Abstract
Purpose
The objective was to determine if alteration in airflow induced by negative pressure (NP) applied to participants’ upper airways during wakefulness, is related to obstructive sleep apnea (OSA) severity as determined by the apnea–hypopnea index (AHI).
Methods
Adults 18 years of age or greater were recruited. All participants underwent overnight polysomnography to assess their apnea–hypopnea index (AHI). While awake, participants were twice exposed, orally, to -3 cm H2O of NP for five full breaths. The ratio of the breathing volumes of the last two breaths during NP exposure to the last two breaths prior to NP exposure was deemed the NP ratio (NPR).
Results
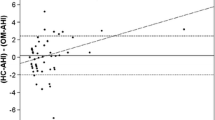
Eighteen participants were enrolled. A strong relationship between the AHI and the exponentially transformed NPR (ExpNPR) for all participants was observed (R2 = 0.55, p < 0.001). A multivariable model using the independent variable ExpNPR, age, body mass index and sex accounted for 81% of variability in AHI (p = 0.0006). A leave-one-subject-out cross-validation analysis revealed that predicted AHI using the multivariable model, and actual AHI from participants’ polysomnograms, were strongly related (R2 = 0.72, p < 0.001).
Conclusion
We conclude that ExpNPR, was strongly related to the AHI, independently of demographic factors known to be related to the AHI.




Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Eckert DJ, Malhotra A (2008) Pathophysiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5:144–153. https://doi.org/10.1513/pats.200707-114MG
Heinzer R, Vat S, Marques-Vidal P et al (2015) Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 3:310–318. https://doi.org/10.1016/s2213-2600(15)00043-0
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177:1006–1014. https://doi.org/10.1093/aje/kws342
Young T, Evans L, Finn L, Palta M (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 20:705–706. https://doi.org/10.1093/sleep/20.9.705
Kee K, Dixon J, Shaw J et al (2018) Comparison of Commonly Used Questionnaires to Identify Obstructive Sleep Apnea in a High-Risk Population. J Clin Sleep Med 14:2057–2064. https://doi.org/10.5664/jcsm.7536
Pini L, Magri R, Perger E et al (2022) Phenotyping OSAH patients during wakefulness. Sleep Breathing 26:1801–1807. https://doi.org/10.1007/s11325-021-02551-5
Romano S, Salvaggio A, Hirata RP, Lo Bue A, Picciolo S, Oliveira LV, Insalaco G (2011) Upper airway collapsibility evaluated by a negative expiratory pressure test in severe obstructive sleep apnea. Clinics (Sao Paulo) 66:567–572. https://doi.org/10.1590/s1807-59322011000400008
Brown IG, Bradley TD, Phillipson EA, Zamel N, Hoffstein V (1985) Pharyngeal compliance in snoring subjects with and without obstructive sleep apnea. Am Rev Respir Dis 132:211–215. https://doi.org/10.1164/arrd.1985.132.2.211
Gleadhill IC, Schwartz AR, Schubert N, Wise RA, Permutt S, Smith PL (1991) Upper airway collapsibility in snorers and in patients with obstructive hypopnea and apnea. Am Rev Respir Dis 143:1300–1303. https://doi.org/10.1164/ajrccm/143.6.1300
Haponik EF, Smith PL, Bohlman ME, Allen RP, Goldman SM, Bleecker ER (1983) Computerized tomography in obstructive sleep apnea. Correlation of airway size with physiology during sleep and wakefulness. Am Rev Respir Dis 127:221–226. https://doi.org/10.1164/arrd.1983.127.2.221
Isono S, Remmers JE, Tanaka A, Sho Y, Sato J (1985) Nishino T (1997) Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J Appl Physiol 82:1319–1326. https://doi.org/10.1152/jappl.1997.82.4.1319
Ferretti A, Giampiccolo P, Redolfi S, Mondini S, Cirignotta F, Cavalli A, Tantucci C (2006) Upper airway dynamics during negative expiratory pressure in apneic and non-apneic awake snorers. Respir Res 7:54
