Abstract
Purpose
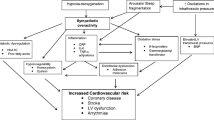
Obstructive sleep apnea (OSA) is the most prevalent sleep-related breathing disorder, with a negative impact on cardiovascular health. Different OSA symptoms and treatment response in males and females have been reported. The aim of this study was to investigate inflammatory markers in patients with OSA and the relationship of those markers to disease severity in male and female subjects.
Methods
We considered consecutive subjects referred to the outpatient Sleep Disorder Service of the Respiratory Medicine Department, San Marino Hospital. We included patients with a diagnosis of moderate or severe OSAS and an age range of 45–80 years. Concomitant inflammatory conditions were an exclusion criterion. A polygraphic study and a blood draw for inflammatory markers were performed for each subject.
Results
Of 110 subjects, 59 were males. Severe OSA affected 72 subjects. We analyzed data through a 4-level categorical variable according to sex and OSA severity (moderate OSA, males; severe OSA, males; moderate OSA, females; severe OSA, females), which showed significant differences for interleukin-6 (IL-6) and C-reactive protein (CRP) levels. A significant difference in IL-6 levels with a significant ascending trend (p = 0.045) from females with moderate OSAS to males with severe OSAS emerged in our pairwise comparison for estimated marginal means. Also, a significant trend (p = 0.0001) for CRP levels from males with moderate OSAS to females with severe OSAS was shown.
Conclusions
OSA and inflammation are interconnected, and both are associated with vascular diseases. Sex-related differences in OSA phenotypes may help the clinicians aim for a more personalized approach.


Similar content being viewed by others
Data availability
All data are available upon request.
Code availability
Not applicable.
References
Salman LA, Shulman R, Cohen JB (2020) Obstructive sleep apnea, hypertension, and cardiovascular risk: epidemiology, pathophysiology, and management. Curr Cardiol Rep 22(2):6. https://doi.org/10.1007/s11886-020-1257-y
Dewan NA, Nieto FJ, Somers VK (2015) Intermittent hypoxemia and OSA: implications for comorbidities. Chest 147(1):266–274. https://doi.org/10.1378/chest.14-0500
Stöwhas AC, Lichtblau M, Bloch KE. Obstructive sleep apnea syndrome. Praxis (Bern 1994) 2019;108:111–117. doi: https://doi.org/10.1024/1661-8157/a003198.
Redline S, Kump K, Tishler PV, Browner I, Ferrette V (1994) Gender differences in sleep disordered breathing in a community-based sample. Am J Respir Crit Care Med 149(3 Pt 1):722–726. https://doi.org/10.1164/ajrccm.149.3.8118642
Poroyko VA, Carreras A, Khalyfa A et al (2016) Chronic sleep disruption alters gut microbiota, induces systemic and adipose tissue inflammation and insulin resistance in mice. Sci Rep 6:35405. https://doi.org/10.1038/srep35405
Nadeem R, Molnar J, Madbouly EM et al (2013) Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med 9(10):1003–1012. https://doi.org/10.5664/jcsm.3070
Rocchi C., Conti V., Totaro V., Broggi S., Lattanzi S., Viticchi G., et al. (2021). Sex related differences in inflammation markers in adult patients with obstructive sleep apnea. WCN 2021 online. Meeting Abstracts ID 3506. doi.org/https://doi.org/10.1016/j.jns.2021.118667
Buysse DJ, Reynolds CF, Monk TH et al (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545. https://doi.org/10.1093/sleep/14.6.540
Ridker PM (2007) C-reactive protein and the prediction of cardiovascular events among those at intermediate risk: moving an inflammatory hypothesis toward consensus. J Am Coll Cardiol 49:2129–2138. https://doi.org/10.1016/j.jacc.2007.02.052
