Abstract
Purpose
The pathogenesis of obstructive sleep apnea (OSA) is complex and may vary between different races. It has been suggested that the anatomical balance between skeletal tissues and soft tissues around the upper airway is a key pathophysiologic factor of OSA. Therefore, the aim of this study was to compare the anatomical balance of the upper airway between Dutch and Chinese patients with OSA based on cone beam computed tomography (CBCT) images.
Methods
This was a cross-sectional study performed in two centers and included Dutch and Chinese adults with OSA. CBCT scans in the supine position were obtained for both Dutch and Chinese OSA groups. The primary outcome variable was the anatomical balance of the upper airway, defined as the ratio of the tongue area and the maxillomandibular enclosure area.
Results
A total of 28 Dutch adults (mean age ± SD of 46.6 ± 14.1 years, body mass index [BMI] of 26.8 ± 3.5 kg/m2, and apnea-hypopnea index [AHI] of 15.7 ± 7.1 events/h) and 24 Chinese adults (age 41.0 ± 12.4 years, BMI 26.5 ± 3.3 kg/m2, and AHI 16.5 ± 7.8 events/h). There were no significant differences in AHI, age, BMI, and sex between the two groups (P = 0.14–0.76). The Dutch group had a significantly larger tongue area and tongue length compared to the Chinese group (P = 0.01 and P < 0.01). On the other hand, the Chinese group had a smaller maxilla length compared to the Dutch group (P < 0.01). However, the anatomical balance of the upper airway of both groups was not significantly different (P = 0.16).
Conclusion
Within the limitations of this study, no significant difference was found in the anatomical balance of the upper airway between Dutch and Chinese patients with mild to moderate OSA.
Trial registration
The present study was registered at the ClinicalTrials.gov identifier NCT03463785.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is characterized by recurrent complete and/or partial obstructions of the upper airway, often resulting in arousals from sleep and oxygen desaturations [1]. Excessive daytime sleepiness, lack of concentration, and fatigue are examples of frequent complaints of patients with OSA [2]. The pathogenesis of OSA involves a complex interaction of anatomical and non-anatomical factors, among which a narrowed upper airway plays a key role [3]. It has been suggested that the pathogenesis of OSA may vary between different races; however, the exact difference is still unclear [4, 5].
Both restricted skeletal structures and enlarged soft tissues can lead to a narrowed upper airway [6, 7]. Specifically, the anatomical balance of the upper airway, defined as the ratio of the tongue size and the maxillomandibular enclosure size, is a key determinant of upper airway morphology [8]. Studies have indicated that, when the OSA severity is similar, Caucasian adults with OSA are more overweight (e.g., greater body mass index (BMI) and neck circumference), whereas Asian adults with OSA show more severe skeletal restrictions (e.g., a smaller maxilla and mandible, and retrognathia) [9-12]. These findings indicate that the anatomical balance of the upper airway may be similar between the two races.
Only a few studies have performed a direct inter-race comparison of the anatomical balance. However, their results are inclusive. A study of Schorr et al. [11] has suggested that Caucasians with OSA had a greater anatomical imbalance as compared with the Japanese-Brazilians with OSA. On the other hand, the study of Lee et al. [10] has suggested a similar anatomical balance between Caucasian and Chinese patients with OSA. The different results could be due to different races being compared. Besides, their results may be biased by using an inaccurate definition of the anatomical balance. Since the anatomical balance is involved in the pathogenesis of OSA [8, 13], and is also an important predictor of treatment outcome of OSA [14], a better understanding of the role of anatomical balance between different races is necessary. This may help to improve OSA recognition and result in a more targeted therapy for specific racial groups.
According to the current evidence, we hypothesized that the anatomical balance of the upper airway (i.e., the ratio of the tongue area and the maxillomandibular enclosure area) is similar between Dutch and Chinese patients with OSA. To investigate upper airway morphology, cone beam computed tomography (CBCT) has been suggested to be a reliable technique [15, 16] with lower radiation dose and costs compared to traditional CT [17, 18]. Therefore, the aim of this study was to compare the anatomical balance of the upper airway between Dutch and Chinese patients based on CBCT images.
