Abstract
Background
The aim of the study was to provide radiologists and clinicians a rapid tool for assessment of intestinal inflammation in Crohn’s disease (CD) patients through quantification of diffusion-weighted imaging (DWI) signal intensity while performing magnetic resonance enterography (MRE).
Materials and methods
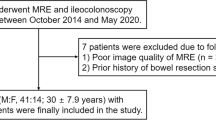
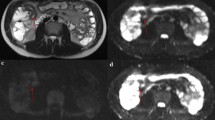
A monocentric retrospective study was conducted between September 2018 and July 2021 on CD patients who underwent MRE. Two radiologists measured signal intensity on DWI scans at the highest b-value (800 s/mm2) within pathologic intestinal walls, lymph nodes, spleen and psoas muscle and calculated the relative ratios. Spearman, Mann–Whitney and Jonckheere–Terpstra tests were applied for estimating correlation among ratios, significant differences between the two patient groups and determining the trend in relation to endoscopic classes. Wilcoxon’s and Cronbach’s alpha tests were employed for comparison of DWI measurements and ratios between the two observers.
Results
Fifty-nine patients were enrolled in the study. In the non-surgical group, correlation has been found among Simple Endoscopic Score for Crohn’s Disease (SES-CD) classes and the different ratios: bowel/spleen (p = 0.034), bowel/psoas (p = 0.008) and bowel/lymph node (p = 0.010).
Within the surgical group, positive correlation was found only between bowel/lymph node ratio and bowel/psoas ratio (p = 0.014). The J–T test demonstrated an increasing monotonic trend for bowel/psoas ratio and bowel/lymph node ratio and SES-CD classes. Inter-reader evaluation demonstrated no statistical differences for DWI measurements and high degree of concordance for the final ratios.
Conclusion
DWI ratios correlate with endoscopic classes in non-surgical patients and have inter-observer reproducibility.






Similar content being viewed by others
References
Feuerstein JD, Cheifetz AS (2017) Crohn disease: epidemiology, diagnosis, and management. Mayo Clin Proc 92(7):1088–1103. https://doi.org/10.1016/j.mayocp.2017.04.010
Leyendecker JR, Bloomfeld RS, DiSantis DJ, Waters GS, Mott R, Bechtold RE (2009) MR enterography in the management of patients with Crohn disease. Radiographics 29(6):1827–1846. https://doi.org/10.1148/rg.296095510
Cicero G, Mazziotti S (2020) Crohn’s disease at radiological imaging: focus on techniques and intestinal tract. Intest Res 19(4):365–378. https://doi.org/10.5217/ir.2020.00097
Cicero G, Ascenti G, Bottari A, Catanzariti F, Blandino A, Mazziotti S (2019) MR enterography: What is next after Crohn’s disease? Jpn J Radiol 37(7):511–517. https://doi.org/10.1007/s11604-019-00838-y
Lorusso F, Principi M, Pedote P, Pignataro P, Francavilla M, Sardaro A, Scardapane A (2021) Prevalence and clinical significance of incidental extra-intestinal findings in MR enterography: experience of a single University Centre. Radiol Med 126(2):181–188. https://doi.org/10.1007/s11547-020-01235-6
Kaushal P, Somwaru AS, Charabaty A, Levy AD (2017) MR enterography of inflammatory bowel disease with endoscopic correlation. Radiographics 37(1):116–131. https://doi.org/10.1148/rg.2017160064
Biondi M, Bicci E, Danti G, Flammia F, Chiti G, Palumbo P, Bruno F, Borgheresi A, Grassi R, Grassi F, Fusco R, Granata V, Giovagnoni A, Barile A, Miele V (2022) The role of magnetic resonance enterography in Crohn’s disease: a review of recent literature. Diagnostics (Basel) 12(5):1236. https://doi.org/10.3390/diagnostics12051236.PMID:35626391;PMCID:PMC9140029
