Abstract
Cardiovascular diseases are still among the first causes of death worldwide with a huge impact on healthcare systems. Within these conditions, the correct diagnosis of coronary artery disease with the most appropriate imaging-based evaluations is of utmost importance. The sustainability of the healthcare systems, considering the high economic burden of modern cardiac imaging equipments, makes cost-effective analysis an important tool, currently used for weighing different costs and health outcomes, when policy makers have to allocate funds and to prioritize interventions, getting the most out of their financial resources. This review aims at evaluating cost-effective analysis in the more recent literature, focused on the role of Calcium Score, coronary computed tomography angiography and cardiac magnetic resonance.

Similar content being viewed by others
References
Mensah GA, Roth GA, Fuster V (2019) The global burden of cardiovascular diseases and risk factors: 2020 and Beyond. JACC 19:2529–2532. https://doi.org/10.1016/j.jacc.2019.10.009
European Cardiovascular Disease Statistics 2017 edition. https://www.ehnheart.org/cvd-statistics.html. Accessed 30 May 2020
Levin DC, Rao VM, Parker L et al (2005) Recent trends in utilization of cardiovascular imaging: how important are they for radiology? J Am Coll Radiol 2:736–739. https://doi.org/10.1016/j.jacr.2005.01.015
Picano E (2005) Economic and biological costs of cardiac imaging. Cardiovasc Ultrasound 3:13. https://doi.org/10.1186/1476-7120-3-13
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdatedJune2008.pdf. Accessed 30 May 2020
WHO Commission on Macroeconomics and Health (2001) Macroeconomics and health: investing in health for economic development. Report of the commission on macroeconomics and health. Geneva: World Health Organization, 200
Weintraub WS, Cohen DJ (2009) The Limits of cost-effectiveness analysis. Circ Cardiovasc Qual Outcomes 2:55–58. https://doi.org/10.1161/CIRCOUTCOMES.108.812321
Diamond GA, Kaul S (2009) Cost, effectiveness, and cost-effectiveness. Circ Cardiovasc Qual Outcomes 2:49–54. https://doi.org/10.1161/CIRCOUTCOMES.108.793406
Kianoush S, Mirbolouk M, Makam RC et al (2017) Coronary artery calcium scoring in current clinical practice: how to define its value? Curr Treat Options Cardiovasc Med 19:85. https://doi.org/10.1007/s11936-017-0582-y
Yeboah J, Young R, McClelland RL et al (2016) Utility of nontraditional risk markers in atherosclerotic cardiovascular disease risk assessment. JACC 67:139–147. https://doi.org/10.1016/j.jacc.2015.10.058
Blaha MJ, Yeboah J, Al Rifai M et al (2016) Providing evidence for subclinical CVD in risk assessment. Glob Heart 11:275–285. https://doi.org/10.1016/j.gheart.2016.08.003
Mody P, Joshi PH, Khera A et al (2016) Beyond coronary calcification, family history, and C-reactive protein: cholesterol efflux capacity and cardiovascular risk prediction. JACC 67:2480–2487. https://doi.org/10.1016/j.jacc.2016.03.538
Sarwar A, Shaw LJ, Shapiro MD et al (2009) Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2:675–688. https://doi.org/10.1016/j.jcmg.2008.12.031
Polonsky TS, McClelland RL, Jorgensen NW et al (2010) Coronary artery calcium score and risk classification for coronary heart disease prediction. JAMA 303:1610–1616. https://doi.org/10.1001/jama.2010.461
Nasir K, Bittencourt MS, Blaha MJ et al (2015) Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association Cholesterol Management guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). JACC 66:1657–1668. https://doi.org/10.1016/j.jacc.2015.07.066
Mahabadi AA, Möhlenkamp S, Lehmann N et al (2017) CAC score improves coronary and CV risk assessment above statin indication by ESC and AHA/ACC primary prevention guidelines. JACC Cardiovasc Imaging 10:143–153. https://doi.org/10.1016/j.jcmg.2016.03.022
Pursnani A, Massaro JM, D’Agostino RB Sr et al (2015) Guideline-based statin eligibility, coronary artery calcification, and cardiovascular events. JAMA 314:134–141. https://doi.org/10.1001/jama.2015.7515
van Kempen BJ, Spronk S, Koller MT et al (2011) Comparative effectiveness and cost-effectiveness of computed tomography screening for coronary artery calcium in asymptomatic individuals. JACC 58:1690–1701. https://doi.org/10.1016/j.jacc.2011.05.056
Pletcher MJ, Pignone M, Earnshaw S et al (2014) Using the coronary artery calcium score to guide statin therapy: a cost-effectiveness analysis. Circ Cardiovasc Qual Outcomes 7:276–284. https://doi.org/10.1161/CIRCOUTCOMES.113.000799
