Abstract
Background
Hospital capacity strain impacts quality of care and hospital throughput and may also impact the well being of clinical staff and teams as well as their ability to do their job. Institutions have implemented a wide array of tactics to help manage hospital capacity strain with variable success.
Objective
Through qualitative interviews, our study explored interventions used to address hospital capacity strain and the perceived impact of these interventions, as well as how hospital capacity strain impacts patients, the workforce, and other institutional priorities.
Design, Setting, and Participants
Qualitative study utilizing semi-structured interviews at 13 large urban academic medical centers across the USA from June 21, 2019, to August 22, 2019 (pre-COVID-19). Interviews were recorded, professionally transcribed verbatim, coded, and then analyzed using a mixed inductive and deductive method at the semantic level.
Main Outcome Measures
Themes and subthemes of semi-structured interviews were identified.
Results
Twenty-nine hospitalist leaders and hospital leaders were interviewed. Across the 13 sites, a multitude of provider, care team, and institutional tactics were implemented with perceived variable success. While there was some agreement between hospitalist leaders and hospital leaders, there was also some disagreement about the perceived successes of the various tactics deployed. We found three main themes: (1) hospital capacity strain is complex and difficult to predict, (2) the interventions that were perceived to have worked the best when facing strain were to ensure appropriate resources; however, less costly solutions were often deployed and this may lead to unanticipated negative consequences, and (3) hospital capacity strain and the tactics deployed may negatively impact the workforce and can lead to conflict.
Conclusions
While institutions have employed many different tactics to manage hospital capacity strain and see this as a priority, tactics seen as having the highest yield are often not the first employed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
BACKGROUND
Hospital capacity strain results when there is a mismatch between supply and demand on any resources a hospital uses to provide care (e.g., beds, nurses, physicians, equipment).1 This is often defined as increased bed demand relative to hospital bed or resource supply1 and has been shown to negatively impact patient care,1,2,3,4,5,6,7 increase costs,8 and disrupt patient flow.9,10,11,12,13 Large academic medical centers have been found to be at particular risk of having daily patient demand exceed supply14 and therefore often face capacity strain; this was further heightened by the COVID-19 pandemic.15,16
The Institute for Healthcare Improvement published the white paper “Achieving Hospital-Wide Patient Flow” that provides a framework for hospitals to improve hospital-wide patient flow through the framework of “the right care, in the right place, at the right time.”14 Numerous specific interventions to manage capacity strain and optimize patient flow have been described in the literature, including strategies that focus on earlier discharges, huddles, and reducing unnecessary hospital days.17,18,19,20,21 It is clear that hospital flow is of strategic importance to many hospital systems; however, the perceived impact of the various strategies has not been well studied.
To better understand the experience of hospitalist leaders and hospital leaders, we utilized qualitative methods to explore interventions used to address hospital capacity strain and the perceived impact of these interventions, as well as how hospital capacity strain impacts patients, the workforce, and other institutional priorities.
METHODS
Study Design
We conducted semi-structured interviews via telephone and through in-person meetings with hospital leaders and hospitalist leaders at large academic medical centers to understand the strategies they utilize to combat hospital capacity strain. The Colorado Multiple Institutional Review Board (COMIRB), University of Colorado, Aurora, reviewed and approved the study. Interviews were conducted from June 21, 2019, to August 22, 2019.
Setting and Participants
Interviews were conducted with participants from 13 academic medical centers. Academic medical centers were chosen for this study as they may be more likely to experience hospital capacity strain.14 To select sites, stratified purposeful expert sampling was performed after creating a comprehensive list of US medical schools along with their respective hospitals, identifying those that had over 200 beds and had hospital medicine groups (sections or divisions). We included hospitals from all regions as grouped by American Hospital Association (AHA) Regions22 and then combined these into larger regions for reporting to ensure anonymity.