Rimola J, Ordás I, Rodriguez S, García-Bosch O, Aceituno M, Llach J, Ayuso C, Ricart E, Panés J (2011) Magnetic resonance imaging for evaluation of Crohn’s disease: validation of parameters of severity and quantitative index of activity. Inflamm Bowel Dis 17(8):1759–1768. https://doi.org/10.1002/ibd.21551
Ordás I, Rimola J, Alfaro I, Rodríguez S, Castro-Poceiro J, Ramírez-Morros A, Gallego M, Giner À, Barastegui R, Fernández-Clotet A, Masamunt M, Ricart E, Panés J (2019) Development and validation of a simplified magnetic resonance index of activity for Crohn’s disease. Gastroenterology 157(2):432-439.e1. https://doi.org/10.1053/j.gastro.2019.03.051
Makanyanga JC, Pendsé D, Dikaios N, Bloom S, McCartney S, Helbren E, Atkins E, Cuthbertson T, Punwani S, Forbes A, Halligan S, Taylor SA (2014) Evaluation of Crohn’s disease activity: initial validation of a magnetic resonance enterography global score (MEGS) against faecal calprotectin. Eur Radiol 24:277–287. https://doi.org/10.1007/s00330-013-3010-z
Daperno M, D’Haens G, Van Assche G, Baert F, Bulois P, Maunoury V, Sostegni R, Rocca R, Pera A, Gevers A, Mary JY, Colombel JF, Rutgeerts P (2004) Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc 60(4):505–512. https://doi.org/10.1016/s0016-5107(04)01878-4
Hagmann P, Jonasson L, Maeder P, Thiran JP, Wedeen VJ, Meuli R (2006) Understanding diffusion MR imaging techniques: from scalar diffusion-weighted imaging to diffusion tensor imaging and beyond. Radiographics 26(Suppl 1):S205–S223. https://doi.org/10.1148/rg.26si065510
Minordi LM, Larosa L, Papa A, Cimino G, Bevere A, Brizi MG, Manfredi R (2021) A review of Magnetic Resonance Enterography classification and quantitative evaluation of active disease in patients with Crohn’s disease. Clin Imaging 69:50–62. https://doi.org/10.1016/j.clinimag.2020.06.006
Guimarães LS, Greer MC, Dillman JR, Fletcher JG (2020) Magnetic resonance in Crohn’s disease: diagnosis, disease burden, and classification. Magn Reson Imaging Clin N Am 28(1):31–44. https://doi.org/10.1016/j.mric.2019.08.003
Bruining DH, Zimmermann EM, Loftus EV Jr, Sandborn WJ, Sauer CG, Strong SA, Society of Abdominal Radiology Crohn’s Disease-Focused Panel (2018) Consensus recommendations for evaluation, interpretation, and utilization of computed tomography and magnetic resonance enterography in patients with small bowel Crohn’s disease. Radiology 286(3):776–799. https://doi.org/10.1148/radiol.2018171737
Oto A, Kayhan A, Williams JT, Fan X, Yun L, Arkani S, Rubin DT (2011) Active Crohn’s disease in the small bowel: evaluation by diffusion weighted imaging and quantitative dynamic contrast enhanced MR imaging. J Magn Reson Imaging 33(3):615–624. https://doi.org/10.1002/jmri.22435
Kiryu S, Dodanuki K, Takao H, Watanabe M, Inoue Y, Takazoe M, Sahara R, Unuma K, Ohtomo K (2009) Free-breathing diffusion-weighted imaging for the assessment of inflammatory activity in Crohn’s disease. J Magn Reson Imaging 29(4):880–886. https://doi.org/10.1002/jmri.21725
Oto A, Zhu F, Kulkarni K, Karczmar GS, Turner JR, Rubin D (2009) Evaluation of diffusion-weighted MR imaging for detection of bowel inflammation in patients with Crohn’s disease. Acad Radiol 16(5):597–603. https://doi.org/10.1016/j.acra.2008.11.009
Li XH, Sun CH, Mao R, Huang SY, Zhang ZW, Yang XF, Huang L, Lin JJ, Zhang J, Ben-Horin S, Feng ST, Chen MH, Li ZP (2017) Diffusion-weighted MRI enables to accurately grade inflammatory activity in patients of ileocolonic Crohn’s disease: results from an observational study. Inflamm Bowel Dis 23(2):244–253. https://doi.org/10.1097/MIB.0000000000001001