Hirata RP, Schorr F, Kayamori F et al (2016) Upper Airway Collapsibility Assessed by Negative Expiratory Pressure while Awake is Associated with Upper Airway Anatomy. J Clin Sleep Med 12:1339–1346. https://doi.org/10.5664/jcsm.6184
Liistro G, Veriter C, Dury M, Aubert G, Stanescu D (1999) Expiratory flow limitation in awake sleep-disordered breathing subjects. Eur Respir J 14:185–190. https://doi.org/10.1034/j.1399-3003.1999.14a31.x
Montemurro LT, Bettinzoli M, Corda L, Braghini A, Tantucci C (2010) Relationship between critical pressure and volume exhaled during negative pressure in awake subjects with sleep-disordered breathing. Chest 137:1304–1309. https://doi.org/10.1378/chest.09-2109
Baydur A, Vigen C, Chen Z (2012) Expiratory Flow Limitation in Obstructive Sleep Apnea and COPD: A Quantitative Method to Detect Pattern Differences Using the Negative Expiratory Pressure Technique. Open Respir Med J 6:111–120. https://doi.org/10.2174/1874306401206010111
Guillot M, Costes F, Sforza E, Maudoux D, Bertoletti L, Barthelemy JC, Roche F (2010) Is tidal expiratory flow limitation predictive of sleep-related disorders in the elderly? Eur Respir J 36:842–848. https://doi.org/10.1183/09031936.00078009
Insalaco G, Romano S, Marrone O, Salvaggio A, Bonsignore G (2005) A new method of negative expiratory pressure test analysis detecting upper airway flow limitation to reveal obstructive sleep apnea. Chest 128:2159–2165. https://doi.org/10.1378/chest.128.4.2159
Rouatbi S, Tabka Z, Dogui M, Abdelghani A, Guenard H (2009) Negative expiratory pressure (NEP) parameters can predict obstructive sleep apnea syndrome in snoring patients. Lung 187:23–28. https://doi.org/10.1007/s00408-008-9122-6
Schwartz AR, Smith PL, Wise RA, Gold AR (1985) Permutt S (1988) Induction of upper airway occlusion in sleeping individuals with subatmospheric nasal pressure. J Appl Physiol 64:535–542. https://doi.org/10.1152/jappl.1988.64.2.535
Smith PL, Wise RA, Gold AR, Schwartz AR, Permutt S (1988) Upper airway pressure-flow relationships in obstructive sleep apnea. J Appl Physiol 64:789–795. https://doi.org/10.1152/jappl.1988.64.2.789
Berry RB, Budhiraja R, Gottlieb DJ et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619. https://doi.org/10.5664/jcsm.2172
Mendelson M, Lyons OD, Yadollahi A, Inami T, Oh P, Bradley TD (2016) Effects of exercise training on sleep apnoea in patients with coronary artery disease: a randomised trial. Eur Respir J 48:142–150. https://doi.org/10.1183/13993003.01897-2015
Young T, Skatrud J, Peppard PE (2004) Risk factors for obstructive sleep apnea in adults. JAMA 291:2013–2016. https://doi.org/10.1001/jama.291.16.2013
Chowdhury MZI, Turin TC (2020) Variable selection strategies and its importance in clinical prediction modelling. Fam Med Community Health 8:262. https://doi.org/10.1136/fmch-2019-000262
Verin E, Tardif C, Portier F, Similowski T, Pasquis P, Muir JF (2002) Evidence for expiratory flow limitation of extrathoracic origin in patients with obstructive sleep apnoea. Thorax 57:423–428. https://doi.org/10.1136/thorax.57.5.423
Gold AR, Marcus CL, Dipalo F, Gold MS (2002) Upper airway collapsibility during sleep in upper airway resistance syndrome. Chest 121:1531–1540. https://doi.org/10.1378/chest.121.5.1531
Malhotra A, Pillar G, Fogel R, Beauregard J, Edwards J, White DP (2001) Upper-airway collapsibility: measurements and sleep effects. Chest 120:156–161. https://doi.org/10.1378/chest.120.1.156
Sanders MH, Moore SE (1983) Inspiratory and expiratory partitioning of airway resistance during sleep in patients with sleep apnea. Am Rev Respir Dis 127:554–558. https://doi.org/10.1164/arrd.1983.127.5.554
Schneider H, Boudewyns A, Smith PL et al (1985) (2002) Modulation of upper airway collapsibility during sleep: influence of respiratory phase and flow regimen. J Appl Physiol 93:1365–1376. https://doi.org/10.1152/japplphysiol.00942.2001
