Abstract
Background
The combination of gemcitabine and cisplatin (gem/cis) with the anti-PD-L1-antibody durvalumab was recently approved as first line therapy for biliary tract cancer (BTC) based on the results of the TOPAZ-1 trial.
Objective
We aim to analyse the feasibility and efficacy of the triple combination therapy in patients with BTC in a real-world setting and in correspondence with the genetic alterations of the cancer.
Methods
In this single-centre retrospective analysis, all patients with BTC and treated with durvalumab plus gem/cis from April 2022 to September 2023 were included. Survival and treatment response were investigated, within the context of the inclusion and exclusion criteria of TOPAZ-1 and in correspondence with genetic alterations of the cancer.
Results
In total, 35 patients, of which 51% met the inclusion criteria of the TOPAZ-1 trial, were analysed. Patients treated within TOPAZ-1 criteria did not have a significantly different median overall survival and progression free survival than the rest of the patients (10.3 versus 9.7 months and 5.3 versus 5 months, respectively). The disease control rate of patients within the TOPAZ-1 criteria was 61.1%, in comparison to 58.8% in the rest of patients. A total of 51 grade 3 and 4 adverse events were observed without significant differences in the subgroups. No specific correlating patterns of genetic alterations with survival and response were observed.
Conclusions
The treatment of advanced patients with BTC with durvalumab and gem/cis, even beyond the inclusion criteria of the TOPAZ-1 trial, shows promising safety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We show that under real-world conditions the treatment of patients with advanced biliary tract cancer with the combination of gemcitabine and cisplatin with durvalumab seems safe in a broader patient population, and we did not observe differences in efficacy after stratification for fulfillment of the TOPAZ-1 inclusion criteria. |
We further could not identify any signal that specific genetic alterations of the tumor could help us predict an individual patients’ response to this therapy regimen. |
1 Introduction
Biliary tract cancer (BTC) represents a heterogenous group of malignancies originating from the biliary tree, including cholangiocarcinoma (CCA) of the intrahepatic and extrahepatic bile ducts as well as gallbladder carcinoma (GBC) [1]. Extrahepatic CCAs (eCCAs) are further classified into perihilar and distal CCAs according to their anatomical localisation [2]. The survival rates of BTCs are poor, and the incidence of intrahepatic CCAs (iCCAs) in particular, is rising globally, leading to an increasingly significant public health concern [3]. Most patients are diagnosed with advanced disease, and the only curative treatment, which requires surgical resection, can only be offered to up to a quarter of patients [4]. Thus, effective palliative systemic treatment is needed for the majority of patients.
The standard first-line treatment over the last decade has been the combination of gemcitabine and cisplatin (gem/cis) based on positive results of two randomised trials (5, 6). Recently, the phase III TOPAZ-1 trial with 685 patients showed that the addition of immune checkpoint therapy using the anti-programmed cell death ligand-1 (anti-PD-L1) antibody durvalumab in combination with gem/cis increased patient survival and has since become the new first-line treatment standard [7]. In this selected patient population, hazard ratios (HRs) for overall survival (OS) favoured durvalumab plus gem/cis over gem/cis with placebo (HR: 0.80) [7]. While the median OS in the intervention arm did increase by just 1.6 months in comparison with the placebo arm, a subgroup showed durable response with a 24-month survival rate of 23.6% versus 11.5%, respectively [8]. Parameters or biomarkers to specify these patients have yet to be identified, but response does not seem to be associated with PD-L1 expression (tumour area positivity higher versus lower than 1%). However, the genetic heterogeneity of BTCs and the critical influence of various oncogenic signaling pathways on the tumour microenvironment and therefore anti-tumour immunity might play a role in response to the triple therapy [9, 10].
Multiple next generation sequencing efforts have dissected the BTC genome over the last decade, revealing that BTCs are genetically very heterogeneous, with a variety of different oncogenes and tumour suppressor genes involved, and that these alterations are associated not only with the anatomical localisation but also with risk factors and pathologies [11,12,13,14]. Particularly for iCCAs, multiple targetable alterations such as IDH1 mutations, FGFR2 fusions or mutations and NTRK gene fusions led to the approval of new targeted therapeutics by regulatory agencies as monotherapy after failure of chemotherapy [15,16,17,18,19]. Additionally, while the percentage of microsatellite instability-high or mismatch repair deficient (MSI-H/dMMR) BTCs is low (1.3–1.5% in Western cohorts) [7, 20], these patients showed good response to the anti-programmed cell death protein-1 (PD-1) monoclonal antibody pembrolizumab with an objective response rate (ORR) of 40.9%, which is now approved as a second line therapy in this subgroup [21].