Seo N, Park SH, Kim KJ, Kang BK, Lee Y, Yang SK, Ye BD, Park SH, Kim SY, Baek S, Han K, Ha HK (2016) MR enterography for the evaluation of small-bowel inflammation in Crohn disease by using diffusion-weighted imaging without intravenous contrast material: a prospective noninferiority study. Radiology 278(3):762–772. https://doi.org/10.1148/radiol.2015150809
Petrie A, Sabin C (2020) Medical statistics at a glance, 4th edn. Wiley-Blackwell
Murakami H, Lee SK (2015) Unbiasedness and biasedness of the Jonckheere–Terpstra and the Kruskal–Wallis tests. J Korean Stat Soc 44:342–351. https://doi.org/10.1016/j.jkss.2014.10.001
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Cansu A, Bekircavusoglu S, Oguz S, Bulut E, Fidan S (2020) Can diffusion weighted imaging be used as an alternative to contrast-enhanced imaging on magnetic resonance enterography for the assessment of active inflammation in Crohn disease? Medicine (Baltimore) 99(8):e19202. https://doi.org/10.1097/MD.0000000000019202
Tielbeek JA, Ziech ML, Li Z, Lavini C, Bipat S, Bemelman WA et al (2014) Evaluation of conventional, dynamic contrast enhanced and diffusion weighted MRI for quantitative Crohn’s disease assessment with histopathology of surgical specimens. Eur Radiol 24(3):619–629. https://doi.org/10.1007/s00330-013-3015-7
Foti PV, Travali M, Farina R, Palmucci S, Coronella M, Spatola C, Puzzo L, Garro R, Inserra G, Riguccio G, Zanoli L, Basile A (2021) Can conventional and diffusion-weighted mr enterography biomarkers differentiate inflammatory from fibrotic strictures in Crohn’s disease? Medicina (Kaunas) 57(3):265. https://doi.org/10.3390/medicina57030265
Soydan L, Demir AA, Ozer S, Ozkara S (2019) Can MR enterography and diffusion-weighted imaging predict disease activity assessed by simple endoscopic score for Crohn’s disease? J Belg Soc Radiol 103(1):10. https://doi.org/10.5334/jbsr.1521
Freiman M, Perez-Rossello JM, Callahan MJ, Bittman M, Mulkern RV, Bousvaros A, Warfield SK (2013) Characterization of fast and slow diffusion from diffusion-weighted MRI of pediatric Crohn’s disease. J Magn Reson Imaging 37(1):156–163. https://doi.org/10.1002/jmri.23781
Neubauer H, Pabst T, Dick A, Machann W, Evangelista L, Wirth C, Köstler H, Hahn D, Beer M (2013) Small-bowel MRI in children and young adults with Crohn disease: retrospective head-to-head comparison of contrast-enhanced and diffusion-weighted MRI. Pediatr Radiol 43(1):103–114. https://doi.org/10.1007/s00247-012-2492-1
Ream JM, Dillman JR, Adler J, Khalatbari S, McHugh JB, Strouse PJ, Dhanani M, Shpeen B, Al-Hawary MM (2013) MRI diffusion-weighted imaging (DWI) in pediatric small bowel Crohn disease: correlation with MRI findings of active bowel wall inflammation. Pediatr Radiol 43(9):1077–1085. https://doi.org/10.1007/s00247-013-2712-3
Rosenbaum DG, Rose ML, Solomon AB, Giambrone AE, Kovanlikaya A (2015) Longitudinal diffusion-weighted imaging changes in children with small bowel Crohn’s disease: preliminary experience. Abdom Imaging 40(5):1075–1080
Caruso A, Angriman I, Scarpa M, D’Incà R, Mescoli C, Rudatis M, Sturniolo GC, Schifano G, Lacognata C (2020) Diffusion-weighted magnetic resonance for assessing fibrosis in Crohn’s disease. Abdom Radiol (NY) 45(8):2327–2335. https://doi.org/10.1007/s00261-019-02167-0
Kim KJ, Lee Y, Park SH, Kang BK, Seo N, Yang SK, Ye BD, Park SH, Kim SY, Baek S, Ha HK (2015) Diffusion-weighted MR enterography for evaluating Crohn’s disease: How does it add diagnostically to conventional MR enterography? Inflamm Bowel Dis 21(1):101–109. https://doi.org/10.1097/MIB.0000000000000222
Masselli G, De Vincentiis C, Aloi M, Guida M, Cao R, Cartocci G, Miele V, Grassi R (2019) Detection of Crohn’s disease with diffusion images versus contrast-enhanced images in pediatric using MR enterography with histopathological correlation. Radiol Med 124(12):1306–1314. https://doi.org/10.1007/s11547-019-01067-z
