Abstract
Quality of life following percutaneous coronary intervention (PCI) in patients with coronary artery bypass graft surgery (CABG) has been reported as lower than non-CABG patients, however previous reports pre-date modern developments in PCI and cardiac surgery. This study aimed to examine the 30-day QoL after PCI between patients with and without prior CABG using a contemporary dataset. A retrospective analysis of the Victorian Cardiac Outcomes Registry was undertaken. This study included 36,799 patients who completed the EQ-5D questionnaire that was used to assess the 30-day QoL and was compared between groups with and without prior CABG at baseline. Most of the participants were older than 65 years, more than half were male and had PCI due to acute coronary symptoms (ACS) and nearly 90% of patients received drug eluting stents. Compared to the ‘no prior CABG’ group, the ‘CABG’ group had a significantly higher rate of reporting a health problem (OR 1.30, 95% CI 1.10–1.53), presence of a problem in mobility (OR 1.42, 95% CI 1.15–1.75), personal care (OR 1.49, 95%CI 1.13–1.97) and usual activities (OR 1.39, 95%CI 1.15–1.68), pain/discomfort (OR 1.31, 95%CI 1.11–1.54), and anxiety/depression (OR 1.20, 95%CI 1.02–1.42). Despite modern developments in both PCI and CABG, our study showed a consistent negative association between prior CABG status and 30-day QoL following PCI. There is a need for better targeted cardiac rehabilitation in patients with prior CABG to address their greater relative risk of experiencing poor health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to improvements in medical and therapeutic management, coronary artery disease mortality has been steadily decreasing which has also increased the number of patients who survive and live with an increased risk of having further revascularisation (Moran et al., 2014). Patients with prior coronary artery bypass grafting (CABG) tend to have a high CVD risk profile and high risk of further revascularization due to the progression of atherosclerosis in the native coronary arteries or particularly saphenous vein grafts (Chen et al., 1996). Saphenous vein grafts will be occluded in up to 50% of cases or have a high risk of stenosis within ten years (Fitzgibbon et al., 1996; Goldman et al., 2004). Percutaneous Coronary Intervention (PCI) has been the most common revascularisation procedure in patients with prior CABG (Mohamed et al., 2020; Neumann et al., 2019a) that was associated with better survival relative to redoing CABG. Also, there was no difference in mortality rate between patients with prior CABG compared to those with no prior CABG (Rathod et al., 2020). Prior CABG patients reported an improvement in quality of life (QoL) after PCI although the changes were not as large as the corresponding changes in patients without prior CABG. Still, QoL in the ‘prior CABG’ group remained lower than those in the ‘no prior CABG’ group (Viswanathan et al., 2011; Zając et al., 2016).
The study by Viswanathan et al. (2011) was limited to a small sample of patients with prior CABG (n = 255) and the data were outdated and thus did not account for major advances in pharmacotherapy, PCI techniques (e.g. the use of drug eluting stents), and surgical advances including the use of minimally invasive procedures in recent years. We hypothesised that advances in surgical and PCI techniques may balance QoL post PCI procedure between these two groups. A lack of updated studies have been conducted to compare QoL of patients with and without CABG who experienced a drug eluting stents for a revascularisation. The findings of our study would reflect the impacts of current advances in PCI on quality of life, thus would contribute evidence for intervention on cardiac rehabilitation to improve quality of life in both groups. In this study, we aimed to compare the 30-day QoL after PCI between patients with and without prior CABG in the Victorian Cardiac Outcomes Registry (VCOR).
Methods
Study Design, Setting and Population
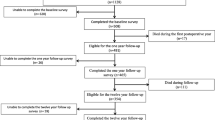
We conducted a retrospective analysis of a prospectively collected registry in Australia. Established in 2012, VCOR is a state-wide population-based PCI clinical quality registry in 25 public and private hospitals in Victoria, Australia (Stub et al., 2018). Patients’ demographic characteristics, medical conditions at admission, PCI procedure details and discharge information were captured through a secure web-based data collection system This current study excluded VCOR patients who died within 30 days post-discharged from PCI (1378 patients) and those who did not complete all five questions of the EQ-5D (25,236 patients). Thus this study included 36,799 patients who underwent PCI and were alive at 30 days post-PCI. In this analysis, included patients were stratified into groups with and without previous CABG at baseline.
