Abstract
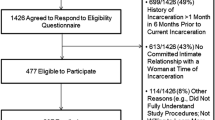
Non-Hispanic Black/African American men who have sex with men (AAMSM) have been disproportionately affected by criminal justice (CJ) involvement and HIV. One potential pathway between CJ involvement and high HIV prevalence and incidence among AAMSM is through risky sexual behavior. The goal of this study was to explore the association between recent CJ involvement, i.e., having been arrested and/or in prison/jail in the past 6 months, and transactional sex in a sample of AAMSM in Baltimore. We analyzed the baseline data of 396 AAMSM from a pilot behavioral HIV intervention conducted in Baltimore, MD, between October 2012 and November 2015. A multivariate logistic regression model was conducted to explore the association between recent CJ involvement and transactional sex. A total of 65 (16%) participants reported recent CJ involvement, and 116 (29%) reported transactional sex in the past 90 days. After adjusting for age, education, employment, sexual identity, HIV status, and drug use, recent CJ involvement was significantly associated with transactional sex (AOR 3.31; 95% CI 1.72; 5.70). Being 24–40 years (AOR 2.73; 95% CI 1.17, 6.33) or over 40 years older (AOR 3.80; 95% CI 1.61, 8.98) vs. younger and using drugs (AOR 4.47; 95% CI 2.43, 8.23) also remained independently associated with recent transactional sex. Findings of the current study contribute to the literature on the association between recent history of CJ involvement and transactional sex among AAMSM. More evidence-based HIV prevention interventions for people involved in the CJ system who are at high risk for contracting HIV, particularly racial and sexual minorities such as AAMSM, are urgently needed.
Similar content being viewed by others
References
Lincoln T, Simon-Levine D, Smith J, Donenberg GR, Springer SA, Zaller N, et al. Prevalence and predictors of mental/emotional distress among HIV+ jail detainees at enrollment in an observational study. J Correct Health Care. 2015;21:125–39.
Center for Disease Control and Prevention (CDC). Half of black gay men and a quarter of Latino gay men projected to be diagnosed within their lifetime. 2016. Available at: http://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html. Accessed 4/1, 2016.
Brewer RA, Magnus M, Kuo I, Wang L, Liu T, Mayer KH. The high prevalence of incarceration history among Black men who have sex with men in the United States: associations and implications. Am J Public Health. 2014;104:448–54.
Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL IV, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;379:341–8.
Jones KT, Johnson WD, Wheeler DP, Gray P, Foust E, Gaiter J, et al. Nonsupportive peer norms and incarceration as HIV risk correlates for young black men who have sex with men. AIDS Behav. 2008;12:41–50.
Phillips G, 2nd, Birkett M, Salamanca P, Ryan D, Garofalo R, Kuhns L, et al. Interplay of race and criminal justice involvement on sexual behaviors of young men who have sex with men. J Adolesc Health. 2018;63:197–204.
Hearn LE, Whitehead NE, Khan MR, Latimer WW. Time since release from incarceration and HIV risk behaviors among women: the potential protective role of committed partners during re-entry. AIDS Behav. 2015;19:1070–7.
Khan MR, Wohl DA, Weir SS, Adimora AA, Moseley C, Norcott K, et al. Incarceration and risky sexual partnerships in a southern US City. J Urban Health. 2008;85:100–13.
Higgins JA, Hoffman S, Dworkin SL. Rethinking gender, heterosexual men, and women’s vulnerability to HIV/AIDS. Am J Public Health. 2010;100:435–45.
Bauermeister JA, Eaton L, Meanley S, Pingel ES, Partnership UHIP. Transactional sex with regular and casual partners among young men who have sex with men in the Detroit metro area. Am J Mens Health. 2017;11:498–507.
Weber AE, Craib KJ, Chan K, Martindale S, Miller ML, Schechter MT, et al. Sex trade involvement and rates of human immunodeficiency virus positivity among young gay and bisexual men. Int J Epidemiol. 2001;30:1449–54. discussion 1455–6
Prestage G, Jin F, Bavinton B, Hurley M. Sex workers and their clients among Australian gay and bisexual men. AIDS Behav. 2014;18:1293–301.
Prestage G, Mao L, Jin F, Grulich A, Kaldor J, Kippax S. Sex work and risk behaviour among HIV-negative gay men. AIDS Care. 2007;19:931–4.
Philbin MM, Kinnard EN, Tanner AE, Ware S, Chambers BD, Ma A, et al. The association between incarceration and transactional aex among HIV-infected young men who have sex with men in the United States. J Urban Health. 2018;95:576–83.