We included both hospitalist leaders and hospital leaders as participants to ensure diverse perspectives were included given the focus of this work impacts both groups of leaders and it has also been suggested that alignment between medical staff and executive leaders is needed in order to build successful patient flow initiatives.14 We hypothesized that the perspectives might be different and important to explore. Hospitalist leaders were leaders in their hospital medicine group who had knowledge of and led initiatives related to managing hospital capacity strain and hospitalist operations such as staffing and service planning and similarly for hospital leaders except that their role was focused on hospital flow. A convenience sample of hospitalist leaders and hospital leaders was selected from the list of hospitals meeting inclusion criteria. When contacted, individuals were asked if their institution faced hospital capacity strain, whether they were interested in participating, and whether they felt they were the appropriate contact for their institution. If not, we asked for suggested participants at their respective site (snowball sampling). Only hospitals that stated they faced hospital capacity strain were included. Consent was performed during the in-person meeting or phone call and participants were provided the consent form prior to the consent discussion and interview.
Interview Guide
Semi-structured interviews with the hospitalist leaders and hospital leaders used open-ended questions to explore interventions used to address hospital capacity strain and the perceived impact of these interventions. Interviews typically lasted one hour.
Questions were derived through a literature review as well as hospitalist expertise and practical experience (collectively spanning more than four decades of experience in the field). Hospital capacity strain was defined as excess bed demand relative to hospital bed or resource supply.1,23 A broad definition of hospital capacity strain was utilized for this study as both space and staffing constraints may be encountered by hospitals facing hospital capacity strain. We utilized the job demand–resource model of burnout24 and the conceptual model for integrated approaches to the protection and promotion of worker health and safety by Sorensen et al. in hospital settings25 as the guiding models for this study, namely that workplace policies and practices can directly impact the workforce and enterprise outcomes.25 The full interview guides are available in Appendices 1 and 2.
Data Collection
Eligible participants were consented and interviewed by investigators (M.B., S.A., and N.V.). Interviews were conducted by S.A. and N.V. (each were in the process of pursuing doctorate-level degrees at the time of the study) with the assistance of a hospitalist physician with qualitative research experience (M.B.). Recruitment of participants was halted when no new codes or themes emerged during analysis.
Interviews were audio-recorded and transcribed. Any identifiers inadvertently captured on the audio-files were removed during professional transcription. The interview transcripts were then supplemented with notes and observations by research personnel made during the interviews. After professional transcription, interviews were imported into the Dedoose qualitative software program.
Analysis
Coding for themes was conducted (S.A., N.V., A.K., S.A., K.B., M.K., M.D., L.M., and M.B.). Both inductive and deductive coding approaches were applied to identify themes hypothesized a priori as well as new themes emerging from the data. An initial codebook was developed a priori, with new codes added as interviews and analysis were conducted. To ensure consensus, research personnel met virtually as a group to code two interviews together. After individual coding for each transcript was completed by at least two researchers, researchers virtually met as a group to harmonize any code disagreements. An inter-rater agreement was not measured as consensus was found through discussion. A thematic analysis was conducted using a mixed inductive and deductive method at the semantic level.26 Coded transcripts were analyzed both within hospitalist leader and hospital leader roles and across roles to identify commonalities and differences. Member checking,27 a technique for exploring the credibility of results, did not yield additional significant revisions.
RESULTS
A total of 29 leaders participated in 27 interviews at a total of 13 large academic medical centers (all 200 beds or more). There were sites from all nine American Hospital Association Regions.28 Interviews were conducted with 13 hospitalist leaders and 16 hospital leaders and noted in Figure 1. All sites that were approached participated with at least one interview (100% site participation). All sites had an interview with a hospitalist leader and all but one site had a hospital leader. All interviews had one participant except one, which had three individuals from the same site and all were hospital leaders. Demographic data for the hospitals the participants were associated with are in Table 1. Specific roles of the respondents were omitted to ensure anonymity; however, high-level roles (physician, non-physician) are noted in Figure 1.
