Abstract
Background
In this study, we used computed tomography (CT)-based radiomics signatures to predict the mutation status of KRAS in patients with colorectal cancer (CRC) and to identify the phase of radiomics signature with the most robust and high performance from triphasic enhanced CT.
Methods
This study involved 447 patients who underwent KRAS mutation testing and preoperative triphasic enhanced CT. They were categorized into training (n = 313) and validation cohorts (n = 134) in a 7:3 ratio. Radiomics features were extracted using triphasic enhanced CT imaging. The Boruta algorithm was used to retain the features closely associated with KRAS mutations. The Random Forest (RF) algorithm was used to develop radiomics, clinical, and combined clinical–radiomics models for KRAS mutations. The receiver operating characteristic curve, calibration curve, and decision curve were used to evaluate the predictive performance and clinical usefulness of each model.
Results
Age, CEA level, and clinical T stage were independent predictors of KRAS mutation status. After rigorous feature screening, four arterial phase (AP), three venous phase (VP), and seven delayed phase (DP) radiomics features were retained as the final signatures for predicting KRAS mutations. The DP models showed superior predictive performance compared to AP or VP models. The clinical–radiomics fusion model showed excellent performance, with an AUC, sensitivity, and specificity of 0.772, 0.792, and 0.646 in the training cohort, and 0.755, 0.724, and 0.684 in the validation cohort, respectively. The decision curve showed that the clinical–radiomics fusion model had more clinical practicality than the single clinical or radiomics model in predicting KRAS mutation status.
Conclusion
The clinical–radiomics fusion model, which combines the clinical and DP radiomics model, has the best predictive performance for predicting the mutation status of KRAS in CRC, and the constructed model has been effectively verified by an internal validation cohort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the second leading cause of cancer-related deaths worldwide and causes almost 881,000 deaths every year [1]. The incidence of colorectal cancer is approximately threefold higher in developed countries than in developing countries. However, as the developing countries become richer, increasing trends are likely to be seen [2]. The Kirsten rat sarcoma (KRAS) viral oncogene homolog is a G protein, which occurs in 40–50% cases of CRCs. Following a mutation in the KRAS gene, the mutant protein activates the downstream mitogen-activated protein kinase (MAPK) pathway, subsequently leading to uncontrolled cell proliferation and malignancy [3]. The National Comprehensive Cancer Network (NCCN) clinical practice guidelines have explicitly indicated that patients with CRC and KRAS mutations are resistant to anti-EGFR monoclonal antibody therapy [4]. Therefore, KRAS mutation testing is crucial for individualized and effective treatment of CRC.
Generally, pathologic specimens obtained via invasive procedures, such as colonoscopy and surgery, are usually required for the identification of KRAS mutation status. However, the presence of extensive heterogeneity in CRC archival samples represents a major limitation of the histological approach [5]. Additionally, tissue specimens for genetic testing cannot be obtained for selected patients with metastatic CRC because they cannot undergo surgical treatment [6]. Furthermore, biopsy testing might not be an effective approach to determine the mutational status of KRAS due to poor DNA quality [7]. Therefore, it is necessary to develop a non-invasive and easy-to-use method to identify KRAS mutation status.
Several studies have demonstrated the use of medical imaging technology, such as fluorine-18 fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) and magnetic resonance imaging, in the prediction of KRAS status [8, 9]. However, these studies involved small sample sizes and lacked validation. Radiomics provide a variety of parameters for quantitative analysis, which have been widely used in cancer diagnosis, classification, and prediction [10]. A previous study demonstrated a significant correlation between a CT-based radiomics signature and KRAS/NRAS/BRAF mutations in patients with CRC [11]. However, this study involved a small sample size and was only performed in the venous phase (VP). Moreover, the superiority of VP compared to the arterial phase (AP) or delay phase (DP) in the prediction of KRAS mutation status in patients with CRC remains to be confirmed. The aim of this study was to investigate whether a CT-based radiomics signature could identify KRAS mutation status in patients with CRC and whether the VP is superior to arterial and delay phases in the prediction of KRAS mutation status in patients with CRC.
