Abstract
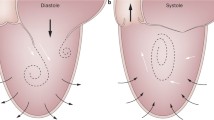
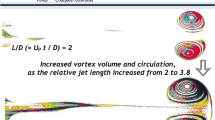
The formation of vortex rings in the left ventricular (LV) blood flow is a mechanism for optimized blood transport from the mitral valve inlet to aortic valve outlet, and the vorticity is an important measure of a well-functioning LV. However, due to lack of quantitative methods, the process of defining the boundary of a vortex in the LV and identifying the dominant vortex components has not been studied previously. The Lagrangian-averaged vorticity deviation (LAVD) can enable us to compute the trajectory integral of the normed difference of the vorticity from its spatial mean. Therefore, in this work, we have employed LAVD to identify the Lagrangian vortices and Eulerian vortices for measuring the vortex volume and vorticity in the LV blood flow. We found that during the LV ejection period, the positive (counterclockwise) and negative (clockwise) vorticity of patients are consistently stronger than those of the healthy groups, and the counterclockwise vortex volume of healthy groups (0.84+0.26 ml) is greater than that of patients (0.55+0.28 ml) during the pre-ejection period. Then, during the middle ejection phase, the counterclockwise vortex ring volume of patients (1.89+0.36 ml) exceeds that of healthy groups (1.38+0.43 ml). Finally, during the end-ejection period, the counterclockwise vortex ring volume of healthy subjects (0.61+0.17 ml) is the same as that of patients (0.60+0.19 ml). The results presented in this paper can provide new insights into the blood flow patterns within the LV. It can accurately indicate the role of vortices and vorticity values in intra-LV flow, and portray how cardiomyopathy (and its distorted contractile mechanism) can affect intra-LV flow patterns and mitigate adequate LV outflow.








Similar content being viewed by others
References
Kheradvar A, Houle H, Pedrizzetti G, Tonti G, Belcik T, Ashraf M, Lindner JR, Gharib M, Sahn D (2010) Echocardiographic particle image velocimetry: a novel technique for quantification of left ventricular blood vorticity pattern. J Am Soc Echocardiogr 23(1):86–94
Kheradvar A, Milano M, Gharib M (2007) Correlation between vortex ring formation and mitral annulus dynamics during ventricular rapid filling. ASAIO J 53(1):8–16
Wong KKL, Kelso RM, Worthley SG, Sanders P, Mazumdar J, Abbott D (2009) Cardiac flow analysis applied to phase contrast magnetic resonance imaging of the heart. Ann Biomed Eng 37(8):1495–1515
Gharib M, Rambod E, Kheradvar A, Sahn DJ, Dabiri JO (2006) Optimal vortex formation as an index of cardiac health. Proc Natl Acad Sci 103(16):6305–6308
Ghista DN, Li L, Chua LP et al (2009) Mechanism of left ventricular pressure increase during isovolumic contraction, and determination of its equivalent myocardial fibers orientation. Journal Mechanics Medicine and Biology 9(2):177–198
Chapra SC (2013) Numerical methods for engineers[J]. Mcgraw-Hill Publ Comp 22(6):59–68
Garcia J, Larose E, Pibarot P, Kadem L (2013) On the evaluation of vorticity using cardiovascular magnetic resonance velocity measurements. J Biomech Eng 135(12):124501–124506
Hirtler D, Garcia J, Barker AJ, Geiger J (2016) Assessment of intracardiac flow and vorticity in the right heart of patients after repair of tetralogy of Fallot by flow-sensitive 4D MRI. Eur Radiol 26(10):3598–3607
Spiczak JV, Crelier G, Giese D, Kozerke S, Maintz D, Bunck AC (2015) Quantitative analysis of vortical blood flow in the thoracic aorta using 4D phase contrast MRI. PLoS One 10(9):e0139025
Nordmeyer S, Riesenkampff E, Messroghli D, Kropf S, Nordmeyer J, Berger F, Kuehne T (2013) Four-dimensional velocity-encoded magnetic resonance imaging improves blood flow quantification in patients with complex accelerated flow. J Magn Reson Imaging 37(1):208–216
Frydrychowicz A, Berger A, Stalder AF, Markl M (2009) Preliminary results by flow-sensitive magnetic resonance imaging after Tiron David I procedure with an anatomically shaped ascending aortic graft. Interact Cardiovasc Thorac Surg 9(2):155–158
Lorenz R, Bock J, Barker AJ, Knobelsdorff-Brenkenhoff FV, Wallis W, Korvink JG et al (2014) 4D flow magnetic resonance imaging in bicuspid aortic valve disease demonstrates altered distribution of aortic blood flow helicity. Magn Reson Med 71(4):1542–1553
Zhong L, Tan RS, Ghista DN, EYK N, Chua LP, Kassab GS (2007) Validation of a novel noninvasive cardiac index of left ventricular contractility in patients. American Journal of Physiology-Heart Circulatory Physiology 292:H2764–H2772