Material and methods
Overview
This was cross-sectional study in which participants were recruited from both the Amsterdam University Medical Center (AUMC) in the Netherlands and the Qilu Hospital of Shandong University in China. Dutch participants were recruited from a randomized controlled trial (RCT) (ClinicalTrials.gov identifier: NCT02724865), which was designed to compare the treatment effects of two different types of mandibular advancement device (MAD) in patients with mild and moderate OSA. Chinese participants were recruited prospectively for this study.
The protocol for recruiting the patients from the Netherlands was approved by the Medical Ethics Committee of the AUMC with reference number NL44085.018.13/COSH. The protocol of recruiting patients from China was approved by the Medical Ethics Committee of the Dental School of Shandong University with reference number NO.GR201814.
Written informed consent was obtained from both Dutch and Chinese patients. The present study was registered at the ClinicalTrials.gov identifier NCT03463785.
Recruitment
Patients that fit the following inclusion/exclusion criteria were recruited in both the Netherlands and China. The inclusion criteria were as follows: (1) age ≥ 18 years; (2) able to speak, read, and write either Dutch or Chinese; (3) able to follow up; (4) diagnosed with symptomatic mild or moderate OSA (5 ≤ apnea-hypopnea index (AHI) < 30); and (5) expected to be able to maintain their current lifestyle (sports, medicine, diet, etc.).
The exclusion criteria were as follows: (1) medication use related to sleeping disorders; (2) evidence of respiratory and/or sleep disorders other than OSA (e.g., central sleep apnea syndrome); (3) systemic disorders (based on medical history and examination, e.g., rheumatoid arthritis); (4) medical history of known daytime fatigue or severe sleep disturbance (e.g., insomnia, PLMS, narcolepsy); (5) known medical history of mental retardation, memory impairment, or psychiatric disorders; (6) reversible morphological upper airway abnormalities (viz., indication for upper airway surgery); (7) syndromes with craniofacial abnormalities (e.g., Pierre Robin sequence and Down syndrome); and (8) inability to provide informed consent. As the Dutch OSA group was recruited from an RCT study, there were two extra exclusion criteria for this group: (1). untreated periodontal problems/toothache/lack of retention possibilities for an MAD, and (2). concomitant use of other modalities to treat OSA.
Polysomnography (PSG)
All Dutch participants included in this study underwent an overnight PSG recording (Embla A10, Broomfield, CO, USA) at one of the four participating sleep centers (Onze Lieve Vrouwe Gasthuis Ziekenhuis (OLVG), Nederlands Slaap Instituut, Medisch Centrum Jan van Goyen, and Amsterdam Medical Center) in Amsterdam for the diagnosis of OSA. All Chinese participants included in this study underwent an overnight PSG recording (Alice 6, Phillips Respironics, USA) at the Qilu Hospital in Jinan for the diagnosis of OSA.
PSG included the following variables: electroencephalogram, electrooculogram, leg and chin electromyograms, electrocardiogram, pulse oximetry, body position, neck microphone, nasal cannula pressure transducer, and inductive plethysmography by means of thoracic and abdominal bands. The PSG recordings were manually scored in a standard manner for both Dutch and Chinese OSA groups [19]. Apnea was defined as a cessation of airflow of ≥ 90% for at least 10 s. Hypopnea was defined as a decrease in airflow of more than 30% for at least 10 s, accompanied by either ≥ 3% oxygen desaturation or an arousal [19]. The apnea-hypopnea index (AHI) was defined as the number of apneas and hypopneas per hour of sleep.
Cone beam computed tomography (CBCT)
The CBCT datasets of Dutch and Chinese patients were obtained using identical NewTom 5G CBCT systems (QR systems, Verona, Italy), according to a standard imaging protocol [15]. In the Netherlands, CBCT scans of the patients were made at the Department of Oral Radiology at the Academic Centre for Dentistry Amsterdam (ACTA). In China, CBCT scans of the patients were made at the Department of Oral Radiology, School of Dentistry, Shandong University.
