Abstract
Background
Considering socioeconomic status (SES) in the diagnosis of obstructive sleep apnea (OSA) will enhance our understanding of socioeconomic disparities in clinical practice of sleep medicine. This systematic review analyzes the relations between SES and OSA measures.
Methodology
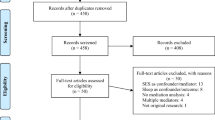
Eleven articles were identified through the Pubmed database. The National Institute of Health’s Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was used to rate the quality of these studies.
Results
This systematic review revealed that associations between socioeconomic status and OSA measures are similar for both adults, children, and adolescents. Our findings showed that: (1) A lower SES is associated with an increased risk of OSA, both in adults and children/adolescents as well as for men and women. (2) Several studies assessed sleep outcomes with a single question, an approach that is unable to capture the multi-dimensionality and day-to-day variability of sleep in general or OSA in particular, (3) Low SES has detrimental effects on sleep health. (4) Sleep questionnaires are more commonly used than objective measure to assess OSA.
Conclusions
Interaction between SES and OSA must be better understood to improve current clinical guidelines. Living conditions influence the trajectory of OSA with unknown speed and for an, undetermined period, pointing to the need for more studies on this topic. Future work should identify the effect of SES on the development and progression of OSA, determine the effect of behavioral intervention and local public health programs to reduce social inequalities associated with OSA.

Similar content being viewed by others
References
Anders MP, Breckenkamp J, Blettner M, Schlehofer B, Berg-Beckhoff G (2014) Association between socioeconomic factors and sleep quality in an urban population-based sample in Germany. Eur J Pub Health 24(6):968–973. https://doi.org/10.1093/eurpub/ckt175
Fang SC, Subramanian SV, Piccolo R, Yang M, Yaggi HK, Bliwise DL, Araujo AB (2015) Geographic variations in sleep duration: a multilevel analysis from the Boston area community health (BACH) survey. J Epidemiol Community Health 69(1):63–69. https://doi.org/10.1136/jech-2013-203256
Gosling JA, Batterham PJ, Glozier N, Christensen H (2014) The influence of job stress, social support and health status on intermittent and chronic sleep disturbance: an 8-year longitudinal analysis. Sleep Med 15(8):979–985. https://doi.org/10.1016/j.sleep.2014.04.007
Haba-Rubio J, Marti-Soler H, Tobback N, Andries D, Marques-Vidal P, Waeber G, Vollenweider P, von Gunten A, Preisig M, Castelao E, Tafti M, Heinzer R, Popp J (2017) Sleep characteristics and cognitive impairment in the general population: the HypnoLaus study. Neurology 88(5):463–469. https://doi.org/10.1212/wnl.0000000000003557
Hita-Yanez E, Atienza M, Gil-Neciga E, Cantero JL (2012) Disturbed sleep patterns in elders with mild cognitive impairment: the role of memory decline and ApoE epsilon4 genotype. Curr Alzheimer Res 9(3):290–297
Westerberg CE, Lundgren EM, Florczak SM, Mesulam MM, Weintraub S, Zee PC, Paller KA (2010) Sleep influences the severity of memory disruption in amnestic mild cognitive impairment: results from sleep self-assessment and continuous activity monitoring. Alzheimer Dis Assoc Disord 24(4):325–333. https://doi.org/10.1097/WAD.0b013e3181e30846
Moroni F, Nobili L, Curcio G, De Carli F, Fratello F, Marzano C, De Gennaro L, Ferrillo F, Cossu M, Francione S, Lo Russo G, Bertini M, Ferrara M (2007) Sleep in the human hippocampus: a stereo-EEG study. PLoS One 2(9):e867. https://doi.org/10.1371/journal.pone.0000867
De Gennaro L, Ferrara M, Spadini V, Curcio G, Cristiani R, Bertini M (2002) The cyclic alternating pattern decreases as a consequence of total sleep deprivation and correlates with EEG arousals. Neuropsychobiology 45(2):95–98. https://doi.org/10.1159/000048683
Babiloni AH, De Koninck BP, Beetz G, De Beaumont L, Martel MO, Lavigne GJ (2019) Sleep and pain: recent insights, mechanisms, and future directions in the investigation of this relationship. J Neural Transm:1–14
Fronczek R, van Geest S, Frolich M, Overeem S, Roelandse FW, Lammers GJ, Swaab DF (2012) Hypocretin (orexin) loss in Alzheimer's disease. Neurobiol Aging 33(8):1642–1650. https://doi.org/10.1016/j.neurobiolaging.2011.03.014
Young T, Peppard PE, Gottlieb DJ (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med 165(9):1217–1239
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235
DJ G, Yenokyan G, AB N, GT O C, NM P, SF Q (2010) Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure. Circulation 122:352–360
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342(19):1378–1384
Trayhurn P, Wang B, Wood IS (2008) Hypoxia in adipose tissue: a basis for the dysregulation of tissue function in obesity? Br J Nutr 100(2):227–235
Gorgone G, Ursini F, Altamura C, Bressi F, Tombini M, Curcio G, Chiovenda P, Squitti R, Silvestrini M, Ientile R (2009) Hyperhomocysteinemia, intima-media thickness and C677T MTHFR gene polymorphism: a correlation study in patients with cognitive impairment. Atherosclerosis 206(1):309–313
Peppard PE, Young T, Palta M, Dempsey J, Skatrud J (2000) Longitudinal study of moderate weight change and sleep-disordered breathing. Jama 284(23):3015–3021