In this retrospective analysis we aim to investigate efficacy and safety of gem/cis and durvalumab in a less restricted real-world population and within the context of cancer genome alterations.
2 Materials and Methods
2.1 Study Population
For this analysis, requirements for inclusion were (1) histologically proven diagnosis of biliary tract malignancy, (2) irresectable (metastatic or locally advanced) disease and (3) start of palliative treatment with gem/cis and durvalumab between April 2022 and June 2023 at the National Center for Tumor Diseases (NCT) in Heidelberg, Germany. Gem/cis and durvalumab were administered intravenously on a 21-day cycle according to the TOPAZ-1 protocol: durvalumab (1500 mg) at day 1, gemcitabine (1000 mg/m2) and cisplatin (25 mg/m2) at days 1 and 8, respectively [7]. After eight cycles, treatment was continued with durvalumab 1500 mg monotherapy every 4 weeks until radiological progression, unacceptable toxicity or death.
The data were maintained via a prospective database, the Liver Cancer Center Heidelberg (LCCH) registry. The observation period for each patient started with initiation of gem/cis and durvalumab (after primary diagnosis of metastatic or unresectable disease, or after diagnosis of recurrence). The follow-up period for this analysis ended on 30 September 2023.
Written informed consent was obtained from all patients prospectively enrolled in the Liver Cancer Center Heidelberg (LCCH) registry, which was approved by the Heidelberg University ethics committee (ethical permit number S-693/2019), complied with the provisions of the Good Clinical Practice guidelines and the Declaration of Helsinki and local laws and fulfilled the Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data (ID number DSAN854-A-OS/5).
2.2 Assessments
The clinical data were reported via an electronic medical record by the attending oncologists and medical staff. Information included date of previous treatment (surgery, adjuvant chemotherapy and radiochemotherapy), start and stop date of chemotherapy, type and severity of toxicities, Eastern Cooperative Ongology Group performance status (ECOG PS) and date of death. Adverse events were registered according to the US National Cancer Institute’s common terminology criteria for adverse events (CTCAE). Tumour response was routinely evaluated with a structured oncology reporting in analogy to the response evaluation criteria in solid tumours (RECIST) 1.1 [22].
2.3 Statistical Analysis
Descriptive statistics were used to analyse baseline characteristics, survival times, treatment response, adverse events (AEs) and molecular tumour characterisation. OS was defined as time from the date of treatment initiation to the date of death. PFS was defined as time from the date of treatment initiation to the date of disease progression or death. Treatment response was assessed radiologically by computed tomography (CT) or magnetic resonance imaging (MRI) by local review. ORR was defined as the rate of complete responses (CR) and partial responses (PR). Disease control rate (DCR) was defined as the sum of CR, PR and the rate of stable disease (SD). Survival plots were presented as Kaplan–Meier curves and quantified by the Gehan–Breslow–Wilcoxon test, HR and 95% confidence interval (CI) based on a log-rank test. Statistical analyses were performed with GraphPad prism V10 (GraphPad Software, San Diego, CA, USA). A P < 0.05 was considered statistically significant.
2.4 Molecular Profiling
DNA and RNA extraction was performed on formalin-fixed paraffin-embedded tumour sections from 29 patients, who had been included in a personalised oncology program. All samples had a tumour cell content > 20%. DNA based genetic alterations were obtained using the TruSight Oncolocy 500 (TSO500) panel. RNA based alterations and gene fusions were detected using the TruSight Tumor 170 (TST 170) RNA assay. Analysis was performed by at least two pathological experts and has been previously described [23].
3 Results
3.1 Patient Demographics
The analysis included 35 patients with BTC: 21 (60%) with iCCA, 8 (23%) with eCCA and 6 (17%) patients with GBC, who received gem/cis plus durvalumab as palliative therapy. Patients had a median age of 62 years (range 27–80 years) at start of therapy, 20 of which were female (57%) and 15 of which were male (43%). A total of 25 patients (71%) presented with initially unresectable disease, of which 8 (23%) were locally advanced and 27 (77%) had metastatic disease. Ten patients (29%) presented with recurrent disease, and two patients (6%), both with iCCA, suffered from liver cirrhosis, of which one was caused by chronic hepatitis B infection. Nine (26%) patients had previously undergone resection, of which eight patients received further adjuvant therapy (chemotherapy or radiation). Two additional patients (6%) had undergone radiation therapy prior to the systemic triple therapy, and four (11%) patients had received prior palliative systemic therapy, of which one of these reveived radiation therapy and systemic therapy. A total of 22 (63%) patients were therapy-naïve; 31 patients (88%) presented with ECOG performance status of 0 and 1 and 4 patients (12%) with ECOG 2 and 3. Additional baseline characteristics are presented in Table 1.