Across the 13 sites studied, a multitude of provider, care team, and institutional tactics were implemented with perceived variable success (Tables 2 and 3). The solutions that were most highly recommended were (1) ensuring appropriate staffing, (2) having proactive data-driven approaches which were felt to be more helpful than multiple pages and meetings, (3) planning for discharge at the time of admission, (4) establishing protocols and plans to manage high-capacity days, and (5) identifying barriers to discharge with a multidisciplinary approach. While there was some agreement between hospitalist leaders and hospital leaders, there was also some disagreement about the perceived successes of the various tactics deployed. Interventions that overall were perceived as positive were caps on patient loads, huddles, multidisciplinary rounds, and triagist roles. On-call providers received mixed reviews. Overall negative interventions were discharge lounges, flexing providers from teaching teams to non-teaching teams, and care escalation initiatives. Hospitalist leaders often felt multiple huddles and new care areas (i.e., surge spaces or adapting non-care areas into areas where patient care is provided) were interventions that were not perceived as successful in helping with capacity strain, whereas hospital leaders felt that designated discharge nurses, using existing staff and resources without adding staff or resources as census rises, and care escalation processes were not perceived as successful. Hospital leaders had mixed reviews on post-acute care contracts, predictive modeling, discharge lounges, and huddles. A coding summary for hospitalist and hospital leaders is provided in Appendix 3.
Themes
Three main themes as elucidated from hospitalist leaders and hospital leaders emerged and are shown below along with the subthemes and verbatim exemplar quotes.
Theme 1: Hospital capacity strain is complex and difficult to predict
Hospitalist leaders and hospital leaders agree that drivers of hospital capacity are complex and difficult to predict, which often leads to conflict and the sense of constant “churn.” Because of the lack of predictability, staffing concerns often lag.
It is like the spigot game…you got one spigot that’s coming out, you put a finger in that to stop it, then also there's the other spigot that now comes out spraying water...it’s like anything else that you solve one problem, careful you may open up a new problem to be encountered. (Participant 110b, hospitalist leader)
Theme 2: The interventions that were perceived to have worked the best when facing strain were to ensure appropriate resources; however, less costly solutions were often deployed and this may lead to unanticipated negative consequences
Both leader types recognized that the capacity crisis was almost daily, caused stress, and that resources often lagged. Because drivers of hospital capacity are complex and difficult to predict, resource allocation can be challenging. Resources and time were felt to be very valuable in managing hospital capacity strain; however, they often lagged or were not deployed in response to the current crisis.
Staffing
Participants noted the need to ensure enough providers for volume, often using a formula based on census with the goal of keeping numbers stable across teams/providers and with a consistent workload. It was perceived as stressful for providers when the hospital became progressively busier with no maximum in sight. Solutions often fell into (1) asking providers on service to take on more patients in a day, (2) adding staff like a backup/on-call/jeopardy system (perceived as challenging because this system is often used for providers who call in sick), or (3) using moonlighters to add staff when needed. The biggest challenges were often noted to be financial (balancing being overstaffed versus understaffed) and accurate projections of volume to know when to staff up because projections are difficult in a constantly changing environment. In addition, some solutions such as moonlighters were perceived as costly and potentially unsafe due to discontinuity of care and there were essentially thresholds at which you can run out of providers to pick up the extra work.
It is ideal to staff at a level where it is just built-in that there is some ability to flex up. There’s really no way to accurately model and predict volume if you’re a large academic medical center treating all variety of patients, you can’t control, if you have an open emergency room, you have a large network, you’re taking referrals, it’s very, very difficult to control volume, so you have to accommodate it. The best way to do it is to sort of staff to a level that allows for some flexibility, to flex up to accommodate sort of maybe 90% of the variation. (Participant 106b, hospitalist leader)
Participants noted that increasing providers, calling in float pool nurses, and adding beds to handle increases in volume does not ensure that the other necessary resources for delivering patient care are available such as care management, social work, physical therapy, occupational therapy, speech and language therapy, respiratory therapy, and imaging.