Materials and methods
Patients
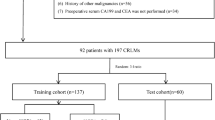
Ethical approval has been obtained by this retrospective study, and the informed consent requirement was waived. For the primary cohort of this study, we analyzed the institutional database in Lanzhou University Second Hospital between March 2014 and June 2020 to identify eligible patients with confirmed cases of CRC who underwent curative resection. A total of 447 patients met the inclusion criteria in our study, which were set based on the following factors: (1) pathologically identified cases of primary CRC adenocarcinoma; (2) patients who underwent KRAS mutation status testing prior to the treatment; and (3) pre-treatment abdominal triphasic enhanced CT with a reconstruction slice thickness of 1.25 mm. The exclusion criteria were set based on the following factors: (1) abdominal triphasic enhanced CT was not performed before surgery or the interval between abdominal triphasic enhanced CT and surgery was > 2 weeks; (2) patients with CRC who have received any anticancer treatment prior to the collection of pathological tissue samples; (3) insufficient CT quality for qualitative and quantitative analyses; (4) incomplete clinical information; and (5) occurrence of intussusception in the area where the tumor was located. Figure 1 shows a flow diagram of the recruitment pathway. Patients were categorized into training and validation cohorts in the ratio 7:3.
Clinicopathological characteristics and semantic features
Baseline clinicopathological characteristics data that were collected from medical records included age, sex, tumor location, KRAS mutation status, CEA level (threshold value ≥ 5 ng/mL, < 5 ng/mL), CA125 level (threshold value ≥ 35 U/mL, < 35 U/mL), and CA19-9 level (threshold value ≥ 37 U/mL, < 37 U/mL). Two experienced gastrointestinal radiologists (Y T C and J Z) analyzed the CT images (including tumor location, maximum diameter, clinical tumor (cT) stage, and clinical node (cN) stage). Both radiologists were blinded to the patient’s clinicopathological data. To minimize bias, qualitative data were obtained three times and the average was calculated; qualitative data were independently evaluated and resolved through consultation when opinions were inconsistent. The maximum tumor thickness was defined as the maximum diameter perpendicular to the long axis of the cross-sectional image. The cT and cN stages were identified according to the eighth edition of the American Joint Committee on Cancer Staging System [12].
KRAS mutation status evaluation
Formalin-fixed tumor tissue samples were obtained following CRC surgeries and confirmed that the specimens used to extract DNA are clearly infiltrated by the tumor. KRAS mutation status (exons 2, 3, and 4) was detected via polymerase chain reaction (PCR).
CT image acquisition and segmentation
Abdominal triphasic enhanced CT scans were performed on a Discovery CT 750 HD scanner (GE Healthcare, Waukesha, WI) and an iCT 256 scanner (Philips, Amsterdam, Netherlands). The scanning parameters are listed in Supplementary Table S1. Enhanced CT scanning was performed using a high-pressure dual-cylinder syringe to inject intravenous iohexol (1 mL/kg) through the median cubital vein with an injection rate of 3.5–4.5 mL/second. Following the injection of the contrast medium, AP, VP, and DP were scanned at 25–30 s, 60–70 s, and 120–150 s, respectively.
The original images of AP, VP, and DP were stored in the corresponding folders in DICOM format. Two gastrointestinal radiologists (reader 1: Y T C and reader 2: J Z) performed three-dimensional (3D) radiomics segmentation on AP, VP, and DP images using ITK-SNAP software (version 3.6.0; www.itksnap.org). Reader 1 segmented 247 cases and reader 2 segmented the other 200 cases.
For 3D radiomics segmentation, the ROI was manually delineated on each slice of the tumor. Air and feces in the intestinal tract and pericolonic fat were carefully excluded from the contours (Fig. 2). Finally, each patient generated three ROIs (AP ROI, VP ROI, and DP ROI). To evaluate the inter-observer reproducibility and robustness of the feature extraction, reader 1 and reader 2 randomly selected 30 patients and performed manual segmentation. We estimated the reproducibility of the feature extraction using intra-/inter-class correlation coefficients (ICCs); ICC values greater than 0.80 indicate good reproducibility [13]. Additionally, 30 patients were randomly selected from each CT scanner to build the CT scanners set for calculating the ICCs.
Workflow of KRAS prediction building and analysis. The tumors were segmented on arterial phase (A, B), delayed phase (C, D) and venous phase (E, F) CT images to form volumes of interest (VOIs). One thousand and thirty-seven quantitative radiomics features were extracted from each patient. The least absolute shrinkage and selection operator (LASSO) was used to select the features. Multivariate logistic regression was used to build radiomics, clinical, and clinicoradiomics combined models for KRAS prediction. Finally, the radiomics signature and clinical factors were incorporated into a nomogram for individual evaluation. Receiver operating characteristic curves were used to evaluate the clinical usefulness of the nomogram
Feature extraction
Radiomics features were extracted and selected using PyRadiomics software [14]. Seven classes of radiomics features (first-order histogram, 3D morphologic, gray level co-existence matrix (GLCM), gray level range-matrix (GLRM), gray level size zone matrix (GLSZM), neighboring grey tone difference matrix (NGTDM), and grey level dependence matrix (GLDM) features) were extracted from original and filtered images (wavelet and Laplacian of Gaussian). Finally, 1037 3D radiomics features were extracted from each phase of the triphasic enhanced CT. The specific definitions and descriptions of the features are demonstrated in the Supplementary Materials.