A total of 18 patients (51%) fulfilled the inclusion criteria of the TOPAZ-1 trial (TOPAZ-1 IN), whereas 17 patients (49%) did not (TOPAZ-1 OUT). The most common reason for failing to meet the TOPAZ-1 trial inclusion criteria was the prior existence of autoimmune-associated disorders (n = 4 patients: ulcerative colitis, sarcoidosis, SAPHO-syndrome and autoimmune mediated urticaria), followed by ECOG performance status > 1 (n = 4), and five patients had received prior chemotherapy or radiotherapy (Table 2). Seven additional patients would have been excluded from the TOPAZ-1 trial because of insufficient organ function assessment (haematopoiesis and renal function).
3.2 Progression and Survival
Of all patients included, 34 patients (97%) had at least one radiological assessment after starting therapy to evaluate tumour response. One patient died before the first assessment. Median duration of follow-up after start of treatment was 6.2 months (range 1–14.7 months). A total of 16 patients (46%) died. Median OS in the cohort was 10.3 months (Fig. 1A). Median PFS was 5.1 months (Fig. 1C). The investigator-assessed ORR was 14.7%, and the disease control rate (DCR) was 61.7%.
Overall survival (OS) and progression free survival (PFS) with durvalumab plus gem/cis. Kaplan–Meier curve indicating OS A in the whole cohort (n = 35 patients) and B stratified by the inclusion criteria of TOPAZ-1 (TOPAZ-1 IN: n = 18 and TOPAZ-1 OUT: n = 17). PFS depicted by Kaplan–Meier curve C in the whole cohort and D stratified according to TOPAZ-1 inclusion criteria
Median OS in TOPAZ-1 IN patients was not significantly different to TOPAZ-1 OUT patients (10 versus 10.3 months (HR: 0.97, 95% CI 0.3–2.6; Fig. 1B). Similarly, the median PFS with 5.3 months in the TOPAZ-1 IN patient cohort was not significantly different to the 5 months in TOPAZ-1 OUT patients (HR: 1.06, 95% CI 0.49–2.29; Fig. 1D). DCR was similar in both subgroups (TOPAZ-1 IN 61.1% versus TOPAZ-1 OUT 58.8%, respectively), but the ORR in the TOPAZ-1 IN subgroup was higher, with 22.2% versus 5.8%.
3.3 Safety
During the observation period, a total of 51 grade 3–4 AEs were registered in 21 patients (Table 3). The most common AEs were bone marrow toxicity (n = 21, 40%), such as anaemia (n = 8, 23%), thrombocytopenia (n = 7, 20%) and leukopenia (n = 6, 17%). Infectious complications, in particular cholangitis, were observed in five patients (11%). Elevated cholestasis parameters occurred in five patients (11%), and elevated transaminases occurred in two patients (4%). Ascites or pleural effusion were observed in four patients (9%). In five cases (9.6%), AEs were considered to be immunotherapy related (irAEs), two cases of autoimmune colitis and one case of autoimmune hepatitis, autoimmune encephalitis and immune-mediated urticaria each. Three of these patients were treated with corticosteroids. In 14 cases (40%), the adverse event led to a dose reduction. No grade 5 AE has been reported. IrAEs were equally distributed in both subgroups with 2 patients each, and 10 patients in the TOPAZ1-IN and 11 patients in the TOPAZ1-OUT developed non-irAEs. No significant differences in AE occurence in terms of frequency and severity could be observed between the subgroups.
