Abstract
Purpose
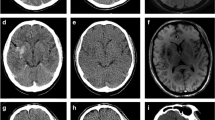
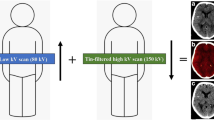
Acute ischemic stroke is currently among the main causes of mortality in Western countries. The current guidelines suggest different flowcharts of diagnostic work-up and treatment modalities, including endovascular thrombectomy. Immediately after intra-arterial recanalization, a brain CT scan is usually performed to assess for the presence of peri-procedural complications; in this setting, it is very hard, if possible, to differentiate blood from iodinated contrast material, which is normally present in ischemic tissue because of BBB disruption. Dual-energy CT may be used for this purpose, exploiting its ability to discriminate different materials.
Materials and methods
We retrospectively studied 44 patients with acute ischemic stroke who were treated with endovascular recanalization at San Giovanni Bosco Hospital in Turin and were then scanned with DECT technology. Subsequent scan was used as standard, since iodine from contrast staining is usually reabsorbed in 24 h and blood persists longer. A χ2 test of independence was performed to examine the relationship between blood detected by DECT scan after the endovascular procedure and the presence of blood in the same areas on the following scans, with a significant result: χ2 (1, N = 37) = 10.7086, p = 0.0010.
Results
Patients with blood detected on DECT scans had a double chance of having hemorrhagic infarction in follow-up scans, (RR 2.02). The sensitivity and specificity of DECT were respectively 70% and 90%, with an overall diagnostic accuracy of 76% and a positive and negative predictive value, respectively, of 95% and 53%.
Conclusion
Dual-energy CT scan after endovascular recanalization in ischemic stroke identifies early hemorrhagic infarction with excellent specificity and good overall diagnostic accuracy, representing a reliable diagnostic tool in everyday clinical practice.







Similar content being viewed by others
References
Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG et al (2021) Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 20(10):795–820
Leira EC, Muir KW (2019) EXTEND trial: towards a more inclusive but complex thrombolysis. Stroke 50(9):2637–2639
Thomalla G, Simonsen CZ, Boutitie F, Andersen G, Berthezene Y, Cheng B et al (2018) MRI-guided thrombolysis for stroke with unknown time of onset. N Engl J Med 379(7):611–622
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378(1):11–21
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378(8):708–718
Amans M et al (2014) Contrast staining on CT after DSA in ischemic stroke patients progresses to infarction and rarely hemorrhages. Interv Neuroradiol 20(1):106–115
Nakano S, Iseda T, Yoneyama T et al (2006) Early CT signs in patients with acute middle cerebral artery occlusion: incidence of contrast staining and haemorrhagic transformations after intra-arterial reperfusion therapy. Clin Radiol 61(2):156–162
McCollough CH, Leng S, Yu L, Fletcher JG (2015) Dual- and multi-energy CT: principles, technical approaches, and clinical applications. Radiology 276(3):637–653
Parakh A, Lennartz S, An C, Rajiah P, Yeh BM, Simeone FJ et al (2021) Dual-energy CT images: pearls and pitfalls. Radiographics 41(1):98–119
Kawamoto S, Fuld MK, Laheru D, Huang P, Fishman EK (2018) Assessment of iodine uptake by pancreatic cancer following chemotherapy using dual-energy CT, vol 43. Springer, New York, pp 445–456
George E, Wortman JR, Fulwadhva UP, Uyeda JW, Sodickson AD (2017) Dual energy CT applications in pancreatic pathologies. Br J Radiol 90:20170411
Gupta S, Wagner-Bartak N, Jensen CT, Hui A, Wei W, Lertdilok P et al (2016) Dual-energy CT of pancreatic adenocarcinoma: reproducibility of primary tumor measurements and assessment of tumor conspicuity and margin sharpness. Abdom Radiol 41(7):1317–1324
Noda Y, Goshima S, Miyoshi T, Kawada H, Kawai N, Tanahashi Y et al (2018) Assessing chemotherapeutic response in pancreatic ductal adenocarcinoma: Histogram analysis of iodine concentration and CT number in single-source dual-energy CT. American journal of roentgenology. American Roentgen Ray Society, Virginia, pp 1221–1226
Hidas G, Eliahou R, Duvdevani M, Coulon P, Lemaitre L, Gofrit ON et al (2010) Determination of renal stone composition with dual-energy CT: in vivo analysis and comparison with X-ray diffraction. Radiology 257(2):394–401
Dawoud MM, Dewan KAAWA, Zaki SA, Sabae MAAR (2017) Role of dual energy computed tomography in management of different renal stones. Egypt J Radiol Nucl Med 48(3):717–727
Ma C et al (2021) The feasibility of dual-energy CT to predict the probability of symptomatic intracerebral haemorrhage after successful mechanical thrombectomy. Clin Radiol 76:316.e9e316.e18
Mangesius S, Janjic T, Steiger R, Haider L, Rehwald R, Knoflach M et al (2021) Dual-energy computed tomography in acute ischemic stroke: state-of-the-art. Eur Radiol. https://doi.org/10.1007/s00330-020-07543-9
von Kummer R, Broderick JP, Campbell BCV, Demchuk A, Goyal M, Hill MD et al (2015) The heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke 46:2981–2986
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50:E344–E418
Li L, Huo M, Zuo T, Wang Y, Chen Y, Bao Y (2021) Prediction of intracerebral hemorrhage after endovascular treatment of acute ischemic stroke: combining quantitative parameters on dual-energy CT with clinical related factors. J Stroke Cerebrovasc Dis 30(10):106001
Djurdjevic T, Rehwald R, Knoflach M, Matosevic B, Kiechl S, Gizewski ER et al (2017) Prediction of infarction development after endovascular stroke therapy with dual-energy computed tomography. Eur Radiol 27(3):907–917
Almqvist H, Almqvist NS, Holmin S, Mazya MV (2020) Dual-energy CT follow-up after stroke thrombolysis alters assessment of hemorrhagic complications. Front Neurol 19:11
Postma AA, Das M, Stadler AAR, Wildberger JE (2015) Dual-energy CT: what the neuroradiologist should know, vol 3. Springer, New York
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The authors did not seek informed consent or ethical committee approval, for the following reasons: the paper does not report on primary research. All data analyzed were collected as part of routine diagnosis and treatment. Patients were diagnosed and treated according to national guidelines and agreements. The paper does not report on the use of experimental or new protocols. Our analysis looked retrospectively at outcomes for a cohort of patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pacielli, A., Vaudano, G.P., Bergamasco, L. et al. Assessment of post-thrombectomy brain hemorrhage in acute ischemic stroke with dual-energy CT: how reliable is it in clinical practice?. Radiol med 129, 575–584 (2024). https://doi.org/10.1007/s11547-023-01749-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-023-01749-9