Shenoy-Bhangle AS, Nimkin K, Aranson T, Gee MS (2016) Value of diffusion-weighted imaging when added to magnetic resonance enterographic evaluation of Crohn disease in children. Pediatr Radiol 46:34–42. https://doi.org/10.1007/s00247-015-3438-1
Caruso A, D’Incà R, Scarpa M, Manfrin P, Rudatis M, Pozza A, Angriman I, Buda A, Sturniolo GC, Lacognata C (2014) Diffusion-weighted magnetic resonance for assessing ileal Crohn’s disease activity. Inflamm Bowel Dis 20(9):1575–1583. https://doi.org/10.1097/MIB.0000000000000128
Buisson A, Hordonneau C, Goutte M, Scanzi J, Goutorbe F, Klotz T, Boyer L, Pereira B, Bommelaer G (2016) Diffusion-weighted magnetic resonance enterocolonography in predicting remission after anti-TNF induction therapy in Crohn’s disease. Dig Liver Dis 48(3):260–266. https://doi.org/10.1016/j.dld.2015.10.019
Bilgili MY (2012) Reproductibility of apparent diffusion coefficients measurements in diffusion-weighted MRI of the abdomen with different b values. Eur J Radiol 81:2066–2068. https://doi.org/10.1016/j.ejrad.2011.06.045
Braithwaite AC, Dale BM, Boll DT, Merkle EM (2009) Short- and midterm reproducibility of apparent diffusion coefficient measurements at 3.0-T diffusion-weighted imaging of the abdomen. Radiology 250:459–465. https://doi.org/10.1148/radiol.2502080849
Mainenti PP, Castiglione F, Rispo A, Laccetti E, Guarino S, Romeo V, Testa A, Pace L, Maurea S (2021) MR-enterography in Crohn’s disease: What MRE mural parameters are associated to one-year therapeutic management outcome? Br J Radiol 94(1118):20200844. https://doi.org/10.1259/bjr.20200844
Pendsé DA, Makanyanga JC, Plumb AA, Bhatnagar G, Atkinson D, Rodriguez-Justo M, Halligan S, Taylor SA (2017) Diffusion-weighted imaging for evaluating inflammatory activity in Crohn’s disease: comparison with histopathology, conventional MRI activity scores, and faecal calprotectin. Abdom Radiol (NY) 42(1):115–123. https://doi.org/10.1007/s00261-016-0863-z
Foti PV, Farina R, Coronella M, Palmucci S, Ognibene N, Milone P, Conti Bellocchi C, Samperi L, Inserra G, Laghi A, Ettorre GC (2015) Crohn’s disease of the small bowel: evaluation of ileal inflammation by diffusion-weighted MR imaging and correlation with the Harvey-Bradshaw index. Radiol Med 120(7):585–594. https://doi.org/10.1007/s11547-015-0502-8
Li XH, Mao R, Huang SY, Fang ZN, Lu BL, Lin JJ, Xiong SS, Chen MH, Li ZP, Sun CH, Feng ST (2019) Ability of DWI to characterize bowel fibrosis depends on the degree of bowel inflammation. Eur Radiol 29(5):2465–2473. https://doi.org/10.1007/s00330-018-5860-x
Kovanlikaya A, Beneck D, Rose M, Renjen P, Dunning A, Solomon A, Sockolow R, Brill PW (2019) Quantitative apparent diffusion coefficient (ADC) values as an imaging biomarker for fibrosis in pediatric Crohn’s disease: preliminary experience. Abdom Imaging 40(5):1068–1074. https://doi.org/10.1007/s00261-014-0247-1
Park SH (2016) DWI at MR enterography for evaluating bowel inflammation in Crohn disease. AJR Am J Roentgenol 207(1):40–48. https://doi.org/10.2214/AJR.15.15862
Funding
The authors declare that no funds, grants or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This work was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cicero, G., Alibrandi, A., Blandino, A. et al. DWI ratios: New indexes for Crohn’s disease activity at magnetic resonance enterography?. Radiol med 128, 16–26 (2023). https://doi.org/10.1007/s11547-022-01573-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01573-7