Outcome Measurement
Quality of life was measured by the three-level version of the EQ-5D questionnaire at 30 days from discharge. The EQ-5D is a short five-item instrument developed by the EuroQol group, and widely used in quality of life assessment and health economics (Scuffham et al., 2008). The five items are Mobility, Self-Care, Usual Activities, Pain/Discomfort, and Anxiety/Depression. The three levels are defined as no problems, some problems, and inability/extreme problems. The patients were interviewed over the phone and their responses were converted to utility scores using the Australian preference index developed from a discrete choice experiment-derived algorithm (Viney et al., 2014). Under this utility measure, an individual with no problems in all five dimensions had a utility score of 1, whereas individuals with inability/extreme problems in all five dimensions had a utility score of approximately -0.2 in the Australian algorithm (Viney et al., 2014). For analysis, the utility score was categorised into two groups: one group of patients with a utility score of 1 reflecting full health in each of the five dimensions, and one group of patients with a utility score of 0 is a health state equivalent to being dead.
Statistical Analyses
Differences between the ‘previous CABG’ and ‘no CABG’ groups for baseline characteristics were tested by t-tests for continuous variables and Chi-square tests for categorical variables. Logistic regression models were used to estimate the odd ratios (ORs) and corresponding 95% confidence interval (CIs) for the outcomes for participants in the ‘prior CABG’ group compared with those in the ‘no CABG’ group. All of the analyses were adjusted for pre-PCI characteristics including age, sex, BMI, diabetes medications, previous PCI status, a history of cerebrovascular disease, peripheral vascular disease, chronic oral anticoagulant therapies, estimated Glomerular Filtration Rate (eGFR), time from admission to PCI procedures, acute coronary syndrome, cardiogenic shock, out of hospital cardiac arrest, in-hospital pre-procedure cardiac arrest and pre-procedural intubation, and abnormal ejection fraction group (EF < 50%). This first analysis is denoted as Model A. Model B extended model A with further adjustment for PCI characteristics including percutaneous entry location, procedural intubation required, mechanical ventricular support required, lesion location, chronic total occlusion, in-stent restenosis, multivessel, lesion successfully treated, tertile groups of the total number of stents, tertile groups of the total length of stents, type of stents implanted (e.g. drug-eluting stents, plain old balloon angioplasty). Model C further extended model B with adjustment for post-PCI characteristics including new renal impairment, post-procedure dialysis, in-hospital shock, in-hospital MI, major bleeding, planned/unplanned revascularisation, in-hospital stent thrombosis, in-hospital stroke, the use of aspirin, thienopyridine, ticagrelor, beta-blocker, ACE/ARB, statins, other lipid-lowering drugs, and oral anticoagulant therapies. We also included interaction terms in the adjusted logistic models to examine potential modifications of QoL by acute coronary syndrome status and abnormal EF group. A backwards-elimination approach was performed to remove variables that had the largest p-value until all remaining variables had a two-sided p-value of less than 0.20 in the final multivariate models. The presence of collinearity in the final models was assessed with the variance inflation factor (VIF) diagnostic (Hamilton, 2006). We kept the variables with more clinical importance in the models if collinearity was presented. Also, a subgroup analysis by EF functions was performed. All models were weighted to reflect the underlying likelihood of completing the instrument by applying iterative proportional fitting or raking (Bergmann, 2011). The main analysis used a statistical significance threshold of 0.05. The analyses were conducted using Stata (version 15).
Results
Patient Characteristics
As presented in Table 1, on average, included patients were older than 65 years (67 ± 12 years), 76% were male, nearly half of them presented with the acute coronary syndrome and nearly 90% of patients received drug eluting stents. Compared to patients without prior CABG, patients with prior CABG had a higher CVD risk profile with a statistically higher proportion of patients with diabetes medications, previous PCI, a history of cerebrovascular disease or peripheral vascular disease, ejection fraction below 50%. Time from admission to PCI procedure was significantly higher in the ‘prior CABG’ group, with a median of 12 h compared to 5 h in the ‘no prior CABG’ group. Regarding PCI-related characteristics, patients with prior CABG were more likely to have a percutaneous entry from the femoral artery whereas patients without prior CABG were more likely to have a radial entry. A significantly higher proportion of lesions on the left circumflex left main and graft was performed in prior CABG patients. There was no difference in major complications after PCI such as new renal impairment, post-procedure dialysis, in-hospital shock, MI, stroke, major bleeding or stent thrombosis between the ‘prior CABG’ and ‘no prior CABG’ groups.