3.4 Molecular Profiling
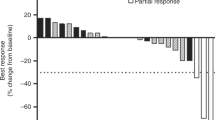
For 29 patients, molecular profiling of the tumour was obtained as a diagnostic work-up in a personalised oncology program (Fig. 2 and Supplementary Table 1). Of those, 18 patients presented with iCCA, 4 patients with eCCA and 2 patients with GBC, and among them, 5 patients had PR, 10 patients had SD and 14 patients were non-responders. The most frequent genetic alteration was loss of tumour suppressor protein 53 (TP53) (28%, n = 8) followed by deletion mutations in BRCA1-associated protein 1 (BAP1; 24%, n = 7). Activating mutations of KRAS were observed in 21% (n = 6). Mutations leading to deletion of ARID1A were observed in 17% (n = 5). Oncogenic IDH1 mutations, deletion mutations of and SMAD4 and MUTYH and fusions of the FGFR2 gene occurred each in 10% (n = 3) of patients. Within this cohort, response to treatment was not associated with specific genetic alterations (Fig. 2).
Distribution of genetic alterations in BTCs in accordance with response to durvalumab plus gem/cis. BTCs are clustered based on the best response to treatment: PR, SD and PD. Tumour localisation is indicated by the respective colours. Genetic alterations are characterized by either deletion, activating or activating translocation (i.e. fusion)
4 Discussion
The advent of the new first-line treatment combining gem/cis with the PD-L1 inhibitor durvalumab based on the positive results of the TOPAZ-1 phase III trial significantly changed the treatment landscape of BTCs in the palliative setting. More recently, the KEYNOTE-966 study using the PD-1 inhibitor pembrolizumab in combination with gem/cis showed similar efficacy and safety data [24], confirming a beneficial effect of immune checkpoint inhibition (ICI) to standard chemotherapy. Both trials achieved median OS data of over 12 months [7, 24], which has not been reached by any other treatment regimen and has a significant impact on this cancer entity with such a poor prognosis. First data from one multicentre retrospective analysis of an early access program in Italy were also able to consolidate the results of the TOPAZ-1 trial in a real-world setting [25].
In our cohort, the median OS and PFS with 10.3 months and 5.1 months were lower than the 12.8 months and 7.2 months reached in the registration trial. While most of the baseline characteristics in our cohort were comparable with the TOPAZ-1 trial data, our cohort was smaller but also presented with less viral hepatitis as underlying liver disease etiology, which also correlated with favourable prognosis in the analysis of Rimini et al. [25]. An additional difference was that our cohort comprised primarily of Caucasians, while in the TOPAZ-1 trial, the Asian subgroup seemed to have responded particularly well. Additionally, the shorter median observation time with 6.2 months in comparison with the registration trial and, therefore, a potential underreporting of OS. Interestingly, the 46% of patients who would have been excluded according to protocol of the TOPAZ-1 trial did not show inferior survival or radiologic response results than TOPAZ-1 IN patients and cannot explain the different outcomes observed.
In summary, our data suggests that a broader set of patients could profit from the triple therapy, which warrants additional prospective analyses in larger cohorts of that extended patient subgroup.
Assessing the safety profile of a treatment is essential for its broad clinical applicability. In general, in most registration trials the patient population is selected and only partially reflects the real-world population. It is therefore important to assess safety of a treatment in a broader collective. In our cohort, even though patients beyond the inclusion criteria of TOPAZ-1 were included, the rate of grade ≥ 3 AEs observed was not higher than in the TOPAZ-1 trial (60% versus 75.7%, respectively). The rate of dose reduction/discontinuation was also similar, as well as the quality of AEs. This was also the case when we compared the two subgroups, TOPAZ-1 IN and TOPAZ-1 OUT. Overall, the inclusion of patients beyond the TOPAZ-1 criteria in this cohort did not lead to an increase in AEs or alteration of the treatment. Our data support that selected patients beyond the population of TOPAZ-1 can undergo triple therapy with limited risk in well-monitored clinical settings.
Molecular profiling of tumours has become increasingly important in understanding cancer biology and guiding treatment decisions. Therefore, we aim to perform panel sequencing analysis in our clinical routine early in the palliative setting, whenever enough tumour material is available. At data cut-off, 29 patients of the cohort had undergone molecular tumour profiling. Despite the relatively small size of the cohort, the distribution of the genetic alterations is consistent with the large, published data sets [11,12,13, 15]. Biomarkers to identify patients who respond well to immunotherapy are sorely lacking, but genetic alterations may play a role in response. To explore this, we included a first analysis to associate genetic alterations with response. While the small cohort size limits interpretation, genetic alterations were quite evenly distributed among both responders and non-responders. Even the patient with MSI-high tumour, where one would except a high chance of response to ICIs, had only moderate response of 7 months SD. However, this is in accordance with data from the Keynote-158 trial with pembrolizumab in second line MSI-high BTCs, where the ORR was 41% [21]. While larger cohorts with molecular data will be required to comprehensively explore these relationships and identify potential biomarkers for response prediction, it is evident that even microsatellite instability, despite being a generally immunoreactive condition, has limited predictive value. This clearly illustrates the multifactorial aspects involved in response to immunotherapy and emphasises that individual response prediction will require consideration of multiple parameters.
