Abstract
Controlling and treating biofilm-related infections is challenging because of the widespread presence of multidrug-resistant microbes. Biofilm, a naturally occurring matrix of microbial aggregates, has developed intricate and diverse resistance mechanisms against many currently used antibiotics. This poses a significant problem, especially for human health, including clinically chronic infectious diseases. Thus, there is an urgent need to search for and develop new and more effective antibiotics. As the marine environment is recognized as a promising reservoir of new biologically active molecules with potential pharmacological properties, marine natural products, particularly those of microbial origin, have emerged as a promising source of antibiofilm agents. Marine microbes represent an untapped source of secondary metabolites with antimicrobial activity. Furthermore, marine natural products, owing to their self-defense mechanisms and adaptation to harsh conditions, encompass a wide range of chemical compounds, including peptides and polyketides, which are primarily found in microbes. These molecules can be exploited to provide novel and unique structures for developing alternative antibiotics as effective antibiofilm agents. This review focuses on the possible antibiofilm mechanism of these marine microbial molecules against biofilm-forming pathogens. It provides an overview of biofilm development, its recalcitrant mode of action, strategies for the development of antibiofilm agents, and their assessments. The review also revisits some selected peptides and polyketides from marine microbes reported between 2016 and 2023, highlighting their moderate and considerable antibiofilm activities. Moreover, their antibiofilm mechanisms, such as adhesion modulation/inhibition targeting biofilm-forming pathogens, quorum sensing intervention and inhibition, and extracellular polymeric substance disruption, are highlighted herein.
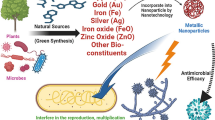
Graphical abstract




Similar content being viewed by others
References
Jamal M, Ahmad W, Andleeb S et al (2018) Bacterial biofilm and associated infections. J Chin Med Assoc 81:7–11. https://doi.org/10.1016/j.jcma.2017.07.012
Sun F, Qu F, Ling Y et al (2013) Biofilm-associated infections: antibiotic resistance and novel therapeutic strategies. Future Microbiol 8:877–886. https://doi.org/10.2217/fmb.13.58
Nobile CJ, Johnson AD (2015) Candida albicans biofilms and human disease. Annu Rev Microbiol 69:71–92. https://doi.org/10.1146/annurev-micro-091014-104330
Patel NB, Hinojosa JA, Zhu M, Robertson DM (2018) Acceleration of the formation of biofilms on contact lens surfaces in the presence of neutrophil-derived cellular debris is conserved across multiple genera. Mol Vis 24:94–104
Song Z, Borgwardt L, Høiby N et al (2013) Prosthesis infections after orthopedic joint replacement: the possible role of bacterial biofilms. Orthop Rev (Pavia) 5:65–71. https://doi.org/10.4081/or.2013.e14
Lauten A, Martinović M, Kursawe L et al (2021) Bacterial biofilms in infective endocarditis: an in vitro model to investigate emerging technologies of antimicrobial cardiovascular device coatings. Clin Res Cardiol 110:323–331. https://doi.org/10.1007/s00392-020-01669-y
Stickler DJ (2014) Clinical complications of urinary catheters caused by crystalline biofilms: something needs to be done. J Intern Med 276:120–129. https://doi.org/10.1111/joim.12220
Gominet M, Compain F, Beloin C, Lebeaux D (2017) Central venous catheters and biofilms: where do we stand in 2017? APMIS 125:365–375. https://doi.org/10.1111/apm.12665
Pelling H, Nzakizwanayo J, Milo S et al (2019) Bacterial biofilm formation on indwelling urethral catheters. Lett Appl Microbiol 68:277–293. https://doi.org/10.1111/lam.13144
Štefánek M, Wenner S, Borges V et al (2022) Antimicrobial resistance and biofilms underlying catheter-related bloodstream coinfection by Enterobacter cloacae complex and Candida parapsilosis. Antibiotics 11:1245. https://doi.org/10.3390/antibiotics11091245