Regarding the likelihood of completing the EQ-5D questionnaire, patients with the following characteristics were less likely to complete and thus were excluded in this analysis: presentation of an acute coronary syndrome, low ejection fraction, diabetes, a history of cerebrovascular disease, later year of data collection, greater stent length, in-hospital renal impairment, the use of ticagrelor, beta-blockers, aspirin and oral anticoagulant therapy after the PCI procedure. In contrast, included patients were more likely to have baseline chronic oral anticoagulant therapy, chronic total occlusion, a higher number of stents, multivessel, longer door-to-procedure hours, on the treatment of other lipid-lowering therapy rather than statins. More information is provided in Table 2.
Association Between Prior CABG and QoL (Table 3 and 4)
At 30 days following a PCI procedure, 33% of included patients reported a health problem, approximately 15% of the patients reported a problem with mobility, usual activities, pain/discomfort and anxiety/depression whereas only 5% reported a problem with personal care. After adjusting for prior-PCI, PCI and post-PCI characteristics, patients with prior CABG were statistically associated with a higher likelihood of having a health problem with an OR 1.30 (1.10–1.53). Looking at each dimension in isolation, patients with prior CABG had a higher likelihood of problems with mobility with an OR 1.42 (1.15–1.75), personal care with an OR 1.49 (1.13–1.97), usual activities with an OR 1.39 (1.15–1.68), pain/discomfort with an OR 1.31 (1.11–1.54), anxiety/depression with an OR 1.20 (1.02–1.42).
In the subgroup analysis by EF status, patients with normal EF and prior CABG were associated with an increased likelihood of reporting a health problem, mobility, personal care and usual activity as compared to patients with normal EF and no prior CABG whereas patients with abnormal EF and prior CABG were associated with a decreased likelihood of reporting those corresponding outcomes with p for interaction < 0.05 for all models.
Discussion
In our study, most of the participants were older than 65 years, more than half were male and had PCI with an ACS indication. Participants with prior CABG had a higher CVD risk profile compared to those without prior CABG. Despite the majority use of drug eluting stents, the current study showed a significantly higher rate of reporting a health problem, presence of problems with mobility, personal care and usual activity after PCI in patients with prior CABG as compared to those without CABG, particularly in patients with normal EF function. In contrast, patients with prior CABG and abnormal EF function were less likely to report those corresponding outcomes except pain/discomfort or anxiety/depression.
Similar to our results in patients with normal EF function, Viswanathan et al. (2011) observed worse QoL measured by the Nottingham Health profile questionnaire in ‘prior CABG’ group compared to those in the ‘no prior CABG’ group at 3-, 12- and 24-month after PCI given that baseline QoL was similar in all domains (e.g. energy, emotional reaction, sleep and social isolation) except for pain and mobility. Characteristics of patients in this study were similar to our patients although no information about EF function was reported. Patients with a history of congestive heart failure accounted for less than 1% of patients in the study by Viswanathan et al. (2011). Our study observed a lower rate of reporting a problem relating to physical activities in patients with previous CABG and abnormal EF that indicated a potential advantage of PCI on these patients. PCI has previously been shown to improve EF (Buszman et al., 2007; Nozari et al., 2012), these observed effects on QoL may be attributable to the difference in the effect of PCI on EF function between groups with and without prior CABG. Due to a lack of information on post-PCI EF, we were unable to perform further analysis. Regardless of EF functions, our study showed that a history of prior CABG was associated with a higher rate of reporting a problem in pain/discomfort and stress/anxiety. A targeted psychological rehabilitation program for patients with prior CABG may help however such programs remain underutilised due to the nature of urgent PCI for ACS, short time in hospital to prepare for PCI, lack of recommendation for psychological care in current guidelines (Neumann et al., 2019b; Salzmann et al., 2020). A study by Lavie et al. showed the effectiveness of cardiac rehabilitation exercise training programs on improving psychological function in patients with CVD (Lavie et al., 2016). Similarly, some other studies demonstrated the importance of improving fitness on cardiac rehabilitation (Lavie et al., 2019; Tutor et al., 2021). Also, patients were unlikely to receive cardiac rehabilitation after discharge due to lack of perceived need, lack of transport, work/social commitments (Astley et al., 2020; Chindhy et al., 2020; Grace et al., 2008; Neubeck et al., 2012; Redfern et al., 2014; Scott et al., 2003).