During the imaging procedure, automatic exposure control was applied, and the patients were positioned in a supine position with the Frankfort horizontal (FH) plane being perpendicular to the floor [15]. They were instructed to maintain light contact between the molars in natural occlusion, to keep quiet breathing, and to avoid swallowing and other movements during the scanning period. The exposure settings were 110 kV, 4 mA, 0.3 mm voxel size, 3.6 s exposure time (pulsed radiation), and 18–36 s scanning time, depending on the size of the patient [15]. To get a standardized head position of each CBCT image, re-orientation was performed by adjusting the palatal plane (the plane crossing anterior nasal spine (ANS)-posterior nasal spine (PNS)) being parallel to the global horizontal plane in the sagittal view, and perpendicular to the global horizontal plane in the axial view [20]. For further analysis, the images were saved as digital imaging and communications in medicine (DICOM) files. All images were presented to the observers in a room with dimmed light.
Primary outcome variable: anatomical balance of the upper airway
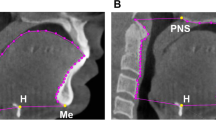
Anatomical balance of the upper airway was calculated using the ratio of the tongue area and the maxillomandibular enclosure area, which were measured on the mid-sagittal plane of CBCT imaging using 3Diagnosys® software (v5.3.1, 3diemme, Cantu, Italy). The tongue area (mm2) was determined by the area enclosed by the point hyoid, menton, the contour of the frontal teeth and the tongue, and the base of the epiglottis (Fig. 1A). The maxillomandibular enclosure area (mm2) was determined by the area enclosed by the point hyoid, menton, the contour of the front teeth, the hard palate, the posterior nasal spine, and the anterior boundary of the second and third cervical vertebra (Fig. 1B).
The values of the anatomical balance range between 0 and 1, and a larger value of the anatomical balance means the tongue occupied a larger section of the maxillomandibular enclosure area compared to a smaller value.
Secondary outcome variables
Secondary outcome variables of the upper airway morphology, including the structures of maxillomandibular enclosure, tongue, soft palate, the maxilla, and the mandible, were measured using 3Diagnosys® software (v5.3.1, 3diemme, Cantu, Italy). The definitions and illustrations of the secondary variables are shown in Table 1 and Fig. 2.
Illustration of the secondary outcome variables of the upper airway morphology (an example from the Dutch group). A Tongue length. B Soft palate length and soft palate thickness. C Maxilla length: distance between ANS (anterior nasal spine) and PNS (posterior nasal spine). D Mandibular length: distance between Go (gonion) and Me (menton)
Statistical analysis
The Shapiro-Wilk test was used to test whether the data were normally distributed. The Mann-Whitney U test (for non-normally distributed variables), the independent t-test (for normally distributed variables), and the chi-squared test (for categorical variables) were used to compare the demographic characteristics, and the primary and secondary outcome variables of the upper airway morphology between the Dutch and Chinese OSA groups. Bonferroni-Holm correction was applied to the comparisons of secondary outcome variables of the upper airway [21]. Statistical analyses were performed using IBM® SPSS® Statistics for Macintosh, Version 26 (IBM Corp., Armonk, NY, USA).
The effect size was calculated for the anatomical balance by the software G*power (version 3.1.9, Franz Faul, Universität Kiel, Germany).
Results
Baseline characteristics
There were 28 Dutch patients and 24 Chinese patients fulfilling the requirements of inclusion and exclusion criteria included in the study. The demographic characteristics of the Dutch and Chinese patients are shown in Table 2. There were no significant differences in age, sex, body mass index (BMI), and apnea-hypopnea index (AHI) between the Dutch and Chinese patients (P = 0.14–0.76).