Etebari A, Vlachos PP (2006) Improvements on the accuracy of derivative estimation from DPIV velocity measurements. Exp Fluids 40(3):500–502
Sotelo J, Urbina J, Valverde I, Mura J, Tejos C, Irarrazaval P, Andia ME, Hurtado DE, Uribe S (2018) Three-dimensional quantification of vorticity and helicity from 3D cine PC-MRI using finite-element interpolations. Magn Reson Med 79(1):541–553
Zienkiewicz OC, Taylor RL, Zhu JZ (2005) The finite element method: its basis and fundamentals, 6th Edition. Butterworth-Heinemann
Töger J, Kanski M, Carlsson M, Kovacs SJ, Söderlind G, Arheden H et al (2012) Vortex ring formation in the left ventricle of the heart: analysis by 4D flow MRI and Lagrangian coherent structures. Ann Biomed Eng 40(12):2652–2662
Elbaz MSM, Calkoen EE, Westenberg JJM, Lelieveldt BPF, Wroest AA, Geest R (2014) Vortex flow during early and late left ventricular filling in normal subjects: quantitative characterization using retrospectively-gated 4D flow cardiovascular magnetic resonance and three-dimensional vortex core analysis. J Cardiovasc Magn Reson 16(1):78–90
Hong GR, Pedrizzetti G, Tonti G, Li P, Wei Z, Kim JK, Baweja A, Liu S, Chung N, Houle H, Narula J, Vannan MA (2008) Characterization and quantification of vortex flow in the human left ventricle by contrast echocardiography using vector particle image velocimetry. J Am Coll Cardiol Img 1(6):705–717
Kräuter C, Reiter U, Reiter C, Nizhnikava V, Masana M, Schmidt A, Fuchsjäger M, Stollberger R, Reiter G (2020) Automated mitral valve vortex ring extraction from 4D-flow MRI. Magn Reson Med 84:3396–3408
Haller G, Hadjighasem A, Farazmand M, Huhn F (2015) Defining coherent vortices objectively from the vorticity. J Fluid Mech 795(7):136–173
Hall JE (2006) Textbook of medical physiology. Quarterly Journal of Experimental Physiology & Cognate Medical Sciences 51(4):380–381
Schmitz L, Koch H, Bein G, Brockmeier K (1998) Left ventricular diastolic function in infants, children, and adolescents. Reference values and analysis of morphologic and physiologic determinants of echocardiographic Doppler flow signals during growth and maturation[J]. J Am Coll Cardiol 32(5):1441–1448
Wong KKL, Tu J, Kelso RM, Worthley SG, Sanders P, Mazumdar J, Abbott D (2010) Cardiac flow component analysis. Med Eng Phys 32(2):174–188
Raffel M, Willert CE, Wereley ST, Kompenhans J (2017) Particle image velocimetry a practical guide[J]. Experimental Fluid Mechanics 255(3):160–162
Kheradvar A, Rickers C, Morisawa D, Kim M, Hong GR, Pedrizzetti G (2019) Diagnostic and prognostic significance of cardiovascular vortex formation. J Cardiol 74(5):403–411
Liu IS (2003) On the transformation property of the deformation gradient under a change of frame. J Elast 71:73–80
Haller G (2016) Dynamic rotation and stretch tensors from a dynamic polar decomposition. Journal of the Mechanics & Physics of Solids 86:70–93
Asami R, Tanaka T, Ki K et al (2017) Accuracy and limitations of vector flow mapping: left ventricular phantom validation using stereo particle image velocimetory. J Echocardiogr 15:57–66
Wu JZ, Xiong AK, Yang YT (2005) Axial stretching and vortex definition. Phys Fluids 17(3):69–74
Kilner PJ, Yang GZ, Wilkes AJ, Mohiaddin RH, Firmin DN, Yacoub MH (2000) Asymmetric redirection of flow through the heart. Nature. 404(6779):759–761
Bermejo J, Benito Y, Alhama M, Yotti R, Martínez-Legazpi P, del Villar CP, Pérez-David E, González-Mansilla A, Santa-Marta C, Barrio A, Fernández-Avilés F, del Álamo JC (2014) Intraventricular vortex properties in nonischemic dilated cardiomyopathy. American Journal of Physiology-Heart Circulatory Physiology 306(5):H718–H729
Stugaard M, Koriyama H, Katsuki K, Masuda K, Asanuma T, Takeda Y, Sakata Y, Itatani K, Nakatani S (2015) Energy loss in the left ventricle obtained by vector flow mapping as a new quantitative measure of severity of aortic regurgitation: a combined experimental and clinical study. Eur Heart J Cardiovasc Imaging 16(7):723–730
Funding
This work was funded by the National Natural Science Foundation of China (Grant Number 81771927).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yang, K., Wu, S., Zhang, H. et al. Lagrangian-averaged vorticity deviation of spiraling blood flow in the heart during isovolumic contraction and ejection phases. Med Biol Eng Comput 59, 1417–1430 (2021). https://doi.org/10.1007/s11517-021-02366-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-021-02366-2