In conclusion, our real-world data provide first evidence that the treatment regimen of durvalumab plus gem/cis in patients with BTC is safe even beyond the TOPAZ-1 inclusion criteria, suggesting that this treatment strategy may have broader applicability in a diverse patient population and supporting further prospective analyses in larger cohorts.
References
Valle JW, Kelley RK, Nervi B, Oh DY, Zhu AX. Biliary tract cancer. Lancet. 2021;397(10272):428–44.
Kirstein MM, Vogel A. Epidemiology and risk factors of cholangiocarcinoma. Visc Med. 2016;32(6):395–400.
Lee W-S, Lee K-W, Heo J-S, Kim S-J, Choi S-H, Kim Y-I, et al. Comparison of combined hepatocellular and cholangiocarcinoma with hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Surg Today. 2006;36(10):892–7.
Banales JM, Marin JJG, Lamarca A, Rodrigues PM, Khan SA, Roberts LR, et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol. 2020;17(9):557–88.
Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, et al. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 2010;362(14):1273–81.
Okusaka T, Nakachi K, Fukutomi A, Mizuno N, Ohkawa S, Funakoshi A, et al. Gemcitabine alone or in combination with cisplatin in patients with biliary tract cancer: a comparative multicentre study in Japan. Br J Cancer. 2010;103(4):469–74.
Oh DY, Lee KH, Lee DW, Yoon J, Kim TY, Bang JH, et al. Gemcitabine and cisplatin plus durvalumab with or without tremelimumab in chemotherapy-naive patients with advanced biliary tract cancer: an open-label, single-centre, phase 2 study. Lancet Gastroenterol Hepatol. 2022;7(6):522–32.
Oh DY, He AR, Qin S, Chen LT, Okusaka T, Vogel A, et al. 78P Updated overall survival (OS) from the phase III TOPAZ-1 study of durvalumab (D) or placebo (PBO) plus gemcitabine and cisplatin (+ GC) in patients (pts) with advanced biliary tract cancer (BTC). Ann Oncol. 2022;33:S1462–3.
Greten TF, Schwabe R, Bardeesy N, Ma L, Goyal L, Kelley RK, et al. Immunology and immunotherapy of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol. 2023;20(6):349–65.
Manthopoulou E, Ramai D, Dhar J, Samanta J, Ioannou A, Lusina E, et al. Cholangiocarcinoma in the era of immunotherapy. Vaccines (Basel). 2023;11(6):1062.
Jusakul A, Cutcutache I, Yong CH, Lim JQ, Huang MN, Padmanabhan N, et al. Whole-genome and epigenomic landscapes of etiologically distinct subtypes of cholangiocarcinoma. Cancer Discov. 2017;7(10):1116–35.
Chan-On W, Nairismagi ML, Ong CK, Lim WK, Dima S, Pairojkul C, et al. Exome sequencing identifies distinct mutational patterns in liver fluke-related and non-infection-related bile duct cancers. Nat Genet. 2013;45(12):1474–8.
Goeppert B, Folseraas T, Roessler S, Kloor M, Volckmar AL, Endris V, et al. Genomic characterization of cholangiocarcinoma in primary sclerosing cholangitis reveals therapeutic opportunities. Hepatology. 2020;72(4):1253–66.
Wu YM, Su F, Kalyana-Sundaram S, Khazanov N, Ateeq B, Cao X, et al. Identification of targetable FGFR gene fusions in diverse cancers. Cancer Discov. 2013;3(6):636–47.
Nakamura H, Arai Y, Totoki Y, Shirota T, Elzawahry A, Kato M, et al. Genomic spectra of biliary tract cancer. Nat Genet. 2015;47(9):1003–10.
Abou-Alfa GK, Sahai V, Hollebecque A, Vaccaro G, Melisi D, Al-Rajabi R, et al. Pemigatinib for previously treated, locally advanced or metastatic cholangiocarcinoma: a multicentre, open-label, phase 2 study. Lancet Oncol. 2020;21(5):671–84.
