Abstract
Background
Empathy with patients improves clinical outcomes. Although previous studies have shown no significant differences in empathy levels between physicians and nurses, investigations have not considered differences in cultural backgrounds and related factors of healthcare providers at the individual level.
Objective
This study compares empathy between physicians and nurses in Japan and identifies relevant factors that contribute to these differences.
Design
A cross-sectional survey design was used in the study. The online survey was conducted using the Nikkei Medical Online website.
Participants
A total of 5441 physicians and 965 nurses in Japan who were registered as members of Nikkei Medical Online were included.
Main Measures
Empathy was measured by the Jefferson Scale of Empathy (JSE).
Key Results
Cronbach’s α was 0.89. The mean JSE score for Japanese physicians was significantly lower at 100.05 (SD = 15.75) than the mean score of 110.63 (SD = 12.25) for nurses (p<0.001). In related factors, higher age (increasing by one year) (+0.29; 95% CI 0.25 to 0.32; p<0.001), self-identified female gender (+5.45; 95% CI 4.40 to 6.49; p<0.001), having children (+1.20; 95% CI 0.30 to 2.10; p=0.009), and working at a hospital with 20–99 beds (+1.73; 95% CI 0.03 to 3.43; p=0.046) were significantly associated with higher scores, whereas those whose mother is a physician (−6.65; 95% CI −8.82 to −4.47; p<0.001) and father is a nurse (−9.53; 95% CI −16.54 to −2.52; p=0.008) or co-medical professional (−3.85; 95% CI −5.49 to −2.21; p<0.001) were significantly associated with lower scores.
Conclusions
Physicians had significantly lower scores on the JSE than nurses in Japan. Higher age, self-identified female gender, having children, working at a small hospital, having a mother who is a physician, and having a father who is a nurse or co-medical professional were factors associated with the level of empathy.


Similar content being viewed by others
Data Availability:
Data supporting the findings of this study are available from the General Medicine Center of Shimane University Hospital (e-mail: shimanegp@gmail.com).
References
Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359-64. doi: https://doi.org/10.1097/ACM.0b013e3182086fe1.
Lamiani G, Dordoni P, Vegni E, Barajon I. Caring for critically ill patients: clinicians’ empathy promotes job satisfaction and does not predict moral distress. Front Psychol. 2020;10:2902. doi: https://doi.org/10.3389/fpsyg.2019.02902.
Del Canale S, Louis DZ, Maio V, et al. The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad Med. 2012;87(9):1243-9. doi:https://doi.org/10.1097/ACM.0b013e3182628fbf
Hojat M, Louis DZ, Maio V, Gonnella JS. Empathy and health care quality. Am J Med Qual. 2013;28(1):6-7. doi:https://doi.org/10.1177/1062860612464731
Ogle J, Bushnell JA, Caputi P. Empathy is related to clinical competence in medical care. Med Educ. 2013;47(8):824-31. doi:https://doi.org/10.1111/medu.12232
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159(9):1563-9. doi: https://doi.org/10.1176/appi.ajp.159.9.1563.
Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88(8):1171-7. doi:https://doi.org/10.1097/ACM.0b013e318299f3e3
Jeffrey D. Empathy, sympathy and compassion in healthcare: is there a problem? Is there a difference? Does it matter? J R Soc Med. 2016;109(12):446-52. doi:https://doi.org/10.1177/0141076816680120
Samarasekera DD, Lee SS, Yeo JHT, Yeo SP, Ponnamperuma G. Empathy in health professions education: what works, gaps and areas for improvement. Med Educ. 2023;57(1):86-101. doi: https://doi.org/10.1111/medu.14865. Epub 2022 Jul 16. PMID: 35790499.
LeVasseur J, Vance DR. Doctors, nurses, and empathy. In: Spiro HM, Curnen M McC MG, eds. Empathy and the Practice of Medicine: beyond Pills and the Scalpel. New Haven, CT: Yale University Press; 1993.
Pedersen R. Empirical research on empathy in medicine-a critical review. Patient Educ Couns. 2009;76(3):307-22. doi: https://doi.org/10.1016/j.pec.2009.06.012.
