Abstract
Objectives
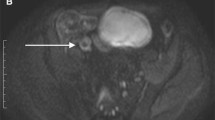
To validate the modified simplified magnetic resonance index of activity (sMARIA) score using DWI on non-contrast magnetic resonance enterography (MRE) to evaluate active inflammation in patients with Crohn’s disease (CD), compared to the original sMARIA scoring system, with and without contrast enhancement.
Methods
This retrospective study included 275 bowel segments from 55 CD patients who underwent ileocolonoscopy and MRE within a 2-week period. Two blinded radiologists evaluated original sMARIA on both conventional MRE (CE-sMARIA) and non-contrast MRE (T2-sMARIA). Modified sMARIA was then evaluated using non-contrast MRE, replacing ulcerations with DWI grades. Three scoring systems were compared for diagnostic accuracy of active inflammation, correlation with simple endoscopic score (SES)-CD, and interobserver reproducibility.
Results
The AUC of modified sMARIA for detecting active inflammation (0.863, 95% confidence interval [0.803–0.923]) was significantly higher than T2-sMARIA (0.827 [0.773–0.881], p = 0.017), and comparable to CE-sMARIA (0.908 [0.857–0.959], p = 0.122). CE-sMARIA, T2-sMARIA, and modified sMARIA all showed moderate correlation with SES-CD (r = 0.795, 0.722, and 0.777, respectively). Interobserver reproducibility of diffusion restriction (κ, 0.686 [0.602–0.770]) was significantly better than ulcers on conventional MRE (κ, 0.382 [0.212–0.552]; p = 0.001) and T2-weighted image (κ, 0.312 [0.034–0.590]; p = 0.012).
Conclusions
Modified sMARIA using DWI can improve the diagnostic performance of sMARIA on non-contrast MRE, showing comparable performance to sMARIA using contrast-enhanced MRE.
Key Points
• DWI can improve the diagnostic performance of non-contrast magnetic resonance enterography (MRE) for assessing active inflammation in patients with Crohn’s disease.
• Modified simplified magnetic resonance index of activity (sMARIA) using DWI grades in place of ulcers showed comparable diagnostic performance to sMARIA using conventional MRE with contrast-enhanced sequences.



Similar content being viewed by others
Abbreviations
- CD:
-
Crohn’s disease
- CE:
-
Contrast-enhanced
- CI:
-
Confidence interval
- ICC:
-
Intraclass correlation coefficient
- MARIA:
-
Magnetic resonance index of activity
- MRE:
-
Magnetic resonance enterography
- SD:
-
Standard deviation
- SES:
-
Simple endoscopic score
- sMARIA:
-
Simplified magnetic resonance index of activity
- T1WI:
-
T1-weighted imaging
- T2WI:
-
T2-weighted imaging
References
Cushing K, Higgins PDR (2021) Management of Crohn disease: a review. JAMA 325:69–80
Lichtenstein GR, Loftus EV, Isaacs KL, Regueiro MD, Gerson LB, Sands BE (2018) ACG clinical guideline: management of Crohn’s disease in adults. Am J Gastroenterol 113:481–517
Maaser C, Sturm A, Vavricka SR et al (2018) ECCO-ESGAR Guideline for diagnostic assessment in IBD Part 1: initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis 13:144-164K
Sturm A, Maaser C, Calabrese E et al (2018) ECCO-ESGAR Guideline for diagnostic assessment in IBD part 2: IBD scores and general principles and technical aspects. J Crohns Colitis 13:273–284
Rimola J, Ordás I, Rodriguez S et al (2010) Magnetic resonance imaging for evaluation of Crohn’s disease: validation of parameters of severity and quantitative index of activity. Inflamm Bowel Dis 17:1759–1768
Ordás I, Rimola J, Alfaro I et al (2019) Development and validation of a simplified magnetic resonance index of activity for Crohn’s disease. Gastroenterology 157:432-439.e431
Maximova N, Gregori M, Zennaro F, Sonzogni A, Simeone R, Zanon D (2016) Hepatic gadolinium deposition and reversibility after contrast agent-enhanced MR imaging of pediatric hematopoietic stem cell transplant recipients. Radiology 281:418–426
Kobayashi M, Levendovszky SR, Hippe DS et al (2021) Comparison of human tissue gadolinium retention and elimination between gadoteridol and gadobenate. Radiology 300:559–569
FDA Drug Safety Communication: FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warnings, U.S. Food and Drug Administration (2018) Available via https://www.fda.gov/Drugs/DrugSafety/ucm589213.htm. Accessed 20 Nov 2022
Bruining DH, Zimmermann EM, Loftus EV et al (2018) Consensus recommendations for evaluation, interpretation, and utilization of computed tomography and magnetic resonance enterography in patients with small bowel Crohn’s disease. Gastroenterology 154:1172–1194