Morrell MJ (1985) Badr MS (1998) Effects of NREM sleep on dynamic within-breath changes in upper airway patency in humans. J Appl Physiol 84:190–199. https://doi.org/10.1152/jappl.1998.84.1.190
Schwab RJ, Gefter WB, Hoffman EA, Gupta KB, Pack AI (1993) Dynamic upper airway imaging during awake respiration in normal subjects and patients with sleep disordered breathing. Am Rev Respir Dis 148:1385–1400. https://doi.org/10.1164/ajrccm/148.5.1385
Remmers JE, deGroot WJ, Sauerland EK, Anch AM (1978) Pathogenesis of upper airway occlusion during sleep. J Appl Physiol Respir Environ Exerc Physiol 44:931–938. https://doi.org/10.1152/jappl.1978.44.6.931
Suratt PM, Wilhoit SC, Cooper K (1984) Induction of airway collapse with subatmospheric pressure in awake patients with sleep apnea. J Appl Physiol Respir Environ Exerc Physiol 57:140–146. https://doi.org/10.1152/jappl.1984.57.1.140
Tantucci C, Mehiri S, Duguet A et al (1998) Application of negative expiratory pressure during expiration and activity of genioglossus in humans. J Appl Physiol 84:1076–1082. https://doi.org/10.1152/jappl.1998.84.3.1076
Fogel RB, Malhotra A, Pillar G, Edwards JK, Beauregard J, Shea SA, White DP (2001) Genioglossal activation in patients with obstructive sleep apnea versus control subjects. Mechanisms of muscle control. Am J Respir Crit Care Med 164:2025–2030. https://doi.org/10.1164/ajrccm.164.11.2102048
Basner RC, Ringler J, Schwartzstein RM, Weinberger SE, Weiss JW (1991) Phasic electromyographic activity of the genioglossus increases in normals during slow-wave sleep. Respir Physiol 83:189–200. https://doi.org/10.1016/0034-5687(91)90028-h
Trinder J, Whitworth F, Kay A (1985) Wilkin P (1992) Respiratory instability during sleep onset. J Appl Physiol 73:2462–2469. https://doi.org/10.1152/jappl.1992.73.6.2462
Findley LJ, Wilhoit SC, Suratt PM (1985) Apnea duration and hypoxemia during REM sleep in patients with obstructive sleep apnea. Chest 87:432–436. https://doi.org/10.1378/chest.87.4.432
Bouloukaki I, Kapsimalis F, Mermigkis C et al (2011) Prediction of obstructive sleep apnea syndrome in a large Greek population. Sleep Breath 15:657–664. https://doi.org/10.1007/s11325-010-0416-6
Deegan PC, McNicholas WT (1996) Predictive value of clinical features for the obstructive sleep apnoea syndrome. Eur Respir J 9:117–124. https://doi.org/10.1183/09031936.96.09010117
Santaolalla Montoya F, Iriondo Bedialauneta JR, Aguirre Larracoechea U, Martinez Ibargüen A, Sanchez Del Rey A, Sanchez Fernandez JM (2007) The predictive value of clinical and epidemiological parameters in the identification of patients with obstructive sleep apnoea (OSA): a clinical prediction algorithm in the evaluation of OSA. Eur Arch Otorhinolaryngol 264:637–643. https://doi.org/10.1007/s00405-006-0241-5
Hoffstein V, Szalai JP (1993) Predictive value of clinical features in diagnosing obstructive sleep apnea. Sleep 16:118–122
Acknowledgements
This work was supported by a grant from the Ontario Lung Association.
T.D. Bradley was supported by the Godfrey S. Pettit Chair in Respiratory Medicine.
Funding
The Ontario Lung Association provided financial support in the form of grant funding. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional ethics board of the University Health Network and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers' bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lim, J., Alshaer, H., Ghahjaverestan, N.M. et al. Relationship between airflow limitation in response to upper airway negative pressure during wakefulness and obstructive sleep apnea severity. Sleep Breath 28, 231–239 (2024). https://doi.org/10.1007/s11325-023-02892-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02892-3