The high-capacity situation has created busy days, seeing larger numbers of patients, which it is just physically and cognitively mentally harder, and potentially creates more frustrations as well because all of the available resources in the hospital can get soaked up, and the things that normally happen quickly happen more slowly, which then creates a vicious cycle… it creates inefficiencies. (Participant 101b, hospitalist leader)
Time
Time is a resource in short supply in a high-capacity strain environment. Those interviewed reflected that it takes time to decompress the hospital after patient volume decreases. In addition, there is not enough time in a day for providers to complete all their tasks if caring for a large number of patients, with institutional initiatives seeming to directly compete with each other in order to finish everything before noon (discharges, calling consultants, multidisciplinary meetings).
The other direct impact obviously is if you are doing QI [quality improvement] or clinical research that relies heavily on workflows being in a certain way, and every time there is a stress on the health system to discharge patients early or keep the flow going, these workflows might be altered and again, would impact your studies... The other side of it is how the human factors the burnout and the constant request for moonlighting, like a lot of people in good faith want to moonlight to help other colleagues, but that time is actually coming out of their research and personal time. (Participant 102b, hospitalist leader)
Unintended Consequences
Participants noted that some of the most commonly implemented initiatives can often have unintended consequences, including distracting from patient care, burnout, and delayed abilities to properly staff for patient care.
It was really just a very inefficient system that people would then try to cram and make work faster and better than they normally would, but something I think makes the providers feel nagged when everyone’s paging, they’re trying to see patients, and they’re running around the hospital trying to find this one patient that got tucked away somewhere in the back of the outpatient area here, and at the same time getting emailed and called and pages, asking if you can discharge people as quickly as possible. (Participant 101b, hospitalist leader)
Theme 3: When a hospital is facing hospital capacity strain, it negatively impacts the workforce and can lead to conflict
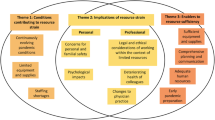
Hospital capacity strain was perceived to have negatively impacted patients, providers, and staff, and it was also noted to encroach upon other academic medical center missions such as education, research, innovation, and financial stability. Appendix 4 highlights these key subtheme areas by key stakeholder groups and core mission areas. Figure 2 is a conceptual model depicting the impact of hospital capacity strain on the workforce, the patients, and institutional priorities. Additional subthemes emerged and are shown below.
The tactics implemented to mitigate hospital capacity strain directly impacts the ability of providers to do their jobs
The many different initiatives that hospitals craft to mitigate hospital capacity strain can have a perceived negative impact on care team members’ abilities to do their jobs. Participants noted being pulled in many different directions and often bombarded with a wide array of communication tactics. This also limited the ability to do other academic work such as teaching.
Because you have a lot of patients and you’re concentrating on the difficult ones. But there could be ones that you know, instead of saying, “Oh, let’s wait until tomorrow,” if you would have had the chance to sort of circle back and evaluate throughout the day you might have been able to get them out that day. But because you’re working on other difficult patients or just the sheer number of patients, then you might not have had that chance to really pay attention closely to a patient. (Participant 112a, hospital leader)
Hospital capacity strain impacts the well being of providers
Hospital capacity strain and the tactics implemented were perceived to lead to increased stress and tension which places providers at increased risk of burnout.
Unfortunately, in the meantime, when you are outnumbered with patients, and finding it difficult to provide the type of care that our providers want to give, there is a long time before you can staff up appropriately to make sure you’re managing that well, and that puts a strain on people and their morale, and their sense of whether this position—this job is sustainable. (Participant 102b, hospitalist leader)
The tension between sufficient resources, the tactics deployed, and being able to do one’s job creates conflict
Conflict was perceived to be experienced when tactics to address hospital capacity strain were implemented without sufficient additional resources.