Hahnel S (2017) Biofilms on dental implants. In: Deng Y, Lv W (eds) Biofilms and implantable medical devices: infection and control. Woodhead Publishing, pp 117–140
Dhaliwal JS, Abd Rahman NA, Ming LC et al (2021) Microbial biofilm decontamination on dental implant surfaces: a mini review. Front Cell Infect Microbiol 11:736186. https://doi.org/10.3389/fcimb.2021.736186
Minkiewicz-Zochniak A, Jarzynka S, Iwańska A et al (2021) Biofilm formation on dental implant biomaterials by Staphylococcus aureus strains isolated from patients with cystic fibrosis. Materials (Basel) 14:2030. https://doi.org/10.3390/ma14082030
Costa RC, Bertolini M, Costa Oliveira BE et al (2023) Polymicrobial biofilms related to dental implant diseases: unravelling the critical role of extracellular biofilm matrix. Crit Rev Microbiol 49:370–390. https://doi.org/10.1080/1040841X.2022.2062219
Vieira Colombo AP, Magalhães CB, Hartenbach FARR et al (2016) Periodontal-disease-associated biofilm: a reservoir for pathogens of medical importance. Microb Pathog 94:27–34. https://doi.org/10.1016/j.micpath.2015.09.009
De A, Raj HJ, Maiti PK (2016) Biofilm in osteomyelitis caused by a rare pathogen, Morganella morganii: a case report. J Clin Diagn Res 10:DD06–DD08. https://doi.org/10.7860/JCDR/2016/18666.7990
Masters EA, Trombetta RP, de Mesy Bentley KL et al (2019) Evolving concepts in bone infection: redefining “biofilm”, “acute vs. chronic osteomyelitis”, “the immune proteome” and “local antibiotic therapy.” Bone Res 7:20. https://doi.org/10.1038/s41413-019-0061-z
Edmiston CE Jr, McBain AJ, Roberts C, Leaper D (2015) Clinical and microbiological aspects of biofilm-associated surgical site infections. In: Donelli G (ed) Biofilm-based healthcare-associated infections, vol I. Advances in Experimental Medicine and Biology 830. Springer International Publishing, Switzerland, pp 69–84
Percival SL, McCarty SM, Lipsky B (2015) Biofilms and wounds: an overview of the evidence. Adv Wound Care 4:373–381. https://doi.org/10.1089/wound.2014.0557
Maslova E, Eisaiankhongi L, Sjöberg F, McCarthy RR (2021) Burns and biofilms: priority pathogens and in vivo models. NPJ Biofilms Microbiomes 7:73. https://doi.org/10.1038/s41522-021-00243-2
Srivastava S, Bhargava A (2016) Biofilms and human health. Biotechnol Lett 38:1–22. https://doi.org/10.1007/s10529-015-1960-8
Stewart PS, Bjarnsholt T (2020) Risk factors for chronic biofilm-related infection associated with implanted medical devices. Clin Microbiol Infect 26:1034–1038. https://doi.org/10.1016/j.cmi.2020.02.027
Flemming HC, Wingender J, Szewzyk U et al (2016) Biofilms: an emergent form of bacterial life. Nat Rev Microbiol 14:563–575. https://doi.org/10.1038/nrmicro.2016.94
Karygianni L, Ren Z, Koo H, Thurnheer T (2020) Biofilm matrixome: extracellular components in structured microbial communities. Trends Microbiol 28:668–681. https://doi.org/10.1016/j.tim.2020.03.016
Berlanga M, Guerrero R (2016) Living together in biofilms: the microbial cell factory and its biotechnological implications. Microb Cell Fact 15:165. https://doi.org/10.1186/s12934-016-0569-5
de Carvalho CCCR (2018) Marine biofilms: a successful microbial strategy with economic implications. Front Mar Sci 5:126. https://doi.org/10.3389/fmars.2018.00126
Telegdi J, Shaban A, Trif L (2020) Review on the microbiologically influenced corrosion and the function of biofilms. Int J Corros Scale Inhib 9:1–33. https://doi.org/10.17675/2305-6894-2020-9-1-1
Zhao X, Zhao F, Wang J, Zhong N (2017) Biofilm formation and control strategies of foodborne pathogens: food safety perspectives. RSC Adv 7:36670–36683. https://doi.org/10.1039/C7RA02497E
Kathju S, Nistico L, Tower I et al (2014) Bacterial biofilms on implanted suture material are a cause of surgical site infection. Surg Infect (Larchmt) 15:592–600. https://doi.org/10.1089/sur.2013.016
Ciofu O, Rojo-Molinero E, Macià MD, Oliver A (2017) Antibiotic treatment of biofilm infections. APMIS 125:304–319. https://doi.org/10.1111/apm.12673
Dostert M, Belanger CR, Hancock REW (2019) Design and assessment of anti-biofilm peptides: steps toward clinical application. J Innate Immun 11:193–204. https://doi.org/10.1159/000491497