Roberts ET, Horne A, Martin SS et al (2015) Cost-effectiveness of coronary artery calcium testing for coronary heart and cardiovascular disease risk prediction to guide statin allocation: the Multi-Ethnic Study of Atherosclerosis (MESA). PLoS ONE 10:e0116377. https://doi.org/10.1371/journal.pone.0116377
Galper BZ, Wang YC, Einstein AJ (2015) Strategies for primary prevention of coronary heart disease based on risk stratification by the ACC/AHA lipid guidelines, ATP III guidelines, coronary calcium scoring, and C-reactive protein, and a global treat-all strategy: a comparative–effectiveness modeling study. PLoS ONE 10:e0138092. https://doi.org/10.1371/journal.pone.0138092
van Kempen BJ, Ferket BS, Steyerberg EW et al (2016) Comparing the cost-effectiveness of four novel risk markers for screening asymptomatic individuals to prevent cardiovascular disease (CVD) in the US population. Int J Cardiol 203:422–431. https://doi.org/10.1016/j.ijcard.2015.10.171
Hong JC, Blankstein R, Shaw LJ et al (2017) Implications of coronary artery calcium testing for treatment decisions among statin candidates according to the ACC/AHA cholesterol management guidelines: a cost-effectiveness analysis. JACC Cardiovasc Imaging 10:938–952. https://doi.org/10.1016/j.jcmg.2017.04.014
Chan PS, Patel MR, Klein LW, Krone RJ et al (2011) Appropriateness of percutaneous coronary intervention. JAMA 306:53–61. https://doi.org/10.1001/jama.2011.916
Go AS, Mozaffarian D, Roger VL et al (2013) Heart disease and stroke statistics-2013 update: a report from the American Heart Association. Circulation 127:e6–e245. https://doi.org/10.1161/CIR.0b013e31828124ad
Bradley SM, Spertus JA, Kennedy KF et al (2014) Patient selection for diagnostic coronary angiography and hospital-level percutaneous coronary intervention appropriateness: insights from the National Cardiovascular Data Registry. JAMA Intern Med 174:1630–1639. https://doi.org/10.1001/jamainternmed.2014.3904
Bradley SM, Maddox TM, Stanislawski MA et al (2014) Normal coronary rates for elective angiography in the Veterans Affairs Healthcare System: insights from the VA CART program (veterans affairs clinical assessment reporting and tracking). JACC 63:417–426. https://doi.org/10.1016/j.jacc.2013.09.055
Patel MR, Peterson ED, Dai D et al (2010) Low diagnostic yield of elective coronary angiography. NEJM 362:886–895. https://doi.org/10.1056/NEJMoa0907272
Janne d’Othee B, Siebert U, Cury R et al (2008) A systematic review on diagnostic accuracy of CT-based detection of significant coronary artery disease. Eur J Radiol 65:449–461. https://doi.org/10.1016/j.ejrad.2007.05.003
Budoff MJ, Dowe D, Jollis JG et al (2008) Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicentre ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. JACC 52:1724–1732. https://doi.org/10.1016/j.jacc.2008.07.031
Miller JM, Rochitte CE, Dewey M et al (2008) Diagnostic performance of coronary angiography by 64-row CT. NEJM 359:2324–2336. https://doi.org/10.1056/NEJMoa0806576
Meijboom WB, Meijs MF, Schuijf JD et al (2008) Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. JACC 52:2135–2144. https://doi.org/10.1016/j.jacc.2008.08.058
Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. Clinical guideline [CG95]. https://www.nice.org.uk/guidance/cg95. Accessed 30 May 2020
Knuuti J, Wijns W, Saraste A et al (2020) ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41:407–477. https://doi.org/10.1093/eurheartj/ehz425
Budoff MJ, Karwasky R, Ahmadi N et al (2009) Cost-effectiveness of multidetector computed tomography compared with myocardial perfusion imaging as gatekeeper to invasive coronary angiography in asymptomatic firefighters with positive treadmill tests. J Cardiovasc Comput Tomogr 3:323–330. https://doi.org/10.1016/j.jcct.2009.08.004
Halpern EJ, Savage MP, Fischman DL et al (2010) Cost-effectiveness of coronary CT angiography in evaluation of patients without symptoms who have positive stress test results. AJR 194:1257–1262. https://doi.org/10.2214/AJR.09.3209
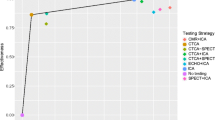
Lorenzoni V, Bellelli S, Caselli C et al (2019) Cost-effectiveness analysis of stand-alone or combined non-invasive imaging tests for the diagnosis of stable coronary artery disease: results from the EVINCI study. Eur J Health Econ 20:1437–1449. https://doi.org/10.1007/s10198-019-01096-5
