Abstract
Purpose
Optimal active recovery is 80% of lactate threshold for trained individuals, yet this may differ for untrained individuals. Therefore, our goal was to investigate the lactate response during optimal active recovery for athletes vs. non-athletes.
Methods
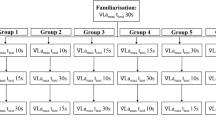
Sixteen adults (21 ± 1 year, BMI: 26.5 ± 3.6 kg·m−2) were enrolled in a cohort study (collegiate athletes vs. non-athletes). Visit one determined participant lactate threshold and VO2max. Visit two consisted of a brief, but intense running protocol followed by active recovery at 80% of lactate threshold. Heart rate and lactate were taken at rest and every four minutes during active recovery. General mixed linear modeling was used (Alpha p < 0.05) and Cohen’s d was calculated for effect size. Post hoc analysis of individual time points used Bonferroni adjustment.
Results
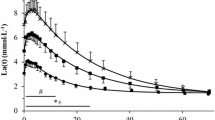
There was a significant difference in overall lactate (β = − 2.34 mmol·L−1·min−1, p < 0.001, d = 2.32) favoring athletes and at each time point during active recovery (all p < 0.005). There was a significant difference in overall heart rate favoring athletes (β = − 14 bpm, p = 0.003, d = 1.64) and individual time points (all p < 0.005).
Conclusion
Lactate removal during active recovery (80% of lactate threshold) demonstrated a significant difference between athletes vs. non-athletes. Optimal intensity of active recovery for non-athletes should be further investigated.


Similar content being viewed by others
References
Buchheit M, Laursen PB (2013) High-intensity interval training, solutions to the programming puzzle: part I: cardiopulmonary emphasis. Sports Med 43(5):313–338
Sloth M, Sloth D, Overgaard K, Dalgas U (2013) Effects of sprint interval training on VO2max and aerobic exercise performance: a systematic review and meta-analysis. Scand J Med Sci Sports 23(6):e341-352
Gist NH, Fedewa MV, Dishman RK, Cureton KJ (2014) Sprint interval training effects on aerobic capacity: a systematic review and meta-analysis. Sports Med 44(2):269–279
Thompson WR (2019) Worldwide survey of fitness trends for 2020. ACSM’s Health Fit J 23(6):10–18
Hood MS, Little JP, Tarnopolsky MA, Myslik F, Gibala MJ (2011) Low-volume interval training improves muscle oxidative capacity in sedentary adults. Med Sci Sports Exerc 43(10):1849–1856
Driller MW, Fell JW, Gregory JR, Shing CM, Williams AD (2009) The effects of high-intensity interval training in well-trained rowers. Int J Sports physiol Perf 4(1):110–121
Garber CE, Blissmer B, Deschenes MR, American College of Sports Medicine position stand et al (2011) Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 43(7):1334–1359
Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB (2002) Exercise type and intensity in relation to coronary heart disease in men. JAMA 288(16):1994–2000
Gillen JB, Percival ME, Skelly LE et al (2014) Three minutes of all-out intermittent exercise per week increases skeletal muscle oxidative capacity and improves cardiometabolic health. PLoS ONE 9(11):e111489
Trost SG, Owen N, Bauman AE, Sallis JF, Brown W (2002) Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc 34(12):1996–2001
Costa Leite T, Da Silva D, Guimarães Coelho R, Zancan P, Sola-Penna M (2007) Lactate favours the dissociation of skeletal muscle 6-phosphofructo-1-kinase tetramers down-regulating the enzyme and muscle glycolysis. Biochem J 408(1):123–130
Stackhouse SK, Reisman DS, Binder-Macleod SA (2001) Challenging the role of pH in skeletal muscle fatigue. Phys Ther 81(12):1897–1903
Weltman A, Stamford BA, Moffatt RJ, Katch VL (1977) Exercise recovery, lactate removal, and subsequent high intensity exercise performance. Res Q 48(4):786–796
Menzies P, Menzies C, McIntyre L, Paterson P, Wilson J, Kemi OJ (2010) Blood lactate clearance during active recovery after an intense running bout depends on the intensity of the active recovery. J sports Sci 28(9):975–982
Franchini E, Yuri Takito M, Yuzo Nakamura F, Ayumi Matsushigue K, Peduti Dal Molin Kiss M (2003) Effects of recovery type after a judo combat on blood lactate removal and on performance in an intermittent anaerobic task. J Sports Med Phys fit. 43(4):424–431
Mota MR, Dantas RAE, Oliveira-Silva I et al (2017) Effect of self-paced active recovery and passive recovery on blood lactate removal following a 200 m freestyle swimming trial. Open Access J Sports Med 8:155
Monedero J, Donne B (2000) Effect of recovery interventions on lactate removal and subsequent performance. Int J Sports Med 21(08):593–597
Tomschi F, Bizjak DA, Predel H-G, Bloch W, Grau M (2018) Lactate distribution in red blood cells and plasma after a high intensity running exercise in aerobically trained and untrained subjects. J Hum Sport Exerc 13(2):384–392
Sumida KD, Urdiales JH, Donovan CM (1993) Enhanced gluconeogenesis from lactate in perfused livers after endurance training. J Appl Physiol 74(2):782–787
ACSM (2017) ACSM’s guidelines for exercise testing and prescription, 10th edn. Wolters Kluwer, Alphen aan den Rijn
Hart S, Drevets K, Alford M, Salacinski A, Hunt BE (2013) A method-comparison study regarding the validity and reliability of the Lactate Plus analyzer. BMJ Open. 3(2):e001899
Bruce RA, Kusumi F, Hosmer D (1973) Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J 85(4):546–562
Davis JA, Rozenek R, DeCicco DM, Carizzi MT, Pham PH (2007) Comparison of three methods for detection of the lactate threshold. Clin Physiol Funct Imaging 27(6):381–384
Faude O, Kindermann W, Meyer T (2009) Lactate threshold concepts. Sports Med 39:469–490
Sahlin K, Alvestrand A, Brandt R, Hultman E (1978) Intracellular pH and bicarbonate concentration in human muscle during recovery from exercise. J Appl Physiol Respir Environ Exerc Physiol 45(3):474–480
Tschakert G, Hofmann P (2013) High-intensity intermittent exercise: methodological and physiological aspects. Int J Sports Physiol Perform 8(6):600–610
Sahlin K (1992) Metabolic factors in fatigue. Sports Med (Auckland, NZ) 13(2):99–107
Gladden LB (2000) Muscle as a consumer of lactate. Med Sci Sports Exerc 32(4):764–771
Gladden L (2004) Lactate metabolism: a new paradigm for the third millennium. J Physiol 558(1):5–30
Armstrong LE, Johnson EC. Water Intake, Water Balance, and the Elusive Daily Water Requirement. Nutrients. 2018;10(12).
Sheriff DD (2010) Role of mechanical factors in governing muscle blood flow. Acta physiol 199(4):385–391
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethics approval
The study procedures were approved by Texas A&M University-Kingsville IRB (2019-030/12306) and was conducted according to the Declaration of Helsinki.
Informed consent
All subjects provided written consent before participation after all procedures had been clearly explained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hinojosa, J.N., Hearon, C.M. & Kowalsky, R.J. Blood lactate response to active recovery in athletes vs. non-athletes. Sport Sci Health 17, 699–705 (2021). https://doi.org/10.1007/s11332-021-00735-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-021-00735-w