Abstract
Summary
In this prospective multicenter study of osteoporotic vertebral fractures (OVFs), delayed union of OVF at 6-month follow-up caused prolonged pain, QOL impairment, ADL impairment, cognitive status deterioration, and vertebral collapse progression.
Purpose
Delayed union following osteoporotic vertebral fracture displayed as an intravertebral cleft on plain X-rays was reported to be a factor for prolonged severe pain. However, the difference of clinical course between bone union and delayed union cases still remains unclear. The purpose of this study was to identify how OVF delayed union following conventional conservative treatment influences the clinical course with a prospective multicenter study.
Methods
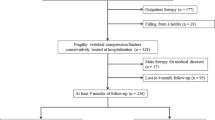
A total of 324 OVF patients from 25 institutes in Osaka, Japan, were included in the study. At the 6-month follow-up after initial visit to each institute, the patients were classified into bone union and delayed union groups based on plain X-ray findings. The outcome assessments included a VAS for back pain, SF-36 for quality of life (QOL), severity of bed-ridden state for activities of daily living (ADL), MMSE for cognitive functions, and degree of vertebral collapse on plain X-rays.
Results
Overall, 280 patients were included into the union group and 44 into the delayed union group. The VAS score at 6 months was significantly worse in the delayed union group (p = 0.01). The scores for the SF-36 scales of physical functioning and bodily pain at 6 months were significantly lower in the delayed union group (p = 0.019, p = 0.01, respectively). The percentage of nearly or completely bed-ridden patients was significantly higher in the delayed union group. The percentage of newly developed cognitive impairment was significantly higher in the delayed union group (p = 0.02). Progression of vertebral collapse during the 6-month follow-up was more pronounced in the delayed union group (p < 0.01).
Conclusion
The present results revealed that delayed union following OVF causes prolonged pain, QOL impairment, ADL impairment, cognitive status deterioration, and vertebral collapse progression.





Similar content being viewed by others
References
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767. https://doi.org/10.1016/S0140-6736(02)08657-9
Cohen L (1990) Fractures of the osteoporotic spine. Orthop Clin N Am 21(1):143–150
El Maghraoui A, Sadni S, Jbili N, Rezqi A, Mounach A, Ghozlani I (2014) The discriminative ability of FRAX, the WHO algorithm, to identify women with prevalent asymptomatic vertebral fractures: a cross-sectional study. BMC Musculoskelet Disord 15(1):365. https://doi.org/10.1186/1471-2474-15-365
Cano A, Baró F, Fernández C, Inaraja V, García-Domínguez CA (2016) Evaluation of the risk factors of asymptomatic vertebral fractures in postmenopausal women with osteopenia at the femoral neck. Maturitas 87:95–101. https://doi.org/10.1016/j.maturitas.2016.02.014
Arciero R, Leung K, Pierce J (1989) Spontaneous unstable burst fracture of the thoracolumbar spine in osteoporosis. A report of two cases. Spine (Phila Pa 1976) 14(1):114–117. https://doi.org/10.1097/00007632-198901000-00024
Lafforgue P, Chagnaud C, Daumen-Legré V, Daver L, Kasbarian M, Acquaviva P (1997) The intravertebral vacuum phenomenon (“vertebral osteonecrosis”). Migration of intradiscal gas in a fractured vertebral body? Spine (Phila Pa 1976) 22(16):1885–1891. https://doi.org/10.1097/00007632-199708150-00015
Maldague BE, Noel HM, Malghem JJ (1978) The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology 129(1):23–29. https://doi.org/10.1148/129.1.23
Malghem J, Maldague B, Labaisse M, Dooms G, Duprez T, Devogelaer J, Vande Berg B (1993) Intravertebral vacuum cleft: changes in content after supine positioning. Radiology 187(2):483–487. https://doi.org/10.1148/radiology.187.2.8475295