Carroll AR, Copp BR, Davis RA et al (2022) Marine natural products. Nat Prod Rep 39:1122–1171. https://doi.org/10.1039/D1NP00076D
Habbu P, Warad V, Shastri R et al (2016) Antimicrobial metabolites from marine microorganisms. Chin J Nat Med 14:101–116. https://doi.org/10.1016/S1875-5364(16)60003-1
Andryukov B, Mikhailov V, Besednova N (2019) The biotechnological potential of secondary metabolites from marine bacteria. J Mar Sci Eng 7:176. https://doi.org/10.3390/jmse7060176
Stowe SD, Richards JJ, Tucker AT et al (2011) Anti-biofilm compounds derived from marine sponges. Mar Drugs 9:2010–2035. https://doi.org/10.3390/md9102010
Blackedge MS, Worthington RJ, Melander C (2013) Biologically inspired strategies for combating bacterial biofilms. Curr Opin Pharmacol 13:699–706. https://doi.org/10.1016/j.coph.2013.07.004
Rabin N, Zheng Y, Opoku-Temeng C et al (2015) Agents that inhibit bacterial biofilm formation. Future Med Chem 7:647–671. https://doi.org/10.2307/j.ctvnwc0d0.18
Ćirić AD, Petrović JD, Glamočlija JM et al (2019) Natural products as biofilm formation antagonists and regulators of quorum sensing functions: a comprehensive review update and future trends. S Afr J Bot 120:65–80. https://doi.org/10.1016/j.sajb.2018.09.010
Melander RJ, Basak AK, Melander C (2020) Natural products as inspiration for the development of bacterial antibiofilm agents. Nat Prod Rep 37:1454–1477. https://doi.org/10.1039/d0np00022a
Mishra R, Panda AK, De Mandal S et al (2020) Natural anti-biofilm agents: strategies to control biofilm-forming pathogens. Front Microbiol 11:566325. https://doi.org/10.3389/fmicb.2020.566325
Deng Y, Liu Y, Li J et al (2022) Marine natural products and their synthetic analogs as promising antibiofilm agents for antibiotics discovery and development. Eur J Med Chem 239:114513. https://doi.org/10.1016/j.ejmech.2022.114513
Wang KL, Dou ZR, Gong GF et al (2022) Anti-larval and anti-algal natural products from marine microorganisms as sources of anti-biofilm agents. Mar Drugs 20:90. https://doi.org/10.3390/md20020090
Doiron K, Beaulieu L, St-Louis R, Lemarchand K (2018) Reduction of bacterial biofilm formation using marine natural antimicrobial peptides. Colloids Surf B Biointerfaces 167:524–530. https://doi.org/10.1016/j.colsurfb.2018.04.051
Galdiero E, Lombardi L, Falanga A et al (2019) Biofilms: novel strategies based on antimicrobial peptides. Pharmaceutics 11:322. https://doi.org/10.3390/pharmaceutics11070322
Duraisamy S, Balakrishnan S, Ranjith S et al (2020) Bacteriocin—a potential antimicrobial peptide towards disrupting and preventing biofilm formation in the clinical and environmental locales. Environ Sci Pollut Res Int 27:44922–44936. https://doi.org/10.1007/s11356-020-10989-5
Dostert M, Trimble MJ, Hancock REW (2021) Antibiofilm peptides: overcoming biofilm-related treatment failure. RSC Adv 11:2718–2728. https://doi.org/10.1039/d0ra09739j
Castillo-Juárez I, Blancas-Luciano BE, García-Contreras R, Fernández-Presas AM (2022) Antimicrobial peptides properties beyond growth inhibition and bacterial killing. PeerJ 10:e12667. https://doi.org/10.7717/peerj.12667
Nicolas M, Beito B, Oliveira M et al (2021) Strategies for antimicrobial peptides immobilization on surfaces to prevent biofilm growth on biomedical devices. Antibiotics 11:13. https://doi.org/10.3390/antibiotics11010013
Patra A, Das J, Agrawal NR et al (2022) Marine antimicrobial peptides-based strategies for tackling bacterial biofilm and biofouling challenges. Molecules 27:7546. https://doi.org/10.3390/molecules27217546
Safronova VN, Bolosov IA, Kruglikov RN et al (2022) Novel β-hairpin peptide from marine polychaeta with a high efficacy against gram-negative pathogens. Mar Drugs 20:1–19. https://doi.org/10.3390/md20080517
Wang H, Fewer DP, Holm L et al (2014) Atlas of nonribosomal peptide and polyketide biosynthetic pathways reveals common occurrence of nonmodular enzymes. Proc Natl Acad Sci USA 111:9259–9264. https://doi.org/10.1073/pnas.1401734111