Comparisons of the upper airway morphology
The variables of the upper airway morphology of the Dutch and Chinese patients are shown in Table 3. The Dutch group had a significantly larger tongue area (T = 2.60, P = 0.01) and a larger tongue length (Z = −3.14, P < 0.01) compared to the Chinese group. On the other hand, the Chinese group had a smaller maxilla length compared to the Dutch group (T = 7.34, P < 0.01). However, the anatomical balance of the upper airway of both groups was not significantly different (T = 1.43, P = 0.16). The effect size d, which is defined as a standardized difference in the means of the anatomical balance of the upper airway between both groups, was 0.4, which can be regarded as between small and medium (the effect size d of 0.20 is small, one of 0.5 is medium, and one of 0.8 is large [22]).
Discussion
The aim of the present study was to compare the anatomical balance of the upper airway between Dutch and Chinese patients with OSA. The results indicated that the Dutch group had a significantly larger tongue area and a larger tongue length compared to the Chinese group, while the Chinese group had a smaller maxilla length compared to the Dutch group. However, the anatomical balance of the upper airway of both groups was not significantly different.
Comparisons of the upper airway morphology
For the primary outcome variable, we did not find a significant difference in the anatomical balance of the upper airway between Dutch and Chinese patients with OSA. Further, the observed effect size d for the difference in the anatomical balance of the upper airway was 0.4, which is between small and medium. With this effect size, the difference in the anatomical balance between both groups may be not clinically relevant either [23, 24]. In contrast to our results, a study of Schorr et al. [11] has suggested that Caucasians with OSA have a larger anatomical imbalance compared with the Japanese-Brazilians with OSA. However, for calculating the anatomical balance, they used the volume of the bony tissue rather than the volume of the bony enclosure as the denominator, which may cause bias and explain the different results as compared to our results. A study of Lee et al. [10] has suggested a similar anatomical balance between Caucasian and Chinese OSA groups, which is similar to our results. However, they used a simplified definition of the anatomical balance, defined as ratios of BMI to mandibular and maxillary bony dimensions, which may be less accurate. The definition used in the present study has been used widely in the literature to investigate the role of the anatomical balance of the upper airway in the pathogenesis and treatment of OSA [13, 14, 25]. Thus, by using a more generalized and accurate definition, the present study confirms that the anatomical balance of the upper airway is similar in Dutch and Chinese OSA groups.
For the secondary outcome variables, the Dutch group had a significantly larger tongue size and larger tongue length compared to the Chinese group. These results are similar to those of previous studies [9-12], which indicates that when the OSA severity is similar, Caucasian patients are more overweight, while Asian patients tend to have a smaller maxilla and mandible.
Previous studies have suggested that the craniofacial skeletal difference between Asians and Caucasians, such as restricted bony structures in Asians, is an important reason for a greater tendency of OSA development in Asians [9, 26]. However, both bony structures and soft tissues can influence the upper airway morphology. By taking into account both factors, the present study indicates that the anatomical imbalance may be similar for both groups. However, in addition to the anatomical factor, several non-anatomical factors are also crucial determinants for upper airway collapse, such as impaired upper airway dilator muscle activity, ventilatory control stability (i.e., high loop gain), and low arousal threshold [27]. The study of Lee et al. [28] has suggested that a low arousal threshold is a less common mechanism in the pathogenesis of the Chinese OSA group compared to the Caucasian OSA group. Further, the study of O’Driscoll et al. [29] has suggested that the loop gain is significantly higher in the Caucasian group than in the Chinese group. However, both studies included moderate-to-severe OSA patients, which may represent a different study sample as compared to our study. To the best of our knowledge, the difference in the non-anatomical factors between both races in patients with mild-to-moderate OSA is not clear yet. Understanding the individual pathogenesis can help in a personalized treatment approach in OSA [27]. Therefore, future research is needed to investigate the roles of anatomical and non-anatomical factors in the pathogenesis of OSA.
Demographic characteristics
Lee et al. [10] have suggested that the referral approach for the clinical assessment of OSA may be influenced by the differences in socioeconomic status, cultural, and environmental factors between the Caucasian and Chinese groups. This is consistent with the phenomenon that we discovered during the recruitment process. There were more patients with severe OSA referred to the sleep laboratory in China than in the Netherlands. To minimize the selection bias, we only recruited patients with mild to moderate OSA in both groups. Besides, both groups were similar in BMI, age, and sex. Therefore, the comparisons of the upper airway morphology between both groups were not biased by these factors.