Feature selection and radiomics prediction model building
After radiomics features extraction, all missing data in the training cohort were replaced by the median value and z-score normalization was performed on each feature; the same preprocessing procedure was applied to the validation cohort. After preprocessing of the features, the most important features were selected to predict KRAS mutations using a three-step procedure. First, univariate analysis was performed for feature selection to retain the feature with P < 0.05 to enter the following process. Second, the Boruta method [15] was used to retain the features that closely associated with KRAS mutations. Finally, multivariable stepwise regression further eliminated irrelevant features and retained the most informative features. A ten times fivefold cross-validation was applied to avoid overfitting and identify the model with the best performance.
Three radiomics models (AP, VP, and DP model) were established based on the above radiomics signatures in triphasic enhanced CT phase images. For example, the VP model was built based on VP features in 3D segmentation patterns (three features). Further, the 3D-combined model was built based on AP, VP, and DP fusion features in 3D segmentation patterns (11 features).
Clinical and combined model construction
For clinical and imaging characteristics, the Chi-squared test or Fisher’s exact test were used to compare the differences in sex, tumor location, CEA, CA125, CA19-9, cT stage, and cN stage, whereas the Student’s t test or Mann–Whitney U test was used to compare the differences in age and maximum diameter between mutated KRAS and wild-type KRAS groups in the training cohorts. We performed multivariable analyses to identify the most important features. A clinical model was established based on the inclusion of selected features.
A clinical–radiomics fusion model was developed based on correlated clinical risk factors, strongly correlated imaging characteristics, and radiomics features to verify whether the combination of radiomics signatures and clinical factors could improve performance in the prediction of KRAS mutations. Two steps were followed to build the fusion model in this study. First, AP, VP, and DP models were compared to determine the enhancement phase with the best KRAS mutation prediction performance. Second, the Random Forest (RF) algorithm was used to combine clinical factors, imaging characteristics, and the radiomics features of the best predictive performance phase to construct a clinical–radiomics fusion model in the training cohort, and the discrimination ability of the fusion model was evaluated based on the AUC value in the validation cohort.
Statistical analysis
All statistical analyses were conducted using the R statistical software package (version 3.6.3; http://www.Rproject.org). The Student’s t test, Mann–Whitney U test, and Chi-squared test or Fisher’s exact test were used to compare continuous and categorical variables, as appropriate. A two-sided P value < 0.05 was considered statistically significant. The ICCs were used to calculate the consistency of measurements between the two radiologists and the different CT scanners. ROC analysis was used to evaluate the predictive accuracy of the different models. The AUC value, 95% confidence interval (CI), accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were also calculated. A calibration curve was constructed to assess the goodness-of-fit of the models. To verify the clinical usefulness of the models, we quantified the net benefit at different threshold probabilities in the dataset using DCA curves.
Results
Clinical characteristics
This study involved a total of 447 patients with CRC in the final analysis, including 263 men (58.8%) and 184 women (41.2%), with an average age of 58.93 ± 12.85 years. Among the 447 patients, 207 had mutated KRAS and 240 had wild-type KRAS. We used stratified sampling to categorize the study cohort into training (n = 313) and validation (n = 134) cohorts in a 7:3 ratio. The training and validation cohorts were used for model building and internal validation, respectively. Patient and tumor characteristics in the training cohort are listed in Table 1.
Predictive performance of the clinical model
In the training cohort, the clinical characteristics age, CEA, CA19-9, and cT stage were found to be significantly different statistically (P < 0.05), and the other characteristics not significantly different (P > 0.05) between mutated KRAS and wild-type KRAS groups (Table 1). After multivariate analyses, clinical characteristics including age, CEA, and cT stage were selected as independent predictors of KRAS mutation and enrolled into clinical model. The clinical model showed lower performance in predicting KRAS mutation both in the training cohort and the validation cohort, with the AUC being 0.654 (95% CI 0.593–0.714) in the training cohort and 0.575 (95% CI 0.478–0.672) in the validation cohort (Table 2). The accuracy, sensitivity, and specificity were 0.617, 0.664, and 0.573 (training cohort) and 0.552, 0.552, and 0.553 (validation cohort), respectively.