Agrawal S, Acharya D, Adholeya A et al (2017) Nonribosomal peptides from marine microbes and their antimicrobial and anticancer potential. Front Pharmacol 8:828. https://doi.org/10.3389/fphar.2017.00828
Hudson GA, Mitchell DA (2018) RiPP antibiotics: biosynthesis and engineering potential. Curr Opin Microbiol 45:61–69. https://doi.org/10.1016/j.mib.2018.02.010
Beck C, Garzón JFG, Weber T (2020) Recent advances in re-engineering modular PKS and NRPS assembly lines. Biotechnol Bioproc E 25:886–894. https://doi.org/10.1007/s12257-020-0265-5
Kimkes TEP, Heinemann M (2020) How bacteria recognise and respond to surface contact. FEMS Microbiol Rev 44:106–122. https://doi.org/10.1093/femsre/fuz029
Bhardwaj AK, Vinothkumar K, Rajpara N (2013) Bacterial quorum sensing inhibitors: attractive alternatives for control of infectious pathogens showing multiple drug resistance. Recent Pat Antiinfect Drug Discov 8:68–83. https://doi.org/10.2174/1574891x11308010012
Otto M (2013) Staphylococcal infections: mechanisms of biofilm maturation and detachment as critical determinants of pathogenicity. Annu Rev Med 64:175–188. https://doi.org/10.1146/annurev-med-042711-140023
Taglialegna A, Navarro S, Ventura S et al (2016) Staphylococcal bap proteins build amyloid scaffold biofilm matrices in response to environmental signals. PLoS Pathog 12:e1005711. https://doi.org/10.1371/journal.ppat.1005711
Solano C, Echeverz M, Lasa I (2014) Biofilm dispersion and quorum sensing. Curr Opin Microbiol 18:96–104. https://doi.org/10.1016/j.mib.2014.02.008
Hengge R, Gründling A, Jenal U et al (2016) Bacterial signal transduction by cyclic di-GMP and other nucleotide second messengers. J Bacteriol 198:15–26. https://doi.org/10.1128/JB.00331-15
Olsen I (2015) Biofilm-specific antibiotic tolerance and resistance. Eur J Clin Microbiol Infect Dis 34:877–886. https://doi.org/10.1007/s10096-015-2323-z
Stewart PS (2015) Antimicrobial tolerance in biofilms. Microbiol Spectr. https://doi.org/10.1128/9781555817466.ch13
Ciofu O, Moser C, Jensen PØ, Høiby N (2022) Tolerance and resistance of microbial biofilms. Nat Rev Microbiol 20:621–635. https://doi.org/10.1038/s41579-022-00682-4
Hall CW, Mah TF (2017) Molecular mechanisms of biofilm-based antibiotic resistance and tolerance in pathogenic bacteria. FEMS Microbiol Rev 41:276–301. https://doi.org/10.1093/femsre/fux010
Darby EM, Trampari E, Siasat P et al (2023) Molecular mechanisms of antibiotic resistance revisited. Nat Rev Microbiol 21:280–295. https://doi.org/10.1038/s41579-022-00820-y
Brauner A, Fridman O, Gefen O, Balaban NQ (2016) Distinguishing between resistance, tolerance and persistence to antibiotic treatment. Nat Rev Microbiol 14:320–330. https://doi.org/10.1038/nrmicro.2016.34
Hathroubi S, Mekni MA, Domenico P et al (2017) Biofilms: microbial shelters against antibiotics. Microb Drug Resist 23:147–156. https://doi.org/10.1089/mdr.2016.0087
Singh S, Singh SK, Chowdhury I, Singh R (2017) Understanding the mechanism of bacterial biofilms resistance to antimicrobial agents. Open Microbiol J 11:53–62. https://doi.org/10.2174/1874285801711010053
Jennings LK, Storek KM, Ledvina HE et al (2015) Pel is a cationic exopolysaccharide that cross-links extracellular DNA in the Pseudomonas aeruginosa biofilm matrix. Proc Natl Acad Sci U S A 112:11353–11358. https://doi.org/10.1073/pnas.1503058112
Wood TK, Knabel SJ, Kwan BW (2013) Bacterial persister cell formation and dormancy. Appl Environ Microbiol 79:7116–7121. https://doi.org/10.1128/AEM.02636-13
Kester JC, Fortune SM (2014) Persisters and beyond: mechanisms of phenotypic drug resistance and drug tolerance in bacteria. Crit Rev Biochem Mol Biol 49:91–101. https://doi.org/10.3109/10409238.2013.869543
van den Bergh B, Fauvart M, Michiels J (2017) Formation, physiology, ecology, evolution and clinical importance of bacterial persisters. FEMS Microbiol Rev 41:219–251. https://doi.org/10.1093/femsre/fux001
Yang S, Hay ID, Cameron DR et al (2015) Antibiotic regimen based on population analysis of residing persister cells eradicates Staphylococcus epidermidis biofilms. Sci Rep 5:18578. https://doi.org/10.1038/srep18578