Baumann AO, Deber RB, Silverman BE, Mallette CM. Who cares? Who cures? The ongoing debate in the provision of health care. J Adv Nurs. 1998;28(5):1040-5. doi: https://doi.org/10.1046/j.1365-2648.1998.00809.x.
Fields SK, Hojat M, Gonnella JS, Mangione S, Kane G, Magee M. Comparisons of nurses and physicians on an operational measure of empathy. Eval Health Prof. 2004;27(1):80-94. doi: https://doi.org/10.1177/0163278703261206.
Nikkei Medical Online website. Available at: https://medical.nikkeibp.co.jp. Accessed June 7, 2023.
Hojat M, DeSantis J, Shannon SC, et al. The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ Theory Pract. 2018;23(5):899-920. doi: https://doi.org/10.1007/s10459-018-9839-9.
Thomas Jefferson University website. Available at: https://www.jefferson.edu/academics/colleges-schools-institutes/skmc/research/research-medical-education/jefferson-scale-of-empathy.html Accessed November 12, 2023.
Hojat M, DeSantis J, Shannon SC, et al. The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ Theory Pract. 2018;23(5):899-920. doi: https://doi.org/10.1007/s10459-018-9839-9.
Hasan S, Al-Sharqawi N, Dashti F, et al. Level of empathy among medical students in Kuwait University, Kuwait. Med Princ Pract. 2013;22(4):385-89. doi: https://doi.org/10.1159/000348300.
Kataoka HU, Koide N, Hojat M, Gonnella JS. Measurement and correlates of empathy among female Japanese physicians. BMC Med Educ. 2012;12:48. doi: https://doi.org/10.1186/1472-6920-12-48.
Kuo JC, Cheng JF, Chen YL, Livneh H, Tsai TY. An exploration of empathy and correlates among Taiwanese nurses. Jpn J Nurs Sci. 2012;9(2):169-76. doi: https://doi.org/10.1111/j.1742-7924.2011.00199.x.
Simmenroth-Nayda A, Görlich Y. Medical school admission test: advantages for students whose parents are medical doctors? BMC Med Educ. 2015;15:81. doi: https://doi.org/10.1186/s12909-015-0354-x.
Christov-Moore L, Simpson EA, Coudé G, Grigaityte K, Iacoboni M, Ferrari PF. Empathy: gender effects in brain and behavior. Neurosci Biobehav Rev. 2014;46(Pt 4):604-27. doi: https://doi.org/10.1016/j.neubiorev.
Costa Martins M, Santos C, Fernandes M, Veríssimo M. Attachment and the development of prosocial behavior in children and adolescents: a systematic review. Children (Basel). 2022;9(6):874. doi: https://doi.org/10.3390/children9060874.
Watari T, Nagai N, Kono K, Onigata K. Background factors associated with academic motivation for attending medical school immediately after admission in Japan: a single-center study. J Gen Fam Med. 2022;23(3):164-71. doi: https://doi.org/10.1002/jgf2.528.
Shi C, Cleofas JV. Professional commitment and willingness to care for people living with HIV among undergraduate nursing students: the mediating role of empathy. Nurse Educ Today. 2022;119:105610. doi: https://doi.org/10.1016/j.nedt.2022.105610.
Shariat SV, Eshtad E, Ansari S. Empathy and its correlates in Iranian physicians: a preliminary psychometric study of the Jefferson Scale of Physician Empathy. Med Teach. 2010;32(10):e417-21. doi: https://doi.org/10.3109/0142159X.2010.498488.
Hojat M, Gonnella JS. Eleven years of data on the Jefferson Scale of Empathy-Medical Student Version (JSE-S): proxy norm data and tentative cutoff scores. Med Princ Pract. student version. 2015;24(4):344-50. doi: https://doi.org/10.1159/000381954.
Assing Hvidt E, Søndergaard J, Wehberg S, Hvidt NC, Andersen CM. A cross-sectional study of student empathy across four medical schools in Denmark-associations between empathy level and age, sex, specialty preferences and motivation. BMC Med Educ. 2022;22(1):489. doi: https://doi.org/10.1186/s12909-022-03532-2.
Hampson E, Anders Van S, Mullin L. A female advantage in the recognition of emotional facial expressions: test of an evolutionary hypothesis. Evol Hum Behav. 2006;27(6):401-16. doi: https://doi.org/10.1016/j.evolhumbehav.2006.05.002.