Naul LG, Peet GJ, Maupin WB (1989) Avascular necrosis of the vertebral body: MR imaging. Radiology 172(1):219–222. https://doi.org/10.1148/radiology.172.1.2740507
Chou L, Knight R (1997) Idiopathic avascular necrosis of a vertebral body. Case report and literature review. Spine (Phila Pa 1976) 22(16):1928–1932. https://doi.org/10.1097/00007632-199708150-00024
Hasegawa K, Homma T, Uchiyama S, Takahashi H (1998) Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976) 23(20):2201–2206. https://doi.org/10.1097/00007632-199810150-00011
Hashidate H, Kamimura M, Nakagawa H, Takahara K, Uchiyama S (2006) Pseudoarthrosis of vertebral fracture: radiographic and characteristic clinical features and natural history. J Orthop Sci 11(1):28–33. https://doi.org/10.1007/s00776-005-0967-8
Folstein M, Folstein S, McHugh P (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198. https://doi.org/10.1016/0022-3956(75)90026-6
Genant HK, Cooper C, Poor G, Reid I, Ehrlich G, Kanis J, Nordin BEC, Barrett-Connor E, Black D, Bonjour JP, Dawson-Hughes B, Delmas PD, Dequeker J, Eis SR, Gennari C, Johnell O, Johnston Jr CC, Lau EMC, Liberman UA, Lindsay R, Martin TJ, Masri B, Mautalen CA, Meunier PJ, Miller PD, Mithal A, Morii H, Papapoulos S, Woolf A, Yu W, Khaltaev N (1999) Interim report and recommendations of the World Health Organization task-force for osteoporosis. Osteoporos Int 10(4):259–264. https://doi.org/10.1007/s001980050224
(1998) Osteoporosis: review of the evidence for prevention, diagnosis and treatment and cost-effectiveness analysis. Executive summary. Osteoporos Int 8 Suppl 4:S3–6
Melton LJ, Chrischilles EA, Cooper C, Lane AW, Riggs BL (1992) Perspective. How many women have osteoporosis? J Bone Miner Res 7(9):1005–1010. https://doi.org/10.1002/jbmr.5650070902
Nishimura A, Akeda K, Kato K, Asanuma K, Yamada T, Uchida A, Sudo A (2014) Osteoporosis, vertebral fractures and mortality in a Japanese rural community. Mod Rheumatol 24(5):840–843. https://doi.org/10.3109/14397595.2013.866921
Toyone T, Tanaka T, Wada Y et al (2006) Changes in vertebral wedging rate between supine and standing position and its association with back pain: a prospective study in patients with osteoporotic vertebral compression fractures. Spine (Phila Pa 1976) 31(25):2963–2966. https://doi.org/10.1097/01.brs.0000247802.91724.7e
Begerow B, Pfeifer M, Pospeschill M, Scholz M, Schlotthauer T, Lazarescu A, Pollaehne W, Minne H (1999) Time since vertebral fracture: an important variable concerning quality of life in patients with postmenopausal osteoporosis. Osteoporos Int 10(1):26–33. https://doi.org/10.1007/s001980050190
Huang C, Ross P, Wasnich R (1996) Vertebral fractures and other predictors of back pain among older women. J Bone Miner Res 11(7):1026–1032. https://doi.org/10.1002/jbmr.5650110721
Diamond T, Champion B, Clark W (2003) Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med 114(4):257–265. https://doi.org/10.1016/S0002-9343(02)01524-3
Nevitt M, Ettinger B, Black D, Stone K, Jamal S, Ensrud K, Segal M, Genant H, Cummings S (1998) The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128(10):793–800. https://doi.org/10.7326/0003-4819-128-10-199805150-00001
Ettinger B, Black DM, Nevitt MC, Rundle AC, Cauley JA, Cummings SR, Genant HK (1992) Contribution of vertebral deformities to chronic back pain and disability. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 7(4):449–456. https://doi.org/10.1002/jbmr.5650070413
Kummell H (1895) Die rarefizierende Ostitis der Wirbelkoerper. Dtsch Med 21:180–181
Kim YC, Kim YH, Ha KY (2014) Pathomechanism of intravertebral clefts in osteoporotic compression fractures of the spine. Spine J 14(4):659–666. https://doi.org/10.1016/j.spinee.2013.06.106
Kim DY, Lee SH, Jang JS, Chung SK, Lee HY (2004) Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg 100(1 Suppl Spine):24–31