Bjarnsholt T, Jensen PØ, Burmølle M et al (2005) Pseudomonas aeruginosa tolerance to tobramycin, hydrogen peroxide and polymorphonuclear leukocytes is quorum-sensing dependent. Microbiology 151:373–383. https://doi.org/10.1099/mic.0.27463-0
Chua SL, Yam JKH, Hao P et al (2016) Selective labelling and eradication of antibiotic-tolerant bacterial populations in Pseudomonas aeruginosa biofilms. Nat Commun 7:10750. https://doi.org/10.1038/ncomms10750
Yarwood JM, Bartels DJ, Volper EM, Greenberg EP (2004) Quorum sensing in Staphylococcus aureus biofilms. J Bacteriol 186:1838–1850. https://doi.org/10.1128/JB.186.6.1838-1850.2004
Dale JL, Cagnazzo J, Phan CQ et al (2015) Multiple roles for Enterococcus faecalis glycosyltransferases in biofilm-associated antibiotic resistance, cell envelope integrity, and conjugative transfer. Antimicrob Agents Chemother 59:4094–4105. https://doi.org/10.1128/AAC.00344-15
Hazan R, Que YA, Maura D et al (2016) Auto poisoning of the respiratory chain by a quorum-sensing-regulated molecule favors biofilm formation and antibiotic tolerance. Curr Biol 26:195–206. https://doi.org/10.1016/j.cub.2015.11.056
Dam S, Pagès JM, Masi M (2018) Stress responses, outer membrane permeability control and antimicrobial resistance in Enterobacteriaceae. Microbiology 164:260–267. https://doi.org/10.1099/mic.0.000613
Liao J, Schurr MJ, Sauer K (2013) The MerR-like regulator BrlR confers biofilm tolerance by activating multidrug efflux pumps in Pseudomonas aeruginosa biofilms. J Bacteriol 195:3352–3363. https://doi.org/10.1128/JB.00318-13
Chambers JR, Sauer K (2013) The MerR-like regulator BrlR impairs Pseudomonas aeruginosa biofilm tolerance to colistin by repressing PhoPQ. J Bacteriol 195:4678–4688. https://doi.org/10.1128/JB.00834-13
Rojo-Molinero E, MacIà MD, Oliver A (2019) Social behavior of antibiotic resistant mutants within Pseudomonas aeruginosa biofilm communities. Front Microbiol 10:570. https://doi.org/10.3389/fmicb.2019.00570
Xu Q, Hu X, Wang Y (2021) Alternatives to conventional antibiotic therapy: potential therapeutic strategies of combating antimicrobial-resistance and biofilm-related infections. Mol Biotechnol 63:1103–1124. https://doi.org/10.1007/s12033-021-00371-2
Wilson C, Lukowicz R, Merchant S et al (2017) Quantitative and qualitative assessment methods for biofilm growth: a mini-review. Res Rev J EngTechnol 6:1–25
Haney EF, Trimble MJ, Cheng JT et al (2018) Critical assessment of methods to quantify biofilm growth and evaluate antibiofilm activity of host defence peptides. Biomolecules 8:29. https://doi.org/10.3390/biom8020029
Haney EF, Trimble MJ, Hancock REW (2021) Microtiter plate assays to assess antibiofilm activity against bacteria. Nat Protoc 16:2615–2632. https://doi.org/10.1038/s41596-021-00515-3
Skogman ME, Vuorela PM, Fallarero A (2016) A platform of anti-biofilm assays suited to the exploration of natural compound libraries. J Vis Exp 118:e54829. https://doi.org/10.3791/54829
Van Dijck P, Sjollema J, Cammue BPA et al (2018) Methodologies for in vitro and in vivo evaluation of efficacy of antifungal and antibiofilm agents and surface coatings against fungal biofilms. Microb Cell 5:300–326. https://doi.org/10.15698/mic2018.07.638
Laverty G, McCloskey AP, Gorman SP, Gilmore BF (2015) Anti-biofilm activity of ultrashort cinnamic acid peptide derivatives against medical device-related pathogens. J Pept Sci 21:770–778. https://doi.org/10.1002/psc.2805
Azeredo J, Azevedo NF, Briandet R et al (2017) Critical review on biofilm methods. Crit Rev Microbiol 43:313–351. https://doi.org/10.1080/1040841X.2016.1208146
Silva NBS, Marques LA, Röder DDB (2021) Diagnosis of biofilm infections: current methods used, challenges and perspectives for the future. J Appl Microbiol 131:2148–2160. https://doi.org/10.1111/jam.15049
An AY, Choi KYG, Baghela AS, Hancock REW (2021) An overview of biological and computational methods for designing mechanism-informed anti-biofilm agents. Front Microbiol 12:640787. https://doi.org/10.3389/fmicb.2021.640787