Clinical relevance
Based on the non-significant results of the present study, it is possible that the anatomical balance of the upper airway plays a similar role in the pathogenesis of OSA in both races. Therefore, it may be speculated that treatment, which mainly targets the anatomical factors, might result in similar treatment results in both groups. Further studies will be performed in our lab to evaluate the treatment effects of therapy in both races.
Limitations
There are several limitations in the present study. First, this study is a multi-center study recruiting Dutch and Chinese patients separately from two sites, which might cause selection bias. However, one of the investigators (H.C.) visited both clinics to make sure that the protocol was implemented in the same way in both the Netherlands and China. Second, in our study, we defined the Dutch and Chinese races of the patients based on their family trees and names, which may cause selection bias. However, the definition of race in the medical literature is not always clear [30]. Contrary to other studies, our definition of race relied on family history rather than on the assumptions of the investigators, which could be a better approach in epidemiological studies [10]. Third, there are 56 ethnic groups in China, and previous studies concluded that the genetic structure is different among different ethnic groups in China [31, 32]. As the craniofacial structure of patients is influenced by genetic factors [33], it is possible that there could be a difference in the craniofacial structure from different ethnic groups in China. In this study, we therefore recruited the Chinese patients only from the Han ethnic group. We excluded the effect of the living environment by recruiting only Dutch patients living in the Netherlands and Chinese patients living in Shandong, China. The measurements of the tongue area and the maxillomandibular enclosure area were based on the mid-sagittal plane of the CBCT imaging, and not on 3D volume measurements. The volume measurements in CBCT images were limited by the difficulty in discriminating between the different soft-tissue structures (due to similar Hounsfield units).
Conclusion
Within the limitations of this study, we conclude that there is no significant difference in the anatomical balance of the upper airway between Dutch and Chinese patients with mild to moderate OSA.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22(5):667–689
Engleman H, Douglas N (2004) Sleep·4: sleepiness, cognitive function, and quality of life in obstructive sleep apnoea/hypopnoea syndrome. Thorax 59(7):618–622
Carberry JC, Amatoury J, Eckert DJ (2018) Personalized management approach for OSA. Chest 153(3):744–755
Sutherland K, Lee RW, Cistulli PA (2012) Obesity and craniofacial structure as risk factors for obstructive sleep apnoea: impact of ethnicity. Respirology 17(2):213–222
Hnin K, Mukherjee S, Antic NA, Catcheside P, Chai-Coetzer CL, McEvoy D, Vakulin A (2018) The impact of ethnicity on the prevalence and severity of obstructive sleep apnea. Sleep Med Rev 41:78–86
Schwab RJ, Pasirstein M, Pierson R, Mackley A, Hachadoorian R, Arens R, Maislin G, Pack AI (2003) Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am J Respir Crit Care Med 168(5):522–530
Neelapu BC, Kharbanda OP, Sardana HK, Balachandran R, Sardana V, Kapoor P, Gupta A, Vasamsetti S (2017) Craniofacial and upper airway morphology in adult obstructive sleep apnea patients: a systematic review and meta-analysis of cephalometric studies. Sleep Med Rev 31:79–90
Watanabe T, Isono S, Tanaka A, Tanzawa H, Nishino T (2002) Contribution of body habitus and craniofacial characteristics to segmental closing pressures of the passive pharynx in patients with sleep-disordered breathing. Am J Respir Crit Care Medic 165(2):260–265