Radiomics signature building and discrimination performance assessment
The ICCs were calculated to evaluate the agreement of features extracted by two radiologists and different CT scanners; all values > 0.80 indicate good agreement. A total of 1037 3D radiomics features were extracted from each patient's AP, VP, and DP images. Finally, four, three, and seven radiomics features were selected as the final signatures. The feature names and distributions are listed in Table 3. Following stepwise regression analysis, three features were removed after combining the AP, VP, and DP radiomics features. Four models were built based on the above radiomics signatures for preoperatively predicting KRAS mutations. The AUC, accuracy, sensitivity, specificity, PPV, and NPV are listed in Table 2. The DP model had the most optimal predictive performance compared to the AP or VP model in both the training and validation cohorts (Fig. 3A, B, Table 2). In the training cohort, the predictive AUC of KRAS mutations in AP, VP, and DP models were 0.711, 0.692, and 0.752, respectively. In the validation cohort, the AUC of the three models were 0.723, 0.673, and 0.746, respectively. The radiomics model combined with the triphasic enhanced CT phases showed moderate KRAS mutation prediction performance, with an AUC, accuracy, sensitivity, specificity, PPV, and NPV of 0.754, 0.700, 0.738, 0.665, 0.667, and 0.736 in the training cohort, respectively, whereas the AUC, accuracy, sensitivity, specificity, PPV, and NPV in the validation cohort were 0.775, 0.701, 0.707, 0.697, 0.641, and 0.757, respectively (Fig. 3A, B, Table 2).
ROC curves of the different models in training (A) and validation cohorts (B). AUC area under the curve, A radiomics model of arterial phase, D radiomics model of delayed phase, V radiomics model of venous phase, Radiomics radiomics model of fusion of arterial phase, delayed phase and venous phase features, COMB fusion of clinical risk factors and radiomics features of delayed phase
Predictive performance of the combined model
As shown in Table 2 and Fig. 3, we developed a clinical–radiomics model incorporating three clinical factors (age, CEA, and cT stage) and seven DP radiomics signatures. The clinical–radiomics model showed excellent predictive ability for KRAS mutations. The clinical–radiomics fusion model showed superior predictive performance for KRAS mutations compared to either the clinical model or the radiomics model alone; the AUC values of the clinical–radiomics model were 0.772 (95% CI 0.720–0.823) in the training cohort and 0.755 (95% CI 0.674–0.836) in the validation cohort. The calibration curve of each model showed favorable agreement between prediction and observation in predicting the risk of KRAS mutations (Fig. 4A, B).
Calibration curves of the different models in training (A) and validation cohorts (B). A radiomics model of arterial phase, D radiomics model of delayed phase, V radiomics model of venous phase, Radiomics radiomics model of fusion of arterial phase, delayed phase and venous phase features, COMB fusion of clinical risk factors and radiomics features of delayed phase
The DCA curves for the clinical model, radiomics model, and clinical–radiomics model are presented in Fig. 5A, B. The clinical–radiomics model achieved more clinical utility in predicting KRAS mutations than the clinical model and other radiomics models. The DCA curves of the clinical–radiomics model demonstrated that when the threshold probability of a patient or doctor ranged between 20 and 65%, the use of the clinical–radiomics nomogram adds greater benefit for KRAS mutation prediction than the treat-all-patients scheme or the treat-none scheme in the training and validation cohorts.
Decision curve analysis of different models in training (A) and validation cohorts (B). A radiomics model of arterial phase, D radiomics model of delayed phase, V radiomics model of venous phase, Radiomics radiomics model of fusion of arterial phase, delayed phase and venous phase features, COMB fusion of clinical risk factors and radiomics features of delayed phase
Discussion
In this study, clinical, radiomics, and clinical–radiomics models were developed for the preoperative prediction of KRAS mutations. We verified our hypothesis that the DP model had a higher predictive performance than the AP or VP models. Additionally, the clinical–radiomics model showed a higher predictive performance than the clinical or radiomics models alone. The calibration and decision curves of the clinical–radiomics model showed excellent model stability and actual benefit.
KRAS mutations can lead to continuous activation of the EGF/RAS/RAF/ERK signaling pathway without the regulation of EGFR, gradually leading to increased cell proliferation and decreased apoptosis [16,17,18]. Colorectal cancer with KRAS mutations is a negative marker for anti-EGFR targeted drugs [19]. Numerous studies have used 18F-FDG PET/CT to investigate the association between KRAS mutations and 18F-FDG uptake and demonstrated that cells with KRAS mutations had a higher 18F-FDG uptake than those with wild-type KRAS [20, 21]. However, there was no correlation observed between them according to a study by Riklis et al. [22]. The major clinical use of PET/CT in CRC is to detect potentially curable metastases. Yang et al. [11] proposed a CT-based radiomics model to identify KRAS/NRAS/BRAF mutations in CRC and found a relatively high predictive performance. However, this study defined the positive group based on mutations in any of KRAS/NARS/BRAF, which would complicate the clinical application.