Christov-Moore L, Simpson EA, Coudé G, Grigaityte K, Iacoboni M, Ferrari PF. Empathy: gender effects in brain and behavior. Neurosci Biobehav Rev. 2014;46(Pt 4):604-27. doi: https://doi.org/10.1016/j.neubiorev.2014.09.001.
O’Brien E, Konrath SH, Grühn D, Hagen AL. Empathic concern and perspective taking: linear and quadratic effects of age across the adult life span. J Gerontol B Psychol Sci Soc Sci. 2013;68(2):168-75. doi: https://doi.org/10.1093/geronb/gbs055.
Park C, Lee YJ, Hong M, et al. A multicenter study investigating empathy and burnout characteristics in medical residents with various specialties. J Korean Med Sci. 2016;31(4):590-97. doi: https://doi.org/10.3346/jkms.2016.31.4.590.
Nightingale F. Notes on nursing: what it is, and what it is not. New York: Harrison; 1860.
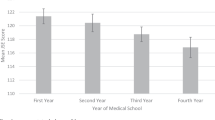
Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182-91. doi: https://doi.org/10.1097/ACM.0b013e3181b17e55.
Newton BW, Barber L, Clardy J, Cleveland E, O’Sullivan P. Is there hardening of the heart during medical school? Acad Med. 2008;83(3):244-9. doi: https://doi.org/10.1097/ACM.0b013e3181637837.
Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38(9):934-41. doi: https://doi.org/10.1111/j.1365-2929.2004.01911.x.
Kataoka HU, Koide N, Ochi K, Hojat M, Gonnella JS. Measurement of empathy among Japanese medical students: psychometrics and score differences by gender and level of medical education. Acad Med. 2009;84(9):1192-7. doi: https://doi.org/10.1097/ACM.0b013e3181b180d4.
Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27(10):1280-6. doi: https://doi.org/10.1007/s11606-012-2063-z.
Acknowledgements:
We would like to thank all those who assisted us in completing this study. In particular, we appreciate the generous cooperation of the Nikkei Medical Online staff. We also thank the members of the Shimane University Center for General Medicine for their support in conducting this study.
Funding
This work was supported by the National Academic Research Grant Fund (JSPS KAKENHI: 20H03913). The sponsor of the study had no role in the study design, data collection, analysis, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
T.W. served as the principal investigator of the entire study. T.O., Y.N., D.Y., M.M., and T.W. collaborated on designing the study, formulating the main conceptual ideas, and outlining the proof. Data collection through a web survey was conducted by T.O., T.W., K.S., Y.S., T.Y., M.M., D.Y., and H.K. The gathered data was subsequently analyzed and visualized by T.O., S.K., Y.S., T.E., S.O., H.K., and T.W. The results were interpreted by T.O., K.S., T.E., S.O., and T.W. The manuscript was authored by T.O. and T.W. with the assistance of the others. N.H., H.K., Y.S., Y.T., and T.W. provided supervision for this study. The manuscript underwent revisions by T.O., T.W., Y.T., N.H., and H.K. All authors discussed the results and provided feedback on the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare no conflict of interest. All authors have reviewed and agreed to the content of the manuscript, and there are no financial interests to declare.
Consent for Publication:
All authors have reviewed and agreed to publish the whole content of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
Question: What are the differences in levels of empathy between physicians and nurses in Japan and the factors influencing them?
Findings: In this cross-sectional study that included 6406 participants, the mean Jefferson Scale of Empathy (JSE) score for Japanese physicians was significantly lower than that for nurses. In terms of related factors, higher age, self-identified female gender, having children, and working at a small hospital were significantly associated with higher scores, whereas those whose mother is a physician and father is a nurse had significantly lower scores.
Meaning
Higher age, self-identified female gender, having children, working at a small hospital, having a mother who is a physician, and having a father who is a nurse were factors associated with the level of empathy.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Otsuka, T., Sakaguchi, K., Houchens, N. et al. Empathy Among Physicians and Nurses in Japan: A Nationwide Cross-sectional Study. J GEN INTERN MED 39, 960–968 (2024). https://doi.org/10.1007/s11606-024-08620-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-024-08620-1