Liu Y, Lowe AA, Zeng X, Fu M, Fleetham JA (2000) Cephalometric comparisons between Chinese and Caucasian patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop 117(4):479–485
Lee RW, Vasudavan S, Hui DS, Prvan T, Petocz P, Darendeliler MA, Cistulli PA (2010) Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep 33(8):1075–1080
Schorr F, Kayamori F, Hirata RP, Danzi-Soares NJ, Gebrim EM, Moriya HT, Malhotra A, Lorenzi-Filho G, Genta PR (2016) Different craniofacial characteristics predict upper airway collapsibility in Japanese-Brazilian and white men. Chest 149(3):737–746
Xu L, Keenan BT, Wiemken AS, Chi L, Staley B, Wang Z, Wang J, Benedikstdottir B, Juliusson S, Pack AI, Gislason T, Schwab RJ (2019) Differences in three-dimensional upper airway anatomy between Asian and European patients with obstructive sleep apnea. Sleep 43(5). https://doi.org/10.1093/sleep/zsz273
Tsuiki S, Isono S, Ishikawa T, Yamashiro Y, Tatsumi K, Nishino T (2008) Anatomical balance of the upper airway and obstructive sleep apnea. Anesthesiology 108(6):1009–1015. https://doi.org/10.1097/ALN.0b013e318173f103
Mostafiz W, Dalci O, Sutherland K, Malhotra A, Srinivasan V, Darendeliler MA, Cistulli PA (2011) Influence of oral and craniofacial dimensions on mandibular advancement splint treatment outcome in patients with obstructive sleep apnea. Chest 139(6):1331–1339
Chen H, Aarab G, Parsa A, de Lange J, van der Stelt PF, Lobbezoo F (2016) Reliability of three-dimensional measurements of the upper airway on cone beam computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol 122(1):104–110
Chen H, Van Eijnatten M, Aarab G, Forouzanfar T, De Lange J, Van Der Stelt P, Lobbezoo F, Wolff J (2018) Accuracy of MDCT and CBCT in three-dimensional evaluation of the oropharynx morphology. Eur J Orthod 40(1):58–64
Palomo JM, Kau CH, Palomo LB, Hans MG (2006) Three-dimensional cone beam computerized tomography in dentistry. Dent Today 25(11):130
Suomalainen A, Kiljunen T, Kaser Y, Peltola J, Kortesniemi M (2009) Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillofac Radiol 38(6):367–378
Berry RB BR, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL et al (2016) The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications, Version 2.3. www.aasmnet.org. Darien Illinois: American Academy of Sleep Medicine
Weissheimer A, Menezes LM, Sameshima GT, Enciso R, Pham J, Grauer D (2012) Imaging software accuracy for 3-dimensional analysis of the upper airway. Am J Orthod Dentofac Orthop 142(6):801–813. https://doi.org/10.1016/j.ajodo.2012.07.015
Armstrong RA (2014) When to use the Bonferroni correction. Ophthalmic Physiol Opt 34(5):502–508. https://doi.org/10.1111/opo.12131
Cohen J (2013) Statistical power analysis for the behavioral sciences. Academic press
Armijo-Olivo S, Warren S, Fuentes J, Magee DJ (2011) Clinical relevance vs. statistical significance: using neck outcomes in patients with temporomandibular disorders as an example. Man Ther 16(6):563–572
Davis SL, Johnson AH, Lynch T, Gray L, Pryor ER, Azuero A, Soistmann HC, Phillips SR, Rice M (2021) Inclusion of effect size measures and clinical relevance in research papers. Nursing Res 70(3):222–230. https://doi.org/10.1097/nnr.0000000000000494
Chen H, Aarab G, Lobbezoo F, De Lange J, Van der Stelt P, Darendeliler MA, Cistulli PA, Sutherland K, Dalci O (2019) Differences in three-dimensional craniofacial anatomy between responders and non-responders to mandibular advancement splint treatment in obstructive sleep apnoea patients. Eur J Orthod 41(3):308–315. https://doi.org/10.1093/ejo/cjy085
Chen X, Wang R, Lutsey PL, Zee PC, Javaheri S, Alcántara C, Jackson CL, Szklo M, Punjabi N, Redline S, Williams MA (2016) Racial/ethnic differences in the associations between obesity measures and severity of sleep-disordered breathing: the multi-ethnic study of atherosclerosis. Sleep Med 26:46–53. https://doi.org/10.1016/j.sleep.2015.06.003