In the present study, the clinical model constructed by clinicopathological factors has the ability to identify KRAS gene mutations. However, the diagnostic value of the clinical model was quite low. When the clinicopathological factors and DP radiomics features were combined as a clinical–radiomics model, the predictive AUC value of the clinical–radiomics model reached 0.772 in the training cohort and 0.755 in the validation cohort. Thus, the radiomics features can provide additional benefits in predicting KRAS mutations.
During the image preprocessing stage, the LoG and wavelet filters were applied to process the original image. The LoG filter can smoothen the image and improve the efficiency of capturing phenotypic features related to tumor heterogeneity [23]. The wavelet filter could disassemble the frequency signal of the image to extract edges and substantial features of the tumor more effectively. This study finally screened out 25 radiomics features as the radiomics signatures of the AP, VP, DP, and triphasic enhanced combined phase. The features with wavelet filtering accounted for 52% (13/25) of the total features. This shows that the wavelet filter is important for extracting features related to KRAS mutation status, whereas the features with LoG filters are not used as radiomics signatures for predicting KRAS mutations, indicating that the features extracted from the LoG filter images were weakly correlated with KRAS mutations.
Using multivariable regression analysis combined with the radiomics signatures of the triphasic enhanced phases, 11 radiomics features were retained as key features for identifying KRAS mutation status (Table 3), including 5 texture features: A_wavelet.HHH_glszm_GrayLevelNonUniformityNormalized, A_wavelet.LLL_glcm_MCC, D_wavelet.HLL_glcm_Idn, D_wavelet.HLL_gldm_SmallDendenceLowGrayLevelEmphasis, and D_wavelet.LLL_glcm_Idn. Texture features are microscopic tumor descriptions, which reflects the interaction between adjacent pixels as well as tumor heterogeneity [24]. These features are not easily identified by the human visual system and cannot be interpreted as having a clear meaning. Previous studies have shown that texture features may be associated with the tumor microenvironment reflecting tumor heterogeneity and the presence of hypoxia or angiogenesis [25,26,27]. A previous study found that KRAS mutations were associated with higher texture characteristic values (Gskewness and SDs), indicating that mutated KRAS had more tumor heterogeneity than wild-type KRAS [28]. The radiomics score values of texture features (A_wavelet. LLL_glcm_MCC and D_wavelet. HLL_gldm_SmallDendenceLowGrayLevelEmphasis) in the KRAS mutation group were higher than that in the wild-type group, which suggests more tumor heterogeneity in the tumor tissue in the ROI range. The results of this study in combination with that of other studies shows that texture features can be used as non-invasive imaging markers for predicting KRAS mutations status.
In addition, five morphological features (A_original_shape_Elongation, V_original_shape_Maximum2DDiameterSlice, D_original_shape_Elongation, D_original_shape_Maximum3DDiameter, and D_original_shape_Sphericity) were closely correlated with KRAS mutations, suggesting that the morphological characteristics of mutant KRAS and wild-type KRAS tumors were significantly different, which is consistent with previous literatures. A previous study found that morphological features (elongation and flatness) were closely associated with KRAS mutations in rectal cancer [23]. Another study explored the correlation between KRAS mutations in rectal cancer and tumor morphology in magnetic resonance images, and found that the average axial/longitudinal ratio of KRAS mutations in rectal cancer was greater than that of KRAS wild-type tumors (0.46 ± 0.29 vs. 0.36 ± 0.20, P = 0.009) [9].
Among the triphasic enhanced phase models of KRAS mutation prediction in the training cohort, the DP model showed the highest performance, with an AUC value of 0.752, followed by 0.711 in the AP model and 0.692 in the VP model. To our knowledge, this is the first time that triphasic enhanced CT radiomics has been used in KRAS mutation prediction. Although the VP is the most commonly used phase in gastrointestinal radiomics research, contrary to the results observed in this study, the enhancement phase with the best predictive performance was the DP rather than the VP phase. The high predictive performance of the DP model might be due to the possibility of high content and uniform distribution of the contrast agent in the DP lesions or because the ROI range of tumors in the DP images is larger than that in the AP and VP images [29].