Meijboom WB, Van Mieghe CA, van Pelt N et al (2008) Comprehensive assessment of coronary artery stenoses: computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. JACC 52:636–643. https://doi.org/10.1016/j.jacc.2008.05.024
Koo BK, Erglis A, Doh JH et al (2011) Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicentre DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. JACC 58:1989–1997. https://doi.org/10.1016/j.jacc.2011.06.066
Secchi F, Alì M, Faggiano E et al (2016) Fractional flow reserve based on computed tomography: an overview. Eur Heart J Suppl 18:E49–E56. https://doi.org/10.1093/eurheartj/suw014
Hlatky MA, Saxena A, Koo BK et al (2013) Projected costs and consequences of computed tomography-determined fractional flow reserve. Clin Cardiol 36:743–748. https://doi.org/10.1002/clc.22205
Lee SP, Jang EJ, Kim YJ et al (2015) Cost-effectiveness of coronary CT angiography in patients with chest pain: comparison with myocardial single photon emission tomography. J Cardiovasc Comput Tomogr 9:428–437. https://doi.org/10.1016/j.jcct.2015.02.008
Shreibati JB, Baker LC, Hlatky MA (2011) Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA 306:2128–2136. https://doi.org/10.1001/jama.2011.1652
Hulten E, Goehler A, Bittencourt MS et al (2013) Cost and resource utilization associated with use of computed tomography to evaluate chest pain in the emergency department: the Rule Out Myocardial Infarction Using Computer Assisted Tomography (ROMICAT) Study. Circ Cardiovasc Qual Outcomes 6:514–524. https://doi.org/10.1161/CIRCOUTCOMES.113.000244
Lee SP, Seo JK, Hwang IC et al (2019) Coronary computed tomography angiography vs. myocardial single photon emission computed tomography in patients with intermediate risk chest pain: a randomized clinical trial for cost-effectiveness comparison based on real-world cost. Eur Heart J Cardiovasc Imaging 20:417–425. https://doi.org/10.1093/ehjci/jey099
Bertoldi EG, Stella SF, Rohde LEP et al (2017) Cost-effectiveness of anatomical and functional test strategies for stable chest pain: public health perspective from a middle-income country. BMJ Open 7:e012652. https://doi.org/10.1136/bmjopen-2016-012652
Agus AM, McKavanagh P, Lusk L et al (2016) The cost-effectiveness of cardiac computed tomography for patients with stable chest pain. Heart 102:356–362. https://doi.org/10.1136/heartjnl-2015-308247
Gutberlet M, Fröhlich M, Mehl S et al (2005) Myocardial viability assessment in patients with highly impaired left ventricular function: comparison of delayed enhancement, dobutamine stress MRI, end-diastolic wall thickness, and TI201-SPECT with functional recovery after revascularization. Eur Radiol 15:872–880. https://doi.org/10.1007/s00330-005-2653-9
Thom H, West NE, Hughes V et al (2014) Cost-effectiveness of initial stress cardiovascular MR, stress SPECT or stress echocardiography as a gate-keeper test, compared with upfront invasive coronary angiography in the investigation and management of patients with stable chest pain: mid-term outcomes from the CECaT randomised controlled trial. BMJ Open 7:e003419. https://doi.org/10.1136/bmjopen-2013-003419
Moschetti K, Muzzarelli S, Pinget C et al (2012) Cost evaluation of cardiovascular magnetic resonance versus coronary angiography for the diagnostic work-up of coronary artery disease: application of the European Cardiovascular Magnetic Resonance registry data to the German, United Kingdom, Swiss, and United States health care systems. J Cardiovasc Magn Reson 14:35. https://doi.org/10.1186/1532-429X-14-35
Moschetti K, Favre D, Pinget C et al (2014) Comparative cost-effectiveness analyses of cardiovascular magnetic resonance and coronary angiography combined with fractional flow reserve for the diagnosis of coronary artery disease. J Cardiovasc Magn Reson 16:13. https://doi.org/10.1186/1532-429X-16-13
Moschetti K, Petersen SE, Pilz G et al (2016) Cost-minimization analysis of three decision strategies for cardiac revascularization: results of the “suspected CAD” cohort of the European Cardiovascular Magnetic Resonance Registry. J Cardiovasc Magn Reson 18:3. https://doi.org/10.1186/s12968-015-0222-1
Walker S, Girardin F, McKenna C et al (2013) Cost-effectiveness of cardiovascular magnetic resonance in the diagnosis of coronary heart disease: an economic evaluation using data from the CE-MARC study. Heart 99:873–881. https://doi.org/10.1136/heartjnl-2013-303624