Limitations
Our results should be interpreted with some caution. Due to the nature of a post-hoc design, residual confounding is unavoidable. Another limitation of our study is the lack of details of baseline QoL. Prior CABG patients had a higher CVD risk with a higher proportion of patients with diabetic medications, prior PCI, previous CVD and EF < 50. Covariate adjustment for pre- and post-procedure characteristics do not sufficiently control for ‘confounding by indication’. However confounding by indication seemed to bias in favour of worse 30-day QoL in the ‘prior CABG’ group.
In conclusion, despite the use of drug eluting stents, our study showed a consistent negative association between 30-day QoL and prior CABG status. There is a need for better targeted cardiac rehabilitation in patients with prior CABG to address their greater relative risk of experiencing poor health.
Data Availability
Availability of data and materials has been changed to Data availability. Please check if it is correct.
References
Astley, C. M., Chew, D. P., Keech, W., et al. (2020). The impact of cardiac rehabilitation and secondary prevention programs on 12-month clinical outcomes: A linked data analysis. Heart, Lung and Circulation, 29(3), 475–482.
Bergmann, M. (2011). IPFWEIGHT: Stata module to create adjustment weights for surveys.
Buszman, P., Szkróbka, I., Gruszka, A., et al. (2007). Comparison of effectiveness of coronary artery bypass grafting versus percutaneous coronary intervention in patients with ischemic cardiomyopathy. The American Journal of Cardiology, 99(1), 36–41.
Chen, L., Théroux, P., Lespérance, J., Shabani, F., Thibault, B., & de Guise, P. (1996). Angiographic features of vein grafts versus ungrafted coronary arteries in patients with unstable angina and previous bypass surgery. Journal of the American College of Cardiology, 28(6), 1493–1499.
Chindhy, S., Taub, P. R., Lavie, C. J., & Shen, J. (2020). Current challenges in cardiac rehabilitation: Strategies to overcome social factors and attendance barriers. Expert Review of Cardiovascular Therapy, 18(11), 777–789.
Fitzgibbon, G. M., Kafka, H. P., Leach, A. J., Keon, W. J., Hooper, G. D., & Burton, J. R. (1996). Coronary bypass graft fate and patient outcome: Angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. Journal of the American College of Cardiology, 28(3), 616–626.
Goldman, S., Zadina, K., Moritz, T., et al. (2004). Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: Results from a Department of Veterans Affairs Cooperative Study. Journal of the American College of Cardiology, 44(11), 2149–2156.
Grace, S. L., Gravely-Witte, S., Brual, J., et al. (2008). Contribution of patient and physician factors to cardiac rehabilitation enrollment: A prospective multilevel study. European Journal of Preventive Cardiology, 15(5), 548–556.
Hamilton, L. C. (2006). Statistics with Stata (Updated for version 9) Belmont. CA: Thomson-Brooks/Cole.
Lavie, C. J., Menezes, A. R., De Schutter, A., Milani, R. V., & Blumenthal, J. A. (2016). Impact of cardiac rehabilitation and exercise training on psychological risk factors and subsequent prognosis in patients with cardiovascular disease. Canadian Journal of Cardiology, 32(10), S365–S373.
Lavie, C. J., Ozemek, C., Carbone, S., Katzmarzyk, P. T., & Blair, S. N. (2019). Sedentary behavior, exercise, and cardiovascular health. Circulation Research, 124(5), 799–815.
Mohamed, M. O., Shoaib, A., Gogas, B., et al. (2020) Trends of repeat revascularization choice in patients with prior coronary artery bypass surgery. Catheterization and Cardiovascular Interventions.
Moran, A. E., Forouzanfar, M. H., Roth, G. A., et al. (2014). Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: The Global Burden of Disease 2010 study. Circulation, 129(14), 1483–1492.
Neubeck, L., Freedman, S. B., Clark, A. M., Briffa, T., Bauman, A., & Redfern, J. (2012). Participating in cardiac rehabilitation: A systematic review and meta-synthesis of qualitative data. European Journal of Preventive Cardiology, 19(3), 494–503.