Years ago, before we had a true throughput surge plan, what the typical strategy was for someone in the ED to e-mail someone in hospital leadership, like the president, and say, “It’s crazy down here, can you get those guys upstairs to discharge?” It was very confrontational. (Participant 105b, hospitalist leader)
DISCUSSION
We found that hospital capacity strain was perceived to have wide-reaching impact at each of the participating sites. Participants from all institutions noted a continued struggle with how to manage hospital capacity strain and had implemented numerous measures with variable success. Both hospitalist leaders and hospital leaders felt that the most effective way to address strain is often through ensuring sufficient resources, particularly through staffing, but noted that it is often not the first intervention utilized. Instead, seemingly more cost neutral interventions (e.g., discharge lounge or huddles) are implemented first, even though most people interviewed felt they do not fix the problem and may lead to negative consequences and a repetitive cycle of lagging resources and stress.
There is limited literature about the impact of hospital capacity strain on the various stakeholders and key mission areas of academic medical centers. Some reports have highlighted the impact of hospital capacity strain on timeliness of discharge,29 length of stay,6,7 and quality of care1; however, this study highlights the consequences on the workforce with the words “churn,” “burnout,” and “conflict” frequently utilized when describing how the inpatient workforce manages hospital capacity strain. Clinician burnout is consequential not only for individual providers but also for health care systems, as it may lead to providers leaving the workforce,30,31,32 medical errors,33,34,35,36,37 and has been projected to cost $4.6 billion annually in the USA for burnout related to physicians.38
Hospitalist leaders and hospital leaders had differing opinions on the impact of the various initiatives aimed at improving patient flow and capacity. The perception of conflict was noted throughout the interviews. Workflows may differ for various roles, so an assessment of how these well-intentioned interventions may impact the workforce’s ability to get work done may be necessary as it was noted that some of the interventions could cause distractions and negatively impact patient care.
Some research has suggested that adequate staffing may lend itself to more expedited care and potential cost savings. Elliott et al. showed that increasing hospitalist workload is associated with clinically meaningful increases in length of stay and cost.39 Previous work by Michtalik et al. highlighted that having fixed census caps on teams decreased the odds of reporting unsafe census situations.40 Thus, while adequate staffing may require resources, these studies suggest that the cost may be offset through improved patient flow and improved patient safety. This study suggests that often hospitals employ less costly solutions to address hospital capacity strain; however, the reasons behind why hospital systems choose measures that are perceived to be less effective is unknown and could be a future area of study. Future work should focus on the economic impact of the various initiatives, in particular the impact of high patient census and increased workloads (and cognitive load) as well as interventions that may inadvertently result in provider distractions.
Our study has several strengths. We explored both the hospitalist leader and hospital leader perspectives to understand the impact of hospital capacity strain on key stakeholders and core mission areas as well as the impact of the various tactics deployed to manage strain. We included both perspectives given hospitalist leaders and hospital leaders might have distinct perspectives on the topic given different incentives, constraints, and resources available to respond to capacity strain situations. We also included a large number of institutions from a variety of geographic regions. This work adds to the understanding of which strategies have been deployed and the experiences with these initiatives. While several studies have shown the operational impact of hospital capacity strain (through increased length of stay and mortality), we believe this is one of the first to show the impact on the workforce (i.e., ability to do one’s job, conflict, well being), though there is increasing literature on how COVID-19 has strained clinical care teams.41
Our study also has some limitations. It involved large academic medical centers with greater than 200 beds and hospital medicine groups, and thus, our findings may not apply to smaller hospitals or non-academic medical centers or institutions without hospitalist groups. We interviewed two individuals (a hospitalist leader and hospital leader) at most institutions and thus our findings may not represent the beliefs of frontline workers, though many of the hospitalist leaders were also frontline clinicians. Hospital leaders that were interviewed also had a variety of roles some of which were hospitalists (i.e., hospitalists that led initiatives for the hospital) and thus some of the perspectives could have overlapped between the two groups. Lastly, this work covers hospital capacity situations that may differ from a crisis situation (e.g., COVID, mass casualty event) though likely with some overlapping components.