Roy R, Tiwari M, Donelli G, Tiwari V (2018) Strategies for combating bacterial biofilms: a focus on anti-biofilm agents and their mechanisms of action. Virulence 9:522–554. https://doi.org/10.1080/21505594.2017.1313372
Vandecandelaere I, Van Acker H, Coenye T (2016) A microplate-based system as in vitro model of biofilm growth and quantification. In: Michiels J, Fauvart M (eds) Bacterial persistence: methods and protocols, methods in molecular biology. Humana Press, New York, pp 53–66
Tang PC, Eriksson O, Sjögren J et al (2022) A microfluidic chip for studies of the dynamics of antibiotic resistance selection in bacterial biofilms. Front Cell Infect Microbiol 12:896149. https://doi.org/10.3389/fcimb.2022.896149
Barrila J, Crabbé A, Yang J et al (2018) Modeling host-pathogen interactions in the context of the microenvironment: three-dimensional cell culture comes of age. Infect Immun 86:e00282-e318. https://doi.org/10.1128/IAI.00282-18
Lebeaux D, Chauhan A, Rendueles O, Beloin C (2013) From in vitro to in vivo models of bacterial biofilm-related infections. Pathogens 2:288–356. https://doi.org/10.3390/pathogens2020288
Balan SS, Kumar CG, Jayalakshmi S (2016) Pontifactin, a new lipopeptide biosurfactant produced by a marine Pontibacter korlensis strain SBK-47: purification, characterization and its biological evaluation. Process Biochem 51:2198–2207. https://doi.org/10.1016/j.procbio.2016.09.009
Paraszkiewicz K, Moryl M, Płaza G et al (2021) Surfactants of microbial origin as antibiofilm agents. Int J Environ Health Res 31:401–420. https://doi.org/10.1080/09603123.2019.1664729
Bjerk TR, Severino P, Jain S et al (2021) Biosurfactants: properties and applications in drug delivery, biotechnology and ecotoxicology. Bioengineering 8:115. https://doi.org/10.3390/bioengineering8080115
Théatre A, Cano-Prieto C, Bartolini M et al (2021) The surfactin-like lipopeptides from Bacillus spp.: natural biodiversity and synthetic biology for a broader application range. Front Bioeng Biotechnol 9:623701. https://doi.org/10.3389/fbioe.2021.623701
De Zoysa GH, Cameron AJ, Hegde VV et al (2015) Antimicrobial peptides with potential for biofilm eradication: synthesis and structure activity relationship studies of battacin peptides. J Med Chem 58:625–639. https://doi.org/10.1021/jm501084q
De Zoysa GH, Sarojini V (2017) Feasibility study exploring the potential of novel battacin lipopeptides as antimicrobial coatings. ACS Appl Mater Interfaces 9:1373–1383. https://doi.org/10.1021/acsami.6b15859
Mohammadi M, Taheri B, Momenzadeh N et al (2018) Identification and characterization of novel antimicrobial peptide from Hippocampus comes by in silico and experimental studies. Mar Biotechnol 20:718–728. https://doi.org/10.1371/journal.pone.0206578
Xiu P, Liu R, Zhang D, Sun C (2017) Pumilacidin-like lipopeptides derived from marine bacterium Bacillus sp. strain 176 suppress the motility of Vibrio alginolyticus. Appl Environ Microbiol 83:e00450-e517. https://doi.org/10.1128/AEM.00450-17
Pereira de Melo FM, Fiore MF, Beraldo de Moraes LA et al (2009) Antifungal compound produced by the cassava endophyte Bacillus pumilus MAIIIM4A. Sci Agric 66:583–592
Liu R, Zheng R, Liu G, Sun C (2020) The cyclic lipopeptides suppress the motility of Vibrio alginolyticus via targeting the Na+-driven flagellar motor component MotX. Environ Microbiol 22:4424–4437. https://doi.org/10.1111/1462-2920.15144
Chou S, Guo H, Zingl FG et al (2023) Synthetic peptides that form nanostructured micelles have potent antibiotic and antibiofilm activity against polymicrobial infections. Proc Natl Acad Sci USA 120:e2219679120. https://doi.org/10.1073/pnas.2219679120
De La Fuente-Núñez C, Korolik V, Bains M et al (2012) Inhibition of bacterial biofilm formation and swarming motility by a small synthetic cationic peptide. Antimicrob Agents Chemother 56:2696–2704. https://doi.org/10.1128/AAC.00064-12
Wang J, Nong XH, Zhang XY et al (2017) Screening of anti-biofilm compounds from marine-derived fungi and the effects of secalonic acid D on Staphylococcus aureus biofilm. J Microbiol Biotechnol 27:1078–1089. https://doi.org/10.4014/jmb.1609.09053
