Abstract
Background/objective
Obstructive sleep apnea (OSA) is characterized by complete or partial cessation of breathing during sleep. The tongue is suggested as a possible anatomical site causing airway obstruction. However, the role of other pharyngeal structures in the development of OSA remains unclear. We designed a study using both the apnea–hypopnea index (AHI) and the oxygen saturation measurements to assess the severity of OSA. We aimed to identify critical anatomical structures of the upper airway that correlate with the severity of OSA and to evaluate the utility of magnetic resonance imaging (MRI) markers to detect possible OSA in patients without overt symptoms.
Materials and methods
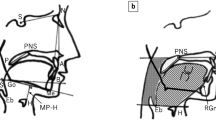
The study included participants referred to the neurology outpatient clinic from the check-up unit. Participants were grouped as controls, mild, moderate, or severe OSA according to the AHI. A cranial MRI with a field of view (FOV) encompassing the upper airway structures was obtained from all participants. The areas of the tongue and the uvula were measured on the sagittal images by drawing the boundaries of the tissues manually. The posterior air space (PAS) area was evaluated from regions of interest in five parallel planes.
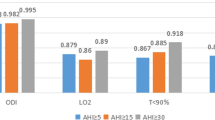
Results
Of 105 participants, 30 were controls, 27 had mild, 25 had moderate, and 23 had severe OSA. The moderate and severe OSA groups did not differ in oxygen saturation levels during sleep. Therefore, patients with moderate and severe OSA were combined into one group (moderate/severe OSA). The area of the tongue was significantly larger in the moderate/severe OSA group compared to the control group. Both the tongue and the uvula areas showed a significant positive correlation with the AHI.
Conclusion
Our findings suggest that the tongue and uvula have prominent roles in the severity of OSAS. It may be useful to measure these structures with MRI to screen for at-risk individuals without overt OSA symptoms.





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
McNicholas WT (2002) Public health and medicolegal implications of sleep apnoea. Eur Respir J 20:1594–1609. https://doi.org/10.1183/09031936.02.00404502
Mortimore IL, Marshall I, Wraith PK et al (1998) Neck and total body fat deposition in nonobese and obese patients with sleep apnea compared with that in control subjects. Am J Respir Crit Care Med 157:280–283. https://doi.org/10.1164/ajrccm.157.1.9703018
Malhotra A, Huang Y, Fogel RB et al (2002) The male predisposition to pharyngeal collapse: importance of airway length. Am J Respir Crit Care Med 166:1388–1395. https://doi.org/10.1164/rccm.2112072
Shelton KE, Woodson H, Gay S et al (1993) Pharyngeal fat in obstructive sleep apnea. Am Rev Respir Dis 148:462–466. https://doi.org/10.1164/ajrccm/148.2.462
Shelton KE, Gay SB, Hollowell DE et al (1993) Mandible enclosure of upper airway and weight in obstructive sleep apnea. Am Rev Respir Dis 148:195. https://doi.org/10.1164/ajrccm/148.1.195
Trudo FJ, Gefter WB, Welch KC et al (1998) State-related changes in upper airway caliber and surrounding soft-tissue structures in normal subjects. Am J Respir Crit Care Med 158:1259–1270. https://doi.org/10.1164/ajrccm.158.4.9712063
Whittle AT, Marshall I, Mortimore IL et al (1999) Neck soft tissue and fat distribution: comparison between normal men and women by magnetic resonance imaging. Thorax 54:323–8. https://doi.org/10.1136/thx.54.4.323