Eckert DJ (2018) Phenotypic approaches to obstructive sleep apnoea–new pathways for targeted therapy. Sleep Med Rev 37:45–59
Lee RW, Sutherland K, Sands SA, Edwards BA, Chan TO, SS NG S, Hui DS, Cistulli PA (2017) Differences in respiratory arousal threshold in Caucasian and Chinese patients with obstructive sleep apnoea. Respirology 22(5):1015–1021. https://doi.org/10.1111/resp.13022
O’Driscoll DM, Landry SA, Pham J, Young A, Sands SA, Hamilton GS, Edwards BA (2019) The physiological phenotype of obstructive sleep apnea differs between Caucasian and Chinese patients. Sleep 42(11). https://doi.org/10.1093/sleep/zsz186
Villaneuva AT, Buchanan PR, Yee BJ, Grunstein RR (2005) Ethnicity and obstructive sleep apnoea. Sleep Med Rev 9(6):419–436. https://doi.org/10.1016/j.smrv.2005.04.005
Kong T, Chen Y, Guo Y, Wei Y, Jin X, Xie T, Mu Y, Dong Q, Wen S, Zhou B, Zhang L, Shen C, Zhu B (2017) Autosomal InDel polymorphisms for population genetic structure and differentiation analysis of Chinese Kazak ethnic group. Oncotarget 8(34):56651–56658. https://doi.org/10.18632/oncotarget.17838
Yang CH, Yin CY, Shen CM, Guo YX, Dong Q, Yan JW, Wang HD, Zhang YD, Meng HT, Jin R, Chen F, Zhu BF (2017) Genetic variation and forensic efficiency of autosomal insertion/deletion polymorphisms in Chinese Bai ethnic group: phylogenetic analysis to other populations. Oncotarget 8(24):39582–39591. https://doi.org/10.18632/oncotarget.17137
Kaparianos A, Sampsonas F, Karkoulias K, Spiropoulos K (2006) Obstructive sleep apnoea syndrome and genes. Neth J Med 64(8):280–289
Acknowledgements
The authors gratefully acknowledge Dr. Naichuan Su, Department of Oral Public Health, Academic Centre for Dentistry Amsterdam (ACTA), for his assistance with the statistical analyses of this study.
Funding
This work was supported by the Royal Netherlands Academy of Arts and Sciences (KNAW; 530-5CDP12), and the Young Clinical Research Fund of the Chinese Stomatological Association (CSA-O2022-08). Xiaoxin Shi has received a scholarship from the China Scholarship Council.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study received ethical approvals from the Netherlands (Amsterdam University Medical Center, reference number NL44085.018.13/COSH), and China (Dental School of Shandong University, reference number NO.GR201814).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
Xiaoxin Shi declares that she has no conflicts of interest. Hui Chen declares that she has no conflicts of interest. Frank Lobbezoo is a member of the Academic Advisory Boards for GrindCare and Oral Function of Sunstar Suisse S.A. and receives research grants from Sunstar Suisse S.A., SomnoMed, Vivisol BV, Health Holland, and Airway Management. Jan de Lange declares that he has no conflicts of interest. Paul van der Stelt declares that he has no conflicts of interest. Erwin Berkhout declares that he has no conflicts of interest. Jing Guo declares that she has no conflicts of interest. Shaohua Ge declares that she has no conflicts of interest. Guoju Li declares that she has no conflicts of interest. Yanzhong Li declares that he has no conflicts of interest. Ghizlane Aarab is a member of the Academic Advisory Board for Oral Function of Sunstar Suisse S.A. and receives research grants from Sunstar Suisse S.A., SomnoMed, Vivisol BV, and Health Holland.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shi, X., Chen, H., Lobbezoo, F. et al. Comparison of the upper airway morphology between Dutch and Chinese adults with obstructive sleep apnea. Sleep Breath 27, 2223–2230 (2023). https://doi.org/10.1007/s11325-023-02834-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02834-z