CONCLUSION
Across the 13 sites, a multitude of provider, care team, and institutional tactics were implemented with variable success. Hospital capacity strain was perceived as complex and difficult to predict with wide-reaching impact on patients, the workforce, and institutional priorities. While ensuring appropriate resources was felt to be key to managing hospital capacity strain, less costly solutions were perceived to be deployed that may result in further negative consequences and conflict.
References
Eriksson CO, Stoner RC, Eden KB, Newgard CD, Guise JM. The Association between hospital capacity strain and inpatient outcomes in highly developed countries: a systematic review. J Gen Intern Med 2017;32:686-96.
Schilling PL, Campbell DA, Jr., Englesbe MJ, Davis MM. A comparison of in-hospital mortality risk conferred by high hospital occupancy, differences in nurse staffing levels, weekend admission, and seasonal influenza. Med Care 2010;48:224-32.
Gaieski DF, Agarwal AK, Mikkelsen ME, et al. The impact of ED crowding on early interventions and mortality in patients with severe sepsis. Am J Emerg Med 2017;35:953-60.
Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med 2010;28:304-9.
Singer AJ, Thode HC, Jr., Viccellio P, Pines JM. The association between length of emergency department boarding and mortality. Acad Emerg Med 2011;18:1324-9.
White BA, Biddinger PD, Chang Y, Grabowski B, Carignan S, Brown DF. Boarding inpatients in the emergency department increases discharged patient length of stay. J Emerg Med 2013;44:230-5.
Forster AJ, Stiell I, Wells G, Lee AJ, van Walraven C. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med 2003;10:127-33.
Foley M, Kifaieh N, Mallon WK. Financial impact of emergency department crowding. West J Emerg Med 2011;12:192-7.
McGowan JE, Truwit JD, Cipriano P, et al. Operating room efficiency and hospital capacity: factors affecting operating room use during maximum hospital census. J Am Coll Surg 2007;204:865-71; discussion 71-2.
Khanna S, Boyle J, Good N, Lind J. Early discharge and its effect on ED length of stay and access block. Stud Health Technol Inform 2012;178:92-8.
Powell ES, Khare RK, Venkatesh AK, Van Roo BD, Adams JG, Reinhardt G. The relationship between inpatient discharge timing and emergency department boarding. J Emerg Med 2012;42:186-96.
Khanna S, Sier D, Boyle J, Zeitz K. Discharge timeliness and its impact on hospital crowding and emergency department flow performance. Emerg Med Australas 2016;28:164-70.
Wertheimer B, Jacobs RE, Iturrate E, Bailey M, Hochman K. Discharge before noon: effect on throughput and sustainability. J Hosp Med 2015;10:664-9.
Rutherford PA, Anderson A, Kotagal UR, Luther K, Provost LP, Ryckman FC, Taylor J. Achieving hospital-Wide Patient Flow (Second edition) IHI White Paper Boston, Massachusetts: Institute for Healthcare Improvement; 2020 (Available at www.ihi.org)
Bowden K, Burnham EL, Keniston A, et al. Harnessing the power of hospitalists in operational disaster planning: COVID-19. J Gen Intern Med 2020;35:2732-7.
Keeley C, Jimenez J, Jackson H, et al. Staffing up for the surge: expanding the new york city public hospital workforce during the COVID-19 pandemic. Health Aff (Millwood) 2020;39:1426-30.
Kane M, Weinacker A, Arthofer R, et al. A multidisciplinary initiative to increase inpatient discharges before noon. J Nurs Adm 2016;46:630-5.
Patel H, Yirdaw E, Yu A, et al. Improving early discharge using a team-based structure for discharge multidisciplinary rounds. Prof Case Manag 2019;24:83-9.