Ryan CF, Lowe AA, Li D et al (1991) Three-dimensional upper airway computed tomography in obstructive sleep apnea. Am Rev Respir Dis 144:428–432. https://doi.org/10.1164/ajrccm/144.2.428
Lowe AA, Gionhaku N, Takeuchi K et al (1986) Three-dimensional CT reconstructions of tongue and airway in adult subjects with obstructive sleep apnea. Am J Orthod Dentofac Orthop 90:364–374. https://doi.org/10.1016/0889-5406(86)90002-8
Schwab RJ, Pasirstein M, Pierson R et al (2003) Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med 168:522–530. https://doi.org/10.1164/rccm.200208-866OC
Arens R, McDonough JM, Corbin AM et al (2002) Linear dimensions of the upper airway structure during development: assessment by magnetic resonance imaging. Am J Respir Crit Care Med 165:117–122. https://doi.org/10.1164/ajrccm.165.1.2107140
Arens R, McDonough JM, Costarino AT et al (2001) Magnetic resonance imaging of the upper airway structure of children with obstructive sleep apnea syndrome. Am J Respir Crit Care Med 164:698–703. https://doi.org/10.1164/ajrccm.164.4.2101127
Welch KC, Foster GD, Ritter CT et al (2002) A novel volumetric magnetic resonance imaging paradigm to study upper airway anatomy. Sleep 25:530–540. https://doi.org/10.1093/sleep/25.5.530
Barrera JE, Pau CY, Forest V et al (2017) Anatomic measures of upper airway structures in obstructive sleep apnea. World J Otorhinolaryngol - Head Neck Surg 3:85–91. https://doi.org/10.1016/j.wjorl.2017.05.002
Ciscar MA, Juan M, Martinez V et al (2001) Magnetic resonance imaging of the pharynx in OSA patients and healthy subjects. Eur Respir J 17:79–86. https://doi.org/10.1183/09031936.01.17100790
Rodenstein DO, Dooms G, Thomas Y et al (1990) Pharyngeal shape and dimensions in healthy subjects, snorers, and patients with obstructive sleep apnoea. Thorax 45:722–7. https://doi.org/10.1136/thx.45.10.722
Schwab RJ, Gubta KB, Gefter WB et al (1995) Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med 152:1673–1689. https://doi.org/10.1164/ajrccm.152.5.7582313
Barbé F, Amilibia J, Capote F (1995) Diagnóstico del síndrome de apneas obstructivas durante el sueño. Informe de consenso del área de insuficiencia respiratoria y trastornos del sueño. Arch Bronconeumol 31:460–462. https://doi.org/10.1016/S0300-2896(15)30866-8
Browman CP, Sampson MG, Yolles SF et al (1984) Obstructive sleep apnea and body weight. Chest 85:435–436. https://doi.org/10.1378/chest.85.3.435
Berry RB, Brooks R, Gamaldo CE et al (2015) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications : version 2.3. American Academy of Sleep Medicine
Temirbekov D, Gunes S, Yazici MZ et al (2018) The ignored parameter in the diagnosis of obstructive sleep apnea syndrome: the oxygen desaturation index. Turk Arch Otorhinolaryngol 56:1–6. https://doi.org/10.5152/tao.2018.3025
Chung F, Liao P, Elsaid H et al (2012) Oxygen desaturation index from nocturnal oximetry: a sensitive and specific tool to detect sleep-disordered breathing in surgical patients. Anesth Analg 114:993–1000
Martinez-Garcia MA, Sanchez de-la Torre M, White DP et al (2023) Hypoxic burden in obstructive sleep apnea: present and future. Archivos deBronconeumologia 59:36–43. https://doi.org/10.1016/j.arbres.2022.08.005
Azarbarzin A, Sands SA, Stone KL et al (2019) The hypoxic burden of sleep apnoea predicted cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study. Eur Heart J 40:1149–1157
Gupta A, Shukla G (2018) Obstructive sleep apnea and stroke. J Clin Sleep Med 14(10):1819. https://doi.org/10.5664/jcsm.7416
Guay-Gagnon M, Vat S, Forget MF et al (2022) Sleep apnea and the risk of dementia: a systematic review and meta-analysis. J Sleep Res 31(5):e13589. https://doi.org/10.1111/jsr.13589