Pager D, Western B, Sugie N. Sequencing disadvantage: barriers to employment facing young black and white men with criminal records. Ann Am Acad Pol Soc Sci. 2009;623:195–213.
Schneider J, Lancki N, Schumm P. At the intersection of criminal justice involvement and sexual orientation: dynamic networks and health among a population-based sample of young black men who have sex with men. Soc Networks. 2017;51:73–87.
German D. The BESURE study: 2018 update. Available at http://phpa.health.maryland.gov/OIDEOR/CHSE/SiteAssets/Pages/behavioral-surveillance/BESURE_Meeting_Handout_20180214.pdf. Accessed 5/1/2018.
Initiative PP. The right investment? Corrections spending in Baltimore City. Washington, DC: Justice Policy Institute; 2015.
Maryland Department of Public Safety and Correctional Services (DPSCS). Quarterly inmate characteristics report. 2014. Available at: http://www.dpscs.state.md.us/publicinfo/pdfs/stats/datareports/I_and_I-Statistics/Inmate_Characteristics/quarterly_Inmate_Characteristics/fy2014/2014-April_Inmate_Char.pdf. Accessed 14 Feb 2018.
U.S. Department of Justice. Investigation of the Baltimore City Police Department. 2016. Available at: https://www.justice.gov/crt/file/883296/download. Accessed 1 Feb 2018.
Javanbakht M, Ragsdale A, Shoptaw S, Gorbach PM. Transactional sex among men who have sex with men: differences by substance use and HIV status. J Urban Health. 2018. https://doi.org/10.1007/s11524-018-0309-8.
Beckwith CG, Zaller ND, Fu JJ, Montague BT, Rich JD. Opportunities to diagnose, treat, and prevent HIV in the criminal justice system. J Acquir Immune Defic Syndr. 2010;55(Suppl 1):S49–55.
Brinkley-Rubinstein L, Dauria E, Tolou-Shams M, Christopoulos K, Chan PA, Beckwith CG, et al. The path to implementation of HIV pre-exposure prophylaxis for people involved in criminal justice systems. Curr HIV/AIDS Rep. 2018;15:93–5.
Centers for Disease Control and Prevention (CDC). US public health service: preexposure prophylaxis for the prevention of HIV infection in the United States - 2017: updated clinical guideline. 2018. Available at: https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Accessed 9 Aug 2018.
Beck A, Berzofksy M, Caspar R, Krebs C. Sexual victimization in prisons and jails reported by inmates. U.S. Department of Justice: Washington, D. C; 2010.
World Health Organization (WHO). WHO expands recommendation on oral preexposure prophylaxis of HIV infection (PrEP). 2015. Available at: https://www.who.int/hiv/pub/prep/policy-brief-prep-2015/en/. Accessed 14 May 2018.
Brinkley-Rubinstein L, Peterson M, Arnold T, Nunn AS, Beckwith CG, Castonguay B, et al. Knowledge, interest, and anticipated barriers of pre-exposure prophylaxis uptake and adherence among gay, bisexual, and men who have sex with men who are incarcerated. PLoS One. 2018;13:e0205593.
Franks J, Hirsch-Moverman Y, Loquere AS Jr, Amico KR, Grant RM, Dye BJ, et al. Sex, PrEP, and stigma: experiences with HIV pre-exposure prophylaxis among new York City MSM participating in the HPTN 067/ADAPT Study. AIDS Behav. 2018;22:1139–49.
Peterson M, Nowotny K, Dauria E, Arnold T, Brinkley-Rubinstein L. Institutional distrust among gay, bisexual, and other men who have sex with men as a barrier to accessing pre-exposure prophylaxis (PrEP). AIDS Care. 2019;31:364–69.
Gagne CA, Finch WL, Myrick KJ, Davis LM. Peer workers in the behavioral and integrated health workforce: opportunities and future directions. Am J Prev Med. 2018;54:S258–66.
Wang EA, Hong CS, Shavit S, Sanders R, Kessell E, Kushel MB. Engaging individuals recently released from prison into primary care: a randomized trial. Am J Public Health. 2012;102:e22–9.
Acknowledgements
This study was funded by R01DA031030 and R01DA040488 from the National Institute of Drug Abuse, R00AA020782 from the National Institute on Alcohol Abuse and Alcoholism, R01MD013495 from National Institute on Minority Health and Health Disparities, R34MH116725 from the National Institute of Mental Health, Johns Hopkins Center for AIDS Research (P30AI094189).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, C., Zaller, N., Clyde, C. et al. Association between Recent Criminal Justice Involvement and Transactional Sex among African American Men Who Have Sex with Men in Baltimore. J Urban Health 97, 635–641 (2020). https://doi.org/10.1007/s11524-019-00350-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-019-00350-8