Gaines J, Vgontzas AN, Fernandez-Mendoza J, Kritikou I, Basta M, Bixler EO (2015) Gender differences in the association of sleep apnea and inflammation. Brain Behav Immun 47:211–217. https://doi.org/10.1016/j.bbi.2014.11.013
Li K, Wei P, Qin Y, Wei Y (2017) Is C-reactive protein a marker of obstructive sleep apnea?: a meta-analysis. Medicine (Baltimore) 96(19):e6850. https://doi.org/10.1097/MD.0000000000006850
Khera A, McGuire DK, Murphy SA, Stanek HG, Das SR, Vongpatansin W, Wians FH, Grundy SM, de Lemos JA (2005) Race and gender differences in C-reactive protein levels. J Am Coll Cardiol 46:464–469. https://doi.org/10.1016/j.jacc.2005.04.051
Doran B, Zhu W, Muennig P (2013) Gender differences in cardiovascular mortality by C- reactive protein level in the United States. Am Heart J 166:45–51. https://doi.org/10.1016/j.ahj.2013.03.017
Imani MM, Sadeghi M, Khazaie H, Emami M, Sadeghi Bahmani D, Brand S (2020) Evaluation of serum and plasma interleukin-6 levels in obstructive sleep apnea syndrome: a meta-analysis and meta-regression. Front Immunol 11:1343. https://doi.org/10.3389/fimmu.2020.01343
Baessler A, Nadeem R, Harvey M, Madbouly E, Younus A, Sajid H, Naseem J, Asif A, Bawaadam H (2013) Treatment for sleep apnea by continuous positive airway pressure improves levels of inflammatory markers—a meta-analysis. J Inflamm (Lond) 10:13. https://doi.org/10.1186/1476-9255-10-13
Bonsignore MR, Saaresranta T, Riha RL (2019) Sex differences in obstructive sleep apnoea. Eur Respir Rev 28(154):190030. https://doi.org/10.1183/16000617.0030-2019
Hirotsu C, Albuquerque RG, Nogueira H, Hachul H, Bittencourt L, Tufik S, Andersen ML (2017) The relationship between sleep apnea, metabolic dysfunction, and inflammation: the gender influence. Brain Behav Immun 59:211–218. https://doi.org/10.1016/j.bbi.2016.09.005
Meier-Ewert HK, Ridker PM, Rifai N, Price N, Dinges DF, Mullington JM (2001) Absence of diurnal variation of C-reactive protein concentrations in healthy human subjects. Clin Chem 47:426–430
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A et al (2001) Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med 163(3 Pt 1):608–613. https://doi.org/10.1164/ajrccm.163.3.9911064
Tishler PV, Larkin EK, Schluchter MD, Redline S (2003) Incidence of sleep-disordered breathing in an urban adult population: the relative importance of risk factors in the development of sleep-disordered breathing. The Journal of the American Medical Association 289(17):2230–2237. https://doi.org/10.1001/jama.289.17.2230
Ley CJ, Lees B, Stevenson JC (1992) Sex- and menopause-associated changes in body-fat distribution. Am J Clin Nutr 55:950–954. https://doi.org/10.1093/ajcn/55.5.950
Zhang Z, Cheng J, Yang W, Zou H, Su C, Miao J (2020) Gender differences in clinical manifestations and polysomnographic findings in Chinese patients with obstructive sleep apnea. Sleep Breath 24(3):1019–1026. https://doi.org/10.1007/s11325-019-01943-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study conforms to the Declaration of Helsinki and later amendments and was approved by the Ethics Committee of the Marche Polytechnic University.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Patients signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The paper was presented as an “Abstract only” at XXV World Congress of Neurology, October 3–7, 2021, Virtual.
Rights and permissions
About this article
Cite this article
Rocchi, C., Valentina, C., Totaro, V. et al. Inflammation markers in moderate and severe obstructive sleep apnea: the influence of sex. Sleep Breath 26, 1703–1709 (2022). https://doi.org/10.1007/s11325-021-02537-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02537-3