In terms of clinical characteristics, age, CEA, and CA19-9 were independent predictors for KRAS mutations. In this study, patients with KRAS mutations were significantly older than those with KRAS wild-type P < 0.05, which is consistent with the findings of a previous study [30]. CEA and CA19-9 were significantly higher for the mutated KRAS group than for the wild-type KRAS group in our study, which is in line with findings from previous studies [31, 32]. Both KRAS mutations and elevated serum levels of CEA and CA19-9 are associated with more aggressive biological behavior in patients with CRC [33,34,35]. A correlation between KRAS mutations and higher CEA and CA19-9 levels suggests that genetic alterations may have independent influences on CRC development, thus resulting in increased tumor biomarkers [36].
Triphasic enhanced CT is often conducted in CT examination of gastrointestinal tumors. The AP is used for tumor detection, the VP to differentiate the tumor from adjacent organs, and the DP to determine the depth of tumor invasion [37]. As for radiation dose, the average DLP value of triphasic enhanced scans was 1917.52 ± 152.31 mGy cm, which is slightly higher than the diagnostic reference level for adults (1490 mGy cm) published by China's National Health Industry standard (WS/T 637-2018) [38]. Application of new techniques such as multi-model iterative reconstruction technology could effectively reduce the radiation dose in clinical practice [39].
Our study should be interpreted after considering several limitations. First, 269 patients were excluded because they did not meet the inclusion and exclusion criteria, which inevitably produced a selection bias. Second, our study only included a single team with an internal validation cohort. The reproducibility should be addressed in future multi-center studies. Third, due to the irregular shape of some tumors, the ROI delineation process is difficult and time consuming. In future studies, it will be necessary to develop an automated or semi-automated tool to achieve effective and automatic tumor segmentation. Finally, we used different imaging instruments and acquisition parameters to complete the CT scanning. The influence of different instruments and different parameters on radiomics features is obvious. Therefore, it is important to standardize scanning protocols in different instruments and different institutions.
Conclusion
In conclusion, triphasic enhanced CT radiomics models were constructed to predict KRAS mutation status in colorectal cancer, and the results showed that the AP, VP, and DP models could better predict KRAS mutation status in the training and validation cohorts. The DP model showed a higher predictive performance compared to the AP or VP models. Additionally, the clinical–radiomics model, which incorporates both clinical risk factors and radiomics features of DP images, showed good performance in predicting KRAS mutations. The clinical–radiomics fusion model can be used as a potential imaging marker for preoperative detection of KRAS mutation status and guide the selection of molecular targeted drug therapy for CRC.
Abbreviations
- AP:
-
Arterial phase
- CRC:
-
Colorectal cancer
- DP:
-
Delayed phase
- KRAS :
-
Kirsten rat sarcoma
- VP:
-
Venous phase
- 3D:
-
Three-dimensional
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394:1467–80.
De Roock W, Claes B, Bernasconi D, De Schutter J, Biesmans B, Fountzilas G, Kalogeras KT, Kotoula V, Papamichael D, Laurent-Puig P, Penault-Llorca F, Rougier P, Vincenzi B, Santini D, Tonini G, Cappuzzo F, Frattini M, Molinari F, Saletti P, De Dosso S, Martini M, Bardelli A, Siena S, Sartore-Bianchi A, Tabernero J, Macarulla T, Di Fiore F, Gangloff AO, Ciardiello F, Pfeiffer P, Qvortrup C, Hansen TP, Van Cutsem E, Piessevaux H, Lambrechts D, Delorenzi M, Tejpar S. Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol. 2010;11:753–62.
Van Cutsem E, Lenz HJ, Köhne CH, Heinemann V, Tejpar S, Melezínek I, Beier F, Stroh C, Rougier P, van Krieken JH, Ciardiello F. Fluorouracil, leucovorin, and irinotecan plus cetuximab treatment and RAS mutations in colorectal cancer. J Clin Oncol. 2015;33:692–700.
Watanabe T, Kobunai T, Yamamoto Y, Matsuda K, Ishihara S, Nozawa K, Iinuma H, Shibuya H, Eshima K. Heterogeneity of KRAS status may explain the subset of discordant KRAS status between primary and metastatic colorectal cancer. Dis Colon Rectum. 2011;54:1170–8.
Sundström M, Edlund K, Lindell M, Glimelius B, Birgisson H, Micke P, Botling J. KRAS analysis in colorectal carcinoma: analytical aspects of Pyrosequencing and allele-specific PCR in clinical practice. BMC Cancer. 2010;10:660.
Wang S, Shi J, Ye Z, Dong D, Yu D, Zhou M, Liu Y, Gevaert O, Wang K, Zhu Y, Zhou H, Liu Z, Tian J. Predicting EGFR mutation status in lung adenocarcinoma on computed tomography image using deep learning. Eur Respir J. 2019;53:1800986.
