, Breslin M, Maleska M, Weymiller AJ (2007) Creating a conversation: insights from the development of a decision aid. PLoS Med 4(8):e233
Guyatt G, Montori V, Devereaux PJ, Schünemann H, Bhandari M (2004) Patients at the center: in our practice, and in our use of language. ACP J Club 140(1):A11–A12
Rowlands G, Protheroe J, Winkley J, Richardson M, Seed PT, Rudd R (2015) A mismatch between population health literacy and the complexity of health information: an observational study. Br J Gen Pract 65(635):e379–e386
Protheroe J, Estacio EV, Saidy-Khan S (2015) Patient information materials in general practices and promotion of health literacy: an observational study of their effectiveness. Br J Gen Pract 65(632):e192–e197
Otmar R, Reventlow SD, Nicholson GC, Kotowicz MA, Pasco JA (2012) General medical practitioners’ knowledge and beliefs about osteoporosis and its investigation and management. Arch Osteoporos 7:107–114
Richardson JC, Hassell AB, Thomas E, Hay EM (2004) GPs’ perceptions of the role of DEXA scanning: an exploratory study. Fam Pract 21(1):51–53
Rizzoli R, Brandi M, Dreinhofer K, Thomas T, Wahl D, Cooper C (2010) The gaps between participant and physician understanding of the emotional and physical impact of osteoporosis. Arch Osteoporos 5:145–153
WHO Regional Office for South-East Asia. (2015) Health literacy toolkit for low- and middle-income countries; 146p. Available from: http://www.searo.who.int/entity/healthpromotion/documents/hl_tookit/en Accessed 02 Jan 2018
Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K et al (2011) Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess (Full Rep) 199:1–941
Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z et al (2012) Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 12:80
Protheroe J, Nutbeam D, Rowlands G (2009) Health literacy: a necessity for increasing participation in health care. Br J Gen Pract 59(567):721–723
Hiligsmann M, Salas M, Hughes DA, Manias E, Gwadry-Sridhar FH, Linck P, Cowell W (2013) Interventions to improve osteoporosis medication adherence and persistence: a systematic review and literature appraisal by the ISPOR Medication Adherence & Persistence Special Interest Group. Osteoporos Int 24(12):2907–2918
Solomon DH, Iversen MD, Avorn J, Gleeson T, Brookhart MA, Patrick AR, Rekedal L, Shrank WH, Lii J, Losina E, Katz JN (2012) Osteoporosis telephonic intervention to improve medication regimen adherence: a large, pragmatic, randomized controlled trial. Arch Intern Med 172(6):477–483
Jha S, Wang Z, Laucis N, Bhattacharyya T (2015) Trends in media reports, oral bisphosphonate prescriptions, and hip fractures 1996-2012: an ecological analysis. J Bone Miner Res 30(12):2179–2187
Hall SF, Edmonds SW, Lou Y, Cram P, Roblin DW, Saag KG, Wright NC, Jones MP, Wolinsky FD (2017) Patient-reported reasons for nonadherence to recommended osteoporosis pharmacotherapy. J Am Pharm Assoc 57(4):503–509
Claesson A, Toth-Pal E, Piispanen P, Salminen H (2015) District nurses’ perceptions of osteoporosis management: a qualitative study. Osteoporos Int 26(7):1911–1918
Funding
This paper presents independent research funded by the Arthritis Research UK Centre in Primary Care grant (Grant Number 18139). GR’s time was supported by a grant from INSPIRE from Keele University School of Medicine (INSPIRE is coordinated by the Academy of Medical Sciences and supported by the Wellcome Trust. INSPIRE activities are designed and delivered locally by individual medical schools).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
ESM 1
(DOCX 17.7 kb)
Electronic supplementary material
ESM 2
(DOCX 16.7 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Raybould, G., Babatunde, O., Evans, A.L. et al. Expressed information needs of patients with osteoporosis and/or fragility fractures: a systematic review. Arch Osteoporos 13, 55 (2018). https://doi.org/10.1007/s11657-018-0470-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0470-4