Moy MP, Sauk J, Gee MS (2016) The role of MR enterography in assessing Crohn’s disease activity and treatment response. Gastroenterol Res Pract 2016:8168695
Capozzi N, Ordás I, Fernandez-Clotet A et al (2020) Validation of the simplified magnetic resonance index of activity [sMARIA] without gadolinium-enhanced sequences for Crohn’s disease. J Crohns Colitis 14:1074–1081
Fernàndez-Clotet A, Sapena V, Capozzi N et al (2022) Avoiding contrast-enhanced sequences does not compromise the precision of the simplified MaRIA for the assessment of non-penetrating Crohn’s disease activity. Eur Radiol 32:3334–3345
Kim JS, Jang HY, Park SH et al (2017) MR enterography assessment of bowel inflammation severity in Crohn disease using the MR index of activity score: modifying roles of DWI and effects of contrast phases. AJR Am J Roentgenol 208:1022–1029
Choi SH, Kim KW, Lee JY, Kim K-J, Park SH (2015) Diffusion-weighted magnetic resonance enterography for evaluating bowel inflammation in Crohn’s disease: a systematic review and meta-analysis. Inflamm Bowel Dis 22:669–679
Park SH (2016) DWI at MR enterography for evaluating bowel inflammation in Crohn disease. AJR Am J Roentgenol 207:40–48
Seo N, Park SH, Kim KJ et al (2016) MR Enterography for the evaluation of small-bowel inflammation in Crohn disease by using diffusion-weighted imaging without intravenous contrast material: a prospective noninferiority study. Radiology 278:762–772
Daperno M, D’Haens G, Van Assche G et al (2004) Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc 60:505–512
Obuchowski NA (1997) Nonparametric analysis of clustered ROC curve data. Biometrics 53:567–578
Zou KH, Tuncali K, Silverman SG (2003) Correlation and simple linear regression. Radiology 227:617–622
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Yang Z, Zhou M (2014) Kappa statistic for clustered matched-pair data. Stat Med 33:2612–2633
Vanbelle S (2017) Comparing dependent kappa coefficients obtained on multilevel data. Biom J 59:1016–1034
Rimola J, Rodriguez S, Garcia-Bosch O et al (2009) Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn’s disease. Gut 58:1113–1120
Buisson A, Joubert A, Montoriol P-F et al (2013) Diffusion-weighted magnetic resonance imaging for detecting and assessing ileal inflammation in Crohn’s disease. Aliment Pharmacol Ther 37:537–545
Tielbeek JA, Makanyanga JC, Bipat S et al (2013) Grading Crohn disease activity with MRI: interobserver variability of MRI features, MRI scoring of severity, and correlation with Crohn disease endoscopic index of severity. AJR Am J Roentgenol 201:1220–1228
Dohan A, Taylor S, Hoeffel C et al (2016) Diffusion-weighted MRI in Crohn’s disease: current status and recommendations. J Magn Reson Imaging 44:1381–1396
Buisson A, Hordonneau C, Goutte M, Boyer L, Pereira B, Bommelaer G (2015) Diffusion-weighted magnetic resonance imaging is effective to detect ileocolonic ulcerations in Crohn’s disease. Aliment Pharmacol Ther 42:452–460
Hordonneau C, Buisson A, Scanzi J et al (2014) Diffusion-weighted magnetic resonance imaging in ileocolonic Crohn’s disease: validation of quantitative index of activity. Am J Gastroenterol 109:89–98
Kim K-J, Lee Y, Park SH et al (2014) Diffusion-weighted MR enterography for evaluating Crohn’s disease: how does it add diagnostically to conventional MR enterography? Inflamm Bowel Dis 21:101–109
Barat M, Hoeffel C, Bouquot M et al (2019) Preoperative evaluation of small bowel complications in Crohn’s disease: comparison of diffusion-weighted and contrast-enhanced MR imaging. Eur Radiol 29:2034–2044
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) [grant number NRF-2018R1C1B6002747], a faculty research grant from Yonsei University College of Medicine [grant number 6-2021-0061], and Bracco diagnostics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Nieun Seo.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Hye Jung Shin (from the Biostatistics Collaboration Unit, Department of Biomedical Systems Informatics, Yonsei University College of Medicine) kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval from Severance Hospital was obtained.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bae, H., Seo, N., Kang, E.A. et al. Validation of the simplified magnetic resonance index of activity by using DWI without gadolinium enhancement to evaluate bowel inflammation in Crohn’s disease. Eur Radiol 33, 3266–3275 (2023). https://doi.org/10.1007/s00330-023-09501-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09501-7