Lovinfosse P, Polus M, Van Daele D, Martinive P, Daenen F, Hatt M, Visvikis D, Koopmansch B, Lambert F, Coimbra C, Seidel L, Albert A, Delvenne P, Hustinx R. FDG PET/CT radiomics for predicting the outcome of locally advanced rectal cancer. Eur J Nucl Med Mol Imaging. 2018;45:365–75.
Shin YR, Kim KA, Im S, Hwang SS, Kim K. Prediction of KRAS mutation in rectal cancer using MRI. Anticancer Res. 2016;36:4799–804.
He K, Liu X, Li M, Li X, Yang H, Zhang H. Noninvasive KRAS mutation estimation in colorectal cancer using a deep learning method based on CT imaging. BMC Med Imaging. 2020;20:59.
Yang L, Dong D, Fang M, Zhu Y, Zang Y, Liu Z, Zhang H, Ying J, Zhao X, Tian J. Can CT-based radiomics signature predict KRAS/NRAS/BRAF mutations in colorectal cancer? Eur Radiol. 2018;28:2058–67.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, Meyer L, Gress DM, Byrd DR, Winchester DP. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67:93–9.
Aerts HJ, Velazquez ER, Leijenaar RT, Parmar C, Grossmann P, Carvalho S, Bussink J, Monshouwer R, Haibe-Kains B, Rietveld D, Hoebers F, Rietbergen MM, Leemans CR, Dekker A, Quackenbush J, Gillies RJ, Lambin P. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun. 2014;5:4006.
Van Griethuysen JJM, Fedorov A, Parmar C, Hosny A, Aucoin N, Narayan V, Beets-Tan RGH, Fillion-Robin JC, Pieper S, Aerts HJWL. Computational radiomics system to decode the radiographic phenotype. Cancer Res. 2017;77:e104–7.
Degenhardt F, Seifert S, Szymczak S. Evaluation of variable selection methods for random forests and omics data sets. Brief Bioinform. 2019;20:492–503.
Chu E. An update on the current and emerging targeted agents in metastatic colorectal cancer. Clin Colorectal Cancer. 2012;11(1):1–13.
Berthélemy P, Bouisson M, Escourrou J, Vaysse N, Rumeau JL, Pradayrol L. Identification of K-ras mutations in pancreatic juice in the early diagnosis of pancreatic cancer. Ann Intern Med. 1995;123:188–91.
Van Laethem JL, Vertongen P, Deviere J, Van Rampelbergh J, Rickaert F, Cremer M, Robberecht P. Detection of c-Ki-ras gene codon 12 mutations from pancreatic duct brushings in the diagnosis of pancreatic tumours. Gut. 1995;36:781–7.
Karapetis CS, Khambata-Ford S, Jonker DJ, O’Callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD, Robitaille S, Price TJ, Shepherd L, Au HJ, Langer C, Moore MJ, Zalcberg JR. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359:1757–65.
Chen SW, Chiang HC, Chen WT, Hsieh TC, Yen KY, Chiang SF, Kao CH. Correlation between PET/CT parameters and KRAS expression in colorectal cancer. Clin Nucl Med. 2014;39:685–9.
Cho A, Jo K, Hwang SH, Lee N, Jung M, Yun M, et al. Correlation between KRAS mutation and F-FDG uptake in stage IV colorectal cancer. Abdom Radiol (NY). 2017;42:1621–6.
Krikelis D, Skoura E, Kotoula V, Rondogianni P, Pianou N, Samartzis A, Xanthakis I, Fountzilas G, Datseris IE. Lack of association between KRAS mutations and 18F-FDG PET/CT in Caucasian metastatic colorectal cancer patients. Anticancer Res. 2014;34:2571–9.
Cui Y, Liu H, Ren J, Du X, Wang D. Development and validation of a MRI based radiomics signature for prediction of KRAS mutation in rectal cancer. Eur Radiol. 2020;30(4):1948–58.
Liu H, Zhang C, Wang L, Luo R, Li J, Zheng H, Yin Q, Zhang Z, Duan S, Li X, Wang D. MRI radiomics analysis for predicting preoperative synchronous distant metastasis in patients with rectal cancer. Eur Radiol. 2019;29:4418–26.
Lubner MG, Smith AD, Sandrasegaran K, et al. CT texture analysis: definitions, applications, biologic correlates, and challenges. Radiographics. 2017;37(5):1483–503.