Pletscher M, Walker S, Moschetti K et al (2016) Cost-effectiveness of functional cardiac imaging in the diagnostic work-up of coronary heart disease. Eur Heart J Qual Care Clin Outcomes 1:201–207. https://doi.org/10.1093/ehjqcco/qcw008
Petrov G, Kelle S, Fleck E et al (2015) Incremental cost-effectiveness of dobutamine stress cardiac magnetic resonance imaging in patients at intermediate risk for coronary artery disease. Clin Res Cardiol 104:401–409. https://doi.org/10.1007/s00392-014-0793-0
Campbell F, Thokala P, Uttley LC et al (2014) Systematic review and modelling of the cost-effectiveness of cardiac magnetic resonance imaging compared with current existing testing pathways in ischaemic cardiomyopathy. Health Technol Assess 18:1–120. https://doi.org/10.3310/hta18590
Porter ME (2010) What is value in health care? NEJM 363:2477–2481. https://doi.org/10.1056/NEJMp1011024
Hegde VA, Biederman RW, Mikolich JR (2017) Cardiovascular magnetic resonance imaging-incremental value in a series of 361 patients demonstrating cost savings and clinical benefits: an outcome-based study. Clin Med Insights Cardiol 11:1–10. https://doi.org/10.1177/1179546817710026
Miller CD, Hwang W, Case D et al (2011) Stress CMR imaging observation unit in the emergency department reduces 1-year medical care costs in patients with acute chest pain: a randomized study for comparison with inpatient care. JACC Cardiovasc Imaging 4:862–870. https://doi.org/10.1016/j.jcmg.2011.04.016
Hulten E, Goehler A, Bittencourt MS et al (2013) Cost and resource utilization associated with use of computed tomography to evaluate chest pain in the emergency department: the Rule Out Myocardial Infarction using Computer Assisted Tomography (ROMICAT) study. Circ Cardiovasc Qual Outcomes 1:514–524. https://doi.org/10.1161/CIRCOUTCOMES.113.000244
Zeb I, Abbas N, Nasir K et al (2014) Coronary computed tomography as a cost-effective test strategy for coronary artery disease assessment - a systematic review. Atherosclerosis 234:426–435. https://doi.org/10.1016/j.atherosclerosis.2014.02.011
Ge Y, Pandya A, Steel K et al (2020) Cost-effectiveness analysis of stress cardiovascular magnetic resonance imaging for stable chest pain syndromes. JACC Cardiovasc Imaging 13:1505–1517. https://doi.org/10.1016/j.jcmg.2020.02.029
Blanke P, Weir-McCall JR, Achenbach S et al (2019) Computed tomography imaging in the context of transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR): an expert consensus document of the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 13:1–20. https://doi.org/10.1016/j.jcct.2018.11.008
Huygens SA, Takkenberg JJ, Rutten-van Molken MP (2018) Systematic review of model-based economic evaluations of heart valve implantations. Eur J Health Econ 19:241–255. https://doi.org/10.1007/s10198-017-0880-z
Manolis AS (2017) Transcatheter aortic valve implantation economics: a grisly reality. Ann Cardiothorac Surg 6:516–523. https://doi.org/10.21037/acs.2017.07.02
Mahon C, Mohiaddin RH (2019) The emerging applications of cardiovascular magnetic resonance imaging in transcatheter aortic valve implantation. Clin Radiol 23:S0009-9260(19)30656-7. https://doi.org/10.1016/j.crad.2019.11.011
Di Cesare E, Carbone I, Carriero A et al (2012) Clinical indications for cardiac computed tomography. From the working group of the cardiac radiology section of the Italian Society of Medical Radiology (SIRM). Radiol Med 117:901–938. https://doi.org/10.1007/s11547-012-0899-2
Di Cesare E, Cademartiri F, Carbone I et al (2013) Clinical indications for the use of cardiac MRI. By the SIRM Study Group on Cardiac Imaging. Radiol Med 118:752–798. https://doi.org/10.1007/s11547-012-0899-2
Malagò R, Pezzato A, Barbiani C et al (2013) Role of MDCT coronary angiography in the clinical setting: economic implications. Radiol Med 118:1294–1308. https://doi.org/10.1007/s11547-013-0933-z
Centonze M, Lorenzin G, Francesconi A et al (2016) Cardiac-CT and Cardiac-MR examinations cost analysis, based on data of four Italian Centers. Radiol Med 121:12–18. https://doi.org/10.1007/s11547-015-0566-5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Centonze, M., Steidler, S., Casagranda, G. et al. Cardiac-CT and cardiac-MR cost-effectiveness: a literature review. Radiol med 125, 1200–1207 (2020). https://doi.org/10.1007/s11547-020-01290-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01290-z