El-Eid GR, Kaddoum R, Tamim H, Hitti EA. Improving hospital discharge time: a successful implementation of Six Sigma methodology. Medicine (Baltimore) 2015;94:e633.
Beck MJ, Okerblom D, Kumar A, Bandyopadhyay S, Scalzi LV. Lean intervention improves patient discharge times, improves emergency department throughput and reduces congestion. Hosp Pract (1995) 2016;44:252-9.
Chadaga SR, Shockley L, Keniston A, et al.Hospitalist-led medicine emergency department team: associations with throughput, timeliness of patient care, and satisfaction. J Hosp Med 2012;7:562-6.
American Hospital Association Regions American Hospital Association. Available at: https://wwwahvrporg/sites/default/files/aha-regional-mappdf. Accessed May 1, 2021.
Kohn R, Harhay MO, Bayes B, et al. Ward capacity strain: a novel predictor of 30-day hospital readmissions. J Gen Intern Med 2018;33:1851-3.
Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol 2001;86:499-512.
Sorensen G, McLellan DL, Sabbath EL, et al. Integrating worksite health protection and health promotion: a conceptual model for intervention and research. Prev Med 2016;91:188-96.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006;3:77-101.
Birt L, Scott S, Cavers D, Campbell C, Walter F. Member checking: a tool to enhance trustworthiness or merely a nod to validation? Qual Health Res 2016;26:1802-11.
American Hospital Association (AHA) Regions. https://wwwahvrporg/sites/default/files/aha-regional-mappdf. Accessed January 31, 2021.
Zoucha J, Hull M, Keniston A, et al. Barriers to Early Hospital Discharge: A Cross-Sectional Study at Five Academic Hospitals. J Hosp Med 2018;13:816-22.
Pantenburg B, Luppa M, Konig HH, Riedel-Heller SG. Burnout among young physicians and its association with physicians’ wishes to leave: results of a survey in Saxony, Germany. J Occup Med Toxicol 2016;11:2.
Hamidi MS, Bohman B, Sandborg C, et al. Estimating institutional physician turnover attributable to self-reported burnout and associated financial burden: a case study. BMC Health Serv Res 2018;18:851.
Willard-Grace R, Knox M, Huang B, Hammer H, Kivlahan C, Grumbach K. Burnout and health care workforce turnover. Ann Fam Med 2019;17:36-41.
Panagioti M, Geraghty K, Johnson J, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med 2018;178:1317-31.
Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002;136:358-67.
Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg 2010;251:995-1000.
Tawfik DS, Profit J, Morgenthaler TI, et al. Physician burnout, well-being, and work unit safety grades in relationship to reported medical errors. Mayo Clin Proc 2018;93:1571-80.
Williams ES, Manwell LB, Konrad TR, Linzer M. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev 2007;32:203-12.
Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med 2019;170:784-90.
Elliott DJ, Young RS, Brice J, Aguiar R, Kolm P. Effect of hospitalist workload on the quality and efficiency of care. JAMA Intern Med 2014;174:786-93.
Michtalik HJ, Pronovost PJ, Marsteller JA, Spetz J, Brotman DJ. Identifying potential predictors of a safe attending physician workload: a survey of hospitalists. J Hosp Med 2013;8:644-6.
Ripp J, Peccoralo L, Charney D. Attending to the emotional well-being of the health care workforce in a new york city health system during the COVID-19 pandemic. Acad Med 2020;95:1136-9.
Funding
Sagarika Arogyaswamy, BA, was supported by the Society of Hospital Medicine Student Hospitalist Scholar Grant
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arogyaswamy, S., Vukovic, N., Keniston, A. et al. The Impact of Hospital Capacity Strain: a Qualitative Analysis of Experience and Solutions at 13 Academic Medical Centers. J GEN INTERN MED 37, 1463–1474 (2022). https://doi.org/10.1007/s11606-021-07106-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07106-8