Ganeshan B, Panayiotou E, Burnand K, Dizdarevic S, Miles K. Tumour heterogeneity in non-small cell lung carcinoma assessed by CT texture analysis: a potential marker of survival. Eur Radiol. 2012;22(4):796–802.
Bashir U, Siddique MM, Mclean E, Goh V, Cook GJ. Imaging heterogeneity in lung cancer: techniques, applications, and challenges. AJR Am J Roentgenol. 2016;207(3):534–43.
Oh JE, Kim MJ, Lee J, Hur BY, Kim B, Kim DY, Baek JY, Chang HJ, Park SC, Oh JH, Cho SA, Sohn DK. Magnetic resonance-based texture analysis differentiating KRAS mutation status in rectal cancer. Cancer Res Treat. 2020;52:51–9.
Cao Y, Zhang G, Zhang J, et al. Predicting microsatellite instability status in colorectal cancer based on triphasic enhanced computed tomography radiomics signatures: a multicenter study. Front Oncol. 2021;11: 687771.
Fu X, Huang Y, Fan X, et al. Demographic trends and KRAS/BRAF mutations in colorectal cancer patients of South China: a single-site report. Int J Cancer. 2019;144:2109–17.
Selcukbiricik F, Bilici A, Tural D, Erdamar S, Soyluk O, Buyukunal E, Demirelli F, Serdengecti S. Are high initial CEA and CA 19–9 levels associated with the presence of K-ras mutation in patients with metastatic colorectal cancer? Tumour Biol. 2013;34:2233–9.
Li W, Qiu T, Ling Y, Guo L, Li L, Ying J. Molecular pathological epidemiology of colorectal cancer in Chinese patients with KRAS and BRAF mutations. Oncotarget. 2015;6:39607–13.
Li W, Qiu T, Zhi W, Shi S, Zou S, Ling Y, Shan L, Ying J, Lu N. Colorectal carcinomas with KRAS codon 12 mutation are associated with more advanced tumor stages. BMC Cancer. 2015;15:340.
Bazan V, Agnese V, Corsale S, Calò V, Valerio MR, Latteri MA, Vieni S, Grassi N, Cicero G, Dardanoni G, Tomasino RM, Colucci G, Gebbia N, Russo A, Gruppo Oncologico dell’Italia Meridionale (GOIM). Specific TP53 and/or Ki-ras mutations as independent predictors of clinical outcome in sporadic colorectal adenocarcinomas: results of a 5-year Gruppo Oncologico dell’Italia Meridionale (GOIM) prospective study. Ann Oncol. 2005;16(Suppl 4):iv50-5.
Li M, Zhang J, Dan Y, Yao Y, Dai W, Cai G, Yang G, Tong T. A clinical-radiomics nomogram for the preoperative prediction of lymph node metastasis in colorectal cancer. J Transl Med. 2020;18:46.
Jeon C-H, Lee H-I, Shin I-H, Park J-W. Genetic alterations of APC, K-ras, p53, MSI, and MAGE in Korean colorectal cancer patients. Int J Colorectal Dis. 2008;23:29–35.
Lee JH, Jeong YK, Kim DH, Go BK, Woo YJ, Ham SY, Yang SO. Two-phase helical CT for detection of early gastric carcinoma: importance of the mucosal phase for analysis of the abnormal mucosal layer. J Comput Assist Tomogr. 2000;24:777–82.
Cao Y, Zhang G, Bao H, et al. Development of a dual-energy spectral CT based nomogram for the preoperative discrimination of mutated and wild-type KRAS in patients with colorectal cancer. Clin Imaging. 2021;69:205–12.
Jia Y, Zhai B, He T, Yu Y, Yu N, Duan H, Yang C, Zhang X. The application of a new model-based iterative reconstruction in low-dose upper abdominal CT. Acad Radiol. 2019;26:e275–83.
Acknowledgements
None.
Funding
This study received funding from the National Natural Science Foundation of China (82260346), Qinghai Provincial Department of science and technology of China (2023-ZJ-918M); Qinghai Province "Kunlun Talents High-end Innovation and Entrepreneurial Talents" Top Talent Cultivation Project; Doctoral research start-up fund project of Zunyi Medical University (BS2021-03); The Sichuan Academy of Medical Sciences & Sichuan Provincial People's Hospital Research Fund (No. 2022QN25).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The clinical institutional review board approved this study, and the need for informed consent requirement was waived owing to the retrospective nature of the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Cao, Y., Zhang, J., Huang, L. et al. Construction of prediction model for KRAS mutation status of colorectal cancer based on CT radiomics. Jpn J Radiol 41, 1236–1246 (2023). https://doi.org/10.1007/s11604-023-01458-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-023-01458-3