Bhalla S, Reinus W (1998) The linear intravertebral vacuum: a sign of benign vertebral collapse. AJR Am J Roentgenol 170(6):1563–1569. https://doi.org/10.2214/ajr.170.6.9609175
Omi H, Yokoyama T, Ono A, Numasawa T, Wada K, Fujisawa Y (2014) Can MRI predict subsequent pseudarthrosis resulting from osteoporotic thoracolumbar vertebral fractures? Eur Spine J 23(12):2705–2710. https://doi.org/10.1007/s00586-014-3490-9
Kawaguchi S, Horigome K, Yajima H, Oda T, Kii Y, Ida K, Yoshimoto M, Iba K, Takebayashi T, Yamashita T (2010) Symptomatic relevance of intravertebral cleft in patients with osteoporotic vertebral fracture. J Neurosurg Spine 13(2):267–275. https://doi.org/10.3171/2010.3.SPINE09364
Hoshino M, Nakamura H, Terai H, Tsujio T, Nabeta M, Namikawa T, Matsumura A, Suzuki A, Takayama K, Takaoka K (2009) Factors affecting neurological deficits and intractable back pain in patients with insufficient bone union following osteoporotic vertebral fracture. Eur Spine J 18(9):1279–1286. https://doi.org/10.1007/s00586-009-1041-6
Jang JS, Kim DY, Lee SH (2003) Efficacy of percutaneous vertebroplasty in the treatment of intravertebral pseudarthrosis associated with noninfected avascular necrosis of the vertebral body. Spine (Phila Pa 1976) 28(14):1588–1592. https://doi.org/10.1097/01.BRS.0000076824.61074.06
Murata K, Watanabe G, Kawaguchi S, Kanaya K, Horigome K, Yajima H, Morita T, Yamashita T (2012) Union rates and prognostic variables of osteoporotic vertebral fractures treated with a rigid external support. J Neurosurg Spine 17(5):469–475. https://doi.org/10.3171/2012.7.SPINE122
Boustani M, Baker MS, Campbell N, Munger S, Hui SL, Castelluccio P, Farber M, Guzman O, Ademuyiwa A, Miller D, Callahan C (2010) Impact and recognition of cognitive impairment among hospitalized elders. J Hosp Med 5(2):69–75. https://doi.org/10.1002/jhm.589
Ito Y, Hasegawa Y, Toda K, Nakahara S (2002) Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J 2(2):101–106. https://doi.org/10.1016/S1529-9430(01)00165-6
Hayashi T, Maeda T, Masuda M, Ueta T, Shiba K (2016) Morphology of the injured posterior wall causing spinal canal encroachment in osteoporotic vertebral fractures. Spine J
Acknowledgments
The authors thank Masami Tatsumi, Tomomi Tanaka, Tomoko Komaru, Aki Tanaka, Asami Satou, and Keiko Yoneda for their help in the collection of data and interviews with the patients. The authors also express their sincere thanks to the doctors from Osaka City General Hospital, Osaka City Juso Hospital, Osaka City Kita Hospital, Osaka City Sumiyoshi Hospital, Kousaiin Hospital, Hujiidera Municipal Hospital, Izumi Municipal Hospital, Aeba Surgical Hospital, Yodogawa Christian Hospital, Ishikiri Seiki Hospital, Asakayama Hospital, Osaka Ekisaikai Hospital, Kyouwa Hospital, Saiseikai Nakatsu Hospital, Saiseikai Senri Hospital, Baba Memorial Hospital, Seikeikai Hospital, Nagayoshi Sougou Hospital, Nishinomiya Watanabe Hospital, Hankai Hospital, Higashisumiyoshi Morimoto Hospital, Shitennoji Hospital, Satou Hospital, and Tsujigeka Hospital for enrolling the patients in this prospective study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study design was preapproved by the Ethical Committee for Clinical Research at the respective institutes. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 (in its most recently amended version). Informed consent was obtained from all patients included in the study.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Yasuda, H., Hoshino, M., Tsujio, T. et al. Difference of clinical course between cases with bone union and those with delayed union following osteoporotic vertebral fractures. Arch Osteoporos 13, 3 (2018). https://doi.org/10.1007/s11657-017-0411-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-017-0411-7