Neumann, F.-J., Sousa-Uva, M., Ahlsson, A., et al. (2019a). 2018 ESC/EACTS Guidelines on myocardial revascularization. European Heart Journal, 40(2), 87–165.
Neumann, F. J., Sousa-Uva, M., Ahlsson, A., et al. (2019b). 2018 ESC/EACTS Guidelines on myocardial revascularization. European Heart Journal, 40(2), 87–165. https://doi.org/10.1093/eurheartj/ehy394
Nozari, Y., Oskouei, N. J., Khazaeipour, Z. (2012). Effect of elective percutaneous coronary intervention on left ventricular function in patients with coronary artery disease. Acta Medica Iranica, 26–30.
Rathod, K. S., Beirne, A. M., Bogle, R., et al. (2020). Prior coronary artery bypass graft surgery and outcome after percutaneous coronary intervention: An observational study from the Pan-London percutaneous coronary intervention registry. Journal of the American Heart Association, 9(12), e014409.
Redfern, J., Hyun, K., Chew, D. P., et al. (2014). Prescription of secondary prevention medications, lifestyle advice, and referral to rehabilitation among acute coronary syndrome inpatients: Results from a large prospective audit in Australia and New Zealand. Heart, 100(16), 1281–1288.
Salzmann, S., Salzmann-Djufri, M., Wilhelm, M., & Euteneuer, F. (2020). Psychological preparation for cardiac surgery. Current Cardiology Reports, 22(12), 1–10.
Scott, I. A., Lindsay, K. A., & Harden, H. E. (2003). Utilisation of outpatient cardiac rehabilitation in Queensland. Medical Journal of Australia, 179(7), 341–345.
Scuffham, P. A., Whitty, J. A., Mitchell, A., & Viney, R. (2008). The use of QALY weights for QALY calculations. PharmacoEconomics, 26(4), 297–310.
Stub, D., Lefkovits, J., Brennan, A. L., et al. (2018). The establishment of the Victorian cardiac outcomes registry (VCOR): Monitoring and optimising outcomes for cardiac patients in Victoria. Heart, Lung and Circulation, 27(4), 451–463.
Tutor, A., Lavie, C. J., Kachur, S., Dinshaw, H., Milani, R. V. (2021). Impact of cardiorespiratory fitness on outcomes in cardiac rehabilitation. Progress in Cardiovascular Diseases.
Viney, R., Norman, R., Brazier, J., et al. (2014). an Australian discrete choice experiment to value EQ-5D health states. Health Economics, 23(6), 729–742.
Viswanathan, G. N., Mayurathan, G., Hildreth, T., Worthley, S. G., & Zaman, A. G. (2011). Health related quality of life after percutaneous coronary revascularisation in patients with previous coronary artery bypass grafts: A two-year follow up study. Applied Research in Quality of Life, 6(3), 311–324.
Zając, P., Życiński, P., Qawoq, H., et al. (2016). Outcomes of percutaneous coronary intervention in patients after previous coronary artery bypass surgery. Kardiologia Polska (polish Heart Journal), 74(4), 322–330.
Acknowledgements
The researchers gratefully acknowledge NHMRC Centre of Research Excellence in Cardiovascular Outcomes Improvement for their support of this project.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions We received funding from NHMRC Centre of Research Excellence in Cardiovascular Outcomes Improvements (GNT: 1111170) and the EuroQoL Foundation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data cleaning and analysis were performed by CH, SS and RN. The first draft of the manuscript was written by CH. Each author contributed important intellectual content during manuscript drafting or revision, accepts personal accountability for the author’s own contributions, and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was approved by the Human Research Ethics Committee at Curtin University.
Competing Interests
CMR is supported by an NHMRC Principal Research Fellowship (1136372). For the remaining authors, none is correct.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ho, C.L.B., Brennan, A., Dinh, D.T. et al. Prior Coronary Artery Bypass Graft Surgery Impacts 30-day Quality of Life after Percutaneous Coronary Intervention: Evidence from the Victorian Cardiac Outcomes Registry (VCOR). Applied Research Quality Life 17, 3415–3426 (2022). https://doi.org/10.1007/s11482-022-10071-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-022-10071-x