Tavsanli ME (2022) Comorbidity analysis in obstructive sleep apnea patients. Annal Med Res 29(9):957–961
Bonsignore MR, Baiamonte P, Mazzuca E et al (2019) Obstructive sleep apnea and comorbidities: a dangerous liaison. Multidiscip Respir Med 14:1–12
White DP (2006) Sleep apnea. Proc Am Thorac Soc 3:124–128. https://doi.org/10.1513/pats.200510-116JH
Nashi N, Kang S, Barkdull GC et al (2007) Lingual fat at autopsy. Laryngoscope 117:1467–1473. https://doi.org/10.1097/MLG.0b013e318068b566
Humbert IA, Reeder SB, Porcaro EJ et al (2008) Simultaneous estimation of tongue volume and fat fraction using IDEAL-FSE. J Magn Reson Imaging An Off J Int Soc Magn Reson Med 28:504–508. https://doi.org/10.1002/jmri.21431
Kim AM, Keenan BT, Jackson N et al (2014) Tongue fat and its relationship to obstructive sleep apnea. Sleep 37:1639–1648. https://doi.org/10.5665/sleep.4072
Sforza E, Roche F (2016) Chronic intermittent hypoxia and obstructive sleep apnea: an experimental and clinical approach. Hypoxia 4:99–108. https://doi.org/10.2147/hp.s103091
Mortimore IL, Marshall I, Wraith PK et al (1998) Neck and total body fat deposition in nonobese and obese patients with sleep apnea compared with that in control subjects. Am J Respir Crit Care Med 157(1):280–283. https://doi.org/10.1164/ajrccm.157.1.9703018
Gray EL, McKenzie DK, Eckert DJ (2017) Obstructive sleep apnea without obesity ıs common and difficult to treat: evidence for a distinct pathophysiological phenotype. J Clin Sleep Med 13(1):81–8. https://doi.org/10.5664/jcsm.6394
Wellman A, Eckert DJ, Jordan AS et al (2011) A method for measuring and modeling the physiological traits causing obstructive sleep apnea. J Appl Physiol 110:1627–1637. https://doi.org/10.1152/japplphysiol.00972.2010
Younes M, Ostrowski M, Atkar R et al (2007) Mechanisms of breathing instability in patients with obstructive sleep apnea. J Appl Physiol 103:1929–1941. https://doi.org/10.1152/japplphysiol.00561.2007
White DP (2005) Pathogenesis of obstructive and central sleep apnea. Am J Respir Crit Care Med 172:1363–1370. https://doi.org/10.1164/rccm.200412-1631SO
Malhotra A, White DP (2002) Obstructive sleep apnoea. Lancet 360:237–245. https://doi.org/10.1016/S0140-6736(02)09464-3
Eckert DJ, Malhotra A (2008) Pathophysiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5:144–153. https://doi.org/10.1513/pats.200707-114MG
Longobardo GS, Evangelisti CJ, Cherniack NS (2009) Influence of arousal threshold and depth of sleep on respiratory stability in man: analysis using a mathematical model. Exp Physiol 94(12):1185–1199
Liégeois F, Albert A, Limme M (2010) Comparison between tongue volume from magnetic resonance images and tongue area from profile cephalograms. Eur J Orthod 32(4):381–386. https://doi.org/10.1093/ejo/cjp105
Acknowledgements
We would like to thank Murat Aksu for his contributions to the editing of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection were performed by MET and AZ, and analysis was performed by MET and MS. The first draft of the manuscript was written by MET, MS, and AZ, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee (Acibadem Mehmet Ali Aydinlar University Ethical Committee) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tavsanli, M.E., Zeynalova, A. & Seckin, M. The effect of pharyngeal structures on the severity of obstructive sleep apnea. Sleep Breath (2023). https://doi.org/10.1007/s11325-023-02973-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11325-023-02973-3