Bao J, Sun YL, Zhang XY et al (2013) Antifouling and antibacterial polyketides from marine gorgonian coral-associated fungus Penicillium sp. SCSGAF 0023. J Antibiot (Tokyo) 66:219–223. https://doi.org/10.1038/ja.2012.110
Lee JH, Kim YG, Yong Ryu S, Lee J (2016) Calcium-chelating alizarin and other anthraquinones inhibit biofilm formation and the hemolytic activity of Staphylococcus aureus. Sci Rep 6:19267. https://doi.org/10.1038/srep19267
Coenye T, Honraet K, Rigole P et al (2007) In vitro inhibition of Streptococcus mutans biofilm formation on hydroxyapatite by subinhibitory concentrations of anthraquinones. Antimicrob Agents Chemother 51:1541–1544. https://doi.org/10.1128/AAC.00999-06
Alves DS, Pérez-Fons L, Estepa A, Micol V (2004) Membrane-related effects underlying the biological activity of the anthraquinones emodin and barbaloin. Biochem Pharmacol 68:549–561. https://doi.org/10.1016/j.bcp.2004.04.012
Xiang H, Cao F, Ming D et al (2017) Aloe-emodin inhibits Staphylococcus aureus biofilms and extracellular protein production at the initial adhesion stage of biofilm development. Appl Microbiol Biotechnol 101:6671–6681. https://doi.org/10.1007/s00253-017-8403-5
Ansari JM, Abraham NM, Massaro J et al (2017) Anti-biofilm activity of a self-aggregating peptide against Streptococcus mutans. Front Microbiol 8:488. https://doi.org/10.3389/fmicb.2017.00488
de Carvalho MP, Abraham W-R (2012) Antimicrobial and biofilm inhibiting diketopiperazines. Curr Med Chem 19:3564–3577. https://doi.org/10.2174/092986712801323243
Mishra AK, Choi J, Choi SJ, Baek KH (2017) Cyclodipeptides: an overview of their biosynthesis and biological activity. Molecules 22:1796. https://doi.org/10.3390/molecules22101796
Sun S, Dai X, Sun J et al (2016) A diketopiperazine factor from Rheinheimera aquimaris QSI02 exhibits anti-quorum sensing activity. Sci Rep 6:39637. https://doi.org/10.1038/srep39637
Yu X, Li L, Sun S et al (2021) A cyclic dipeptide from marine fungus Penicillium chrysogenum DXY-1 exhibits anti-quorum sensing activity. ACS Omega 6:7693–7700. https://doi.org/10.1021/acsomega.1c00020
Holden MTG, Chhabra SR, De Nys R et al (1999) Quorum-sensing cross talk: isolation and chemical characterization of cyclic dipeptides from Pseudomonas aeruginosa and other Gram-negative bacteria. Mol Microbiol 33:1254–1266. https://doi.org/10.1046/j.1365-2958.1999.01577.x
Papaioannou E, Utari PD, Quax WJ (2013) Choosing an appropriate infection model to study quorum sensing inhibition in Pseudomonas infections. Int J Mol Sci 14:19309–19340. https://doi.org/10.3390/ijms140919309
Kiran GS, Priyadharsini S, Sajayan A et al (2017) Production of lipopeptide biosurfactant by a marine Nesterenkonia sp. and its application in food industry. Front Microbiol 8:1138. https://doi.org/10.3389/fmicb.2017.01138
Kiran GS, Sajayan A, Priyadharshini G et al (2021) A novel anti-infective molecule nesfactin identified by sponge associated bacteria Nesterenkonia sp. MSA31 against multidrug resistant Pseudomonas aeruginosa. Microb Pathog 157:104923. https://doi.org/10.1016/j.micpath.2021.104923
O’Gara JP (2007) ica and beyond: biofilm mechanisms and regulation in Staphylococcus epidermidis and Staphylococcus aureus. FEMS Microbiol Lett 270:179–188. https://doi.org/10.1111/j.1574-6968.2007.00688.x
Lauderdale KJ, Boles BR, Cheung AL, Horswill AR (2009) Interconnections between sigma b, agr, and proteolytic activity in Staphylococcus aureus biofilm maturation. Infect Immun 77:1623–1635. https://doi.org/10.1128/IAI.01036-08
Taha MN, Saafan AE, Ahmedy A et al (2019) Two novel synthetic peptides inhibit quorum sensing-dependent biofilm formation and some virulence factors in Pseudomonas aeruginosa PAO1. J Microbiol 57:618–625. https://doi.org/10.1007/s12275-019-8548-2
de Oliveira Filho JWG, Islam MT, Ali ES et al (2017) A comprehensive review on biological properties of citrinin. Food Chem Toxicol 110:130–141. https://doi.org/10.1016/j.fct.2017.10.002
Sabdaningsih A, Liu Y, Mettal U et al (2020) A new citrinin derivative from the Indonesian marine sponge-associated fungus Penicillium citrinum. Mar Drugs 18:227. https://doi.org/10.3390/md18040227