Doebele RC, Drilon A, Paz-Ares L, Siena S, Shaw AT, Farago AF, et al. Entrectinib in patients with advanced or metastatic NTRK fusion-positive solid tumours: integrated analysis of three phase 1–2 trials. Lancet Oncol. 2020;21(2):271–82.
Hong DS, Bauer TM, Lee JJ, Dowlati A, Brose MS, Farago AF, et al. Larotrectinib in adult patients with solid tumours: a multi-centre, open-label, phase I dose-escalation study. Ann Oncol. 2019;30(2):325–31.
Goyal L, Meric-Bernstam F, Hollebecque A, Valle JW, Morizane C, Karasic TB, et al. Futibatinib for FGFR2-rearranged intrahepatic cholangiocarcinoma. N Engl J Med. 2023;388(3):228–39.
Goeppert B, Roessler S, Renner M, Singer S, Mehrabi A, Vogel MN, et al. Mismatch repair deficiency is a rare but putative therapeutically relevant finding in non-liver fluke associated cholangiocarcinoma. Br J Cancer. 2019;120(1):109–14.
Marabelle A, Le DT, Ascierto PA, Di Giacomo AM, De Jesus-Acosta A, Delord JP, et al. Efficacy of pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair-deficient cancer: results from the phase II KEYNOTE-158 study. J Clin Oncol. 2020;38(1):1–10.
Weber TF, Spurny M, Hasse FC, Sedlaczek O, Haag GM, Springfeld C, et al. Improving radiologic communication in oncology: a single-centre experience with structured reporting for cancer patients. Insights Imaging. 2020;11(1):106.
Tomczak A, Springfeld C, Dill MT, Chang DH, Kazdal D, Wagner U, et al. Precision oncology for intrahepatic cholangiocarcinoma in clinical practice. Br J Cancer. 2022;127(9):1701–8.
Kelley RK, Ueno M, Yoo C, Finn RS, Furuse J, Ren Z, et al. Pembrolizumab in combination with gemcitabine and cisplatin compared with gemcitabine and cisplatin alone for patients with advanced biliary tract cancer (KEYNOTE-966): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2023;401(10391):1853–65.
Rimini M, Fornaro L, Lonardi S, Niger M, Lavacchi D, Pressiani T, et al. Durvalumab plus gemcitabine and cisplatin in advanced biliary tract cancer: an early exploratory analysis of real-world data. Liver Int. 2023;43(8):1803–12.
Acknowledgements
The authors are grateful to Ursula Wagner for assistance with recruiting and documentation and would like to thank all patients for their participation in the registry.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open Access funding enabled and organized by Projekt DEAL. A.T. is supported by the German Ministry of Research and Education (01ZZ1802, 01ZZ3222E). M.T.D. is supported by a Max Eder funding grant (70113858) of the German Cancer Aid.
Conflict of interest
P. Michl receives speakers honorary by AstraZeneca. Alexander Olkus, Aurelie Tomczak, Anne Katrin Berger, Conrad Rauber, Philip Puchas, Cyrill Wehling, Thomas Longerich, Arianeb Mehrabi, De-Hua Chang, Jakob Liermann, Sophia Schäfer, Jan Pfeiffenberger, Dirk Jäger, Christoph Springfeld and Michael T. Dill declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval and consent to participate:
The LCCH registry study was approved by the local ethics committee of the Heidelberg University Hospital (S-693/2019). Informed consent was obtained from all prospectively enrolled patients. The study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Data availability
Relevant genomic data are provided as Supplementary Material. Additional data are available upon reasonable request.
Code availability
Not applicable.
Author contributions
A.O. and M.T.D. conceived and designed the study. A.O., A.T., T.L. and M.T.D. analysed the data. A.B., T.L., C.S., P.P., C.R., C.W., M.T.D., A.M., D.H.C., J.L., J.P., D.J. and P.M. participated in interdisciplinary tumour board decisions, supervised clinical annotations and provided critical data interpretation. S.S. supervised the clinical cancer registry and provided intellectual input. A.O. and M.T.D. wrote the manuscript. A.B., C.S. and A.T. provided substantial editorial work to the manuscript. All authors have read and provided comments on the manuscript. All authors approved the manuscript and gave their consent for submission and publication.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Olkus, A., Tomczak, A., Berger, A.K. et al. Durvalumab Plus Gemcitabine and Cisplatin in Patients with Advanced Biliary Tract Cancer: An Exploratory Analysis of Real-World Data. Targ Oncol 19, 213–221 (2024). https://doi.org/10.1007/s11523-024-01044-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-024-01044-1