Ooi N, Eady EA, Cove JH, O’Neill AJ (2015) Redox-active compounds with a history of human use: antistaphylococcal action and potential for repurposing as topical antibiofilm agents. J Antimicrob Chemother 70:479–488. https://doi.org/10.1093/jac/dku409
Poh WH, Rice SA (2022) Recent developments in nitric oxide donors and delivery for antimicrobial and anti-biofilm applications. Molecules 27:674. https://doi.org/10.3390/molecules27030674
Yepuri NR, Barraud N, Mohammadi NS et al (2013) Synthesis of cephalosporin-3′-diazeniumdiolates: biofilm dispersing NO-donor prodrugs activated by β-lactamase. Chem Commun 49:4791–4793. https://doi.org/10.1039/c3cc40869h
Rineh A, Soren O, McEwan T et al (2020) Discovery of cephalosporin-3′-diazeniumdiolates that show dual antibacterial and antibiofilm effects against Pseudomonas aeruginosa clinnical cystic fibrosis isolates and efficacy in a murine respiratory infection model. ACS Infect Dis 6:1460–1479. https://doi.org/10.1021/acsinfecdis.0c00070
Qader MM, Hamed AA, Soldatou S et al (2021) Antimicrobial and antibiofilm activities of the fungal metabolites isolated from the marine endophytes Epicoccum nigrum M13 and Alternaria alternata 13A. Mar Drugs 19:232. https://doi.org/10.3390/MD19040232
Kumla D, Dethoup T, Gales L et al (2019) Erubescensoic acid, a new polyketide and a xanthonopyrone SPF-3059-26 from the culture of the marine sponge-associated fungus Penicillium erubescens KUFA 0220 and antibacterial activity evaluation of some of its constituents. Molecules 24:208. https://doi.org/10.3390/molecules24010208
Leetanasaksakul K, Koomsiri W, Suga T et al (2022) Sattahipmycin, a hexacyclic xanthone produced by a marine-derived Streptomyces. J Nat Prod 85:1211–1217. https://doi.org/10.1021/acs.jnatprod.1c00870
Mohamed SS, Abdelhamid SA, Ali RH (2021) Isolation and identification of marine microbial products. J Genet Eng Biotechnol 19:162. https://doi.org/10.1186/s43141-021-00259-3
Lahiri D, Nag M, Dey A et al (2023) Marine bioactive compounds as antibiofilm agent: a metabolomic approach. Arch Microbiol 205:54. https://doi.org/10.1007/s00203-022-03391-x
Bayona LM, de Voogd NJ, Choi YH (2022) Metabolomics on the study of marine organisms. Metabolomics 18:17. https://doi.org/10.1007/s11306-022-01874-y
Young RJ, Flitsch SL, Grigalunas M et al (2022) The time and place for nature in drug discovery. JACS Au 2:2400–2416. https://doi.org/10.1021/jacsau.2c00415
Xu Y, Li X, Yao H, Lin K (2019) Neural networks in drug discovery: current insights from medicinal chemists. Future Med Chem 11:1669–1672. https://doi.org/10.4155/fmc-2019-0118
Haney EF, Brito-Sánchez Y, Trimble MJ et al (2018) Computer-aided discovery of peptides that specifically attack bacterial biofilms. Sci Rep 8:1871. https://doi.org/10.1038/s41598-018-19669-4
Acknowledgements
The authors gratefully acknowledge Prof. Titik Nuryastuti, M.D., Ph.D, and Prof. Dr. Puspita Lisdiyanti, M.Agr.Chem, from the Indonesian Biofilm Research Collaboration Center for their coordination and extensive support.
Funding
This work was funded by National Research and Innovation Agency through the Expedition and Exploration Funding (No. 2312/II.7/HK.01.00/7/2022) and Research Collaboration Center Research Projects (2/PKR/PPK-DFRI/2022; 1206/UN1/Dit-Lit/PT.01.03/2022) as well as Research Grant for National Collaboration from Faculty of Pharmacy, Gadjah Mada University (No. 63.31.01/UN1/FFA/UP/SK/2023).
Author information
Authors and Affiliations
Contributions
LS conceived the concept of the review, drafted and wrote the original manuscript, and prepared the figures; AA collected information and prepared the table; LS, AA, and TH revised the manuscript; TH supervised the work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sukmarini, L., Atikana, A. & Hertiani, T. Antibiofilm activity of marine microbial natural products: potential peptide- and polyketide-derived molecules from marine microbes toward targeting biofilm-forming pathogens. J Nat Med 78, 1–20 (2024). https://doi.org/10.1007/s11418-023-01754-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-023-01754-2