Jordan AS, McSharry DG, Malhotra A (2014) Adult obstructive sleep apnoea. Lancet 383(9918):736–747
Ye L, Pien GW, Ratcliffe SJ, Weaver TE (2009) Gender differences in obstructive sleep apnea and treatment response to continuous positive airway pressure. J Clin Sleep Med 5(06):512–518
Doghramji PP (2008) Recognition of obstructive sleep apnea and associated excessive sleepiness in primary care. J Fam Pract 57(8):S17–S17
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. sleep 14(6):540–545
Iannella G, Vicini C, Colizza A, Meccariello G, Polimeni A, Greco A, de Vincentiis M, de Vito A, Cammaroto G, Gobbi R (2019) Aging effect on sleepiness and apneas severity in patients with obstructive sleep apnea syndrome: a meta-analysis study. Eur Arch Otorhinolaryngol:1–8
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213
Scarlata S, Pedone C, Curcio G, Cortese L, Chiurco D, Fontana D, Calabrese M, Fusiello R, Abbruzzese G, Santangelo S (2013) Pre-polysomnographic assessment using the Pittsburgh sleep quality index questionnaire is not useful in identifying people at higher risk for obstructive sleep apnea. J Med Screen 20(4):220–226
Jagannath A, Peirson SN, Foster RG (2013) Sleep and circadian rhythm disruption in neuropsychiatric illness. Curr Opin Neurobiol 23(5):888–894. https://doi.org/10.1016/j.conb.2013.03.008
Phelan JC, Link BG, Tehranifar P (2010) Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. Journal of health and social behavior 51 Suppl:S28–40. https://doi.org/10.1177/0022146510383498
Papadopoulos D, Sosso FAE, Khoury T, Surani SR (2020) Sleep disturbances are mediators between socioeconomic status and health: a scoping review. Int J Ment Heal Addict. https://doi.org/10.1007/s11469-020-00378-x
Rodriguez JM, Karlamangla AS, Gruenewald TL, Miller-Martinez D, Merkin SS, Seeman TE (2019) Social stratification and allostatic load: shapes of health differences in the MIDUS study in the United States. J Biosoc Sci 51(5):627–644. https://doi.org/10.1017/s0021932018000378
Mokarami H, Gharibi V, Kalteh HO, Faraji Kujerdi M, Kazemi R (2020) Multiple environmental and psychosocial work risk factors and sleep disturbances. Int Arch Occup Environ Health. https://doi.org/10.1007/s00420-020-01515-8
Wong K, Chan AHS, Ngan SC (2019) The effect of long working hours and overtime on occupational health: a meta-analysis of evidence from 1998 to 2018. Int J Environ Res Public Health 16(12). https://doi.org/10.3390/ijerph16122102
Yin J, Jin X, Shan Z, Li S, Huang H, Li P, Peng X, Peng Z, Yu K, Bao W, Yang W, Chen X, Liu L (2017) Relationship of sleep duration with all-cause mortality and cardiovascular events: a systematic review and dose-response meta-analysis of prospective cohort studies. J Am Heart Assoc 6(9). https://doi.org/10.1161/jaha.117.005947
Adams RJ, Piantadosi C, Appleton SL, Hill CL, Visvanathan R, Wilson DH, McEvoy RD (2012) Investigating obstructive sleep apnoea: will the health system have the capacity to cope? A population study. Aust Health Rev 36(4):424–429. https://doi.org/10.1071/ah11098
Mayne SL, Mitchell JA, Virudachalam S, Williamson AA (2020) 0397 Neighborhood Physical and Social Environments and Sleep Among Children and Adolescents: A Systematic Review. Sleep 43 (Supplement_1):A152-A152. https://doi.org/10.1093/sleep/zsaa056.394
Etindele-Sosso FA (2020) Insomnia, excessive daytime sleepiness, anxiety, depression and socioeconomic status among customer service employees in Canada. Sleep science (Sao Paulo, Brazil) 13 (1):54–64. https://doi.org/10.5935/1984-0063.20190133
Petrovic D, Haba-Rubio J, Carmeli C, Vollenweider P, Heinzer R, Stringhini S (2019) Social inequalities in sleep-disordered breathing: Evidence from the CoLaus|HypnoLaus study. Journal of sleep research 28 (5):e12799. https://doi.org/10.1111/jsr.12799
Mai QD, Hill TD, Vila-Henninger L, Grandner MA (2019) Employment insecurity and sleep disturbance: evidence from 31 European countries. J Sleep Res 28(1):e12763
National Heart L (2014) Institute B. National Institutes of Health, Department of Health and Human Services, Quality assessment tool for observational cohort and cross-sectional studies. Bethesda
Li X, Sundquist K, Sundquist J (2008) Socioeconomic status and occupation as risk factors for obstructive sleep apnea in Sweden: a population-based study. Sleep Med 9(2):129–136. https://doi.org/10.1016/j.sleep.2007.02.003
Reddy EV, Kadhiravan T, Mishra HK, Sreenivas V, Handa KK, Sinha S, Sharma SK (2009) Prevalence and risk factors of obstructive sleep apnea among middle-aged urban Indians: a community-based study. Sleep Med 10(8):913–918. https://doi.org/10.1016/j.sleep.2008.08.011
Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR (2010) Obstructive sleep apnea syndrome in the Sao Paulo epidemiologic sleep study. Sleep Med 11(5):441–446. https://doi.org/10.1016/j.sleep.2009.10.005
Amra B, Farajzadegan Z, Golshan M, Fietze I, Penzel T (2011) Prevalence of sleep apnea-related symptoms in a Persian population. Sleep Breath 15(3):425–429. https://doi.org/10.1007/s11325-010-0353-4
Wall H, Smith C, Hubbard R (2012) Body mass index and obstructive sleep apnoea in the UK: a cross-sectional study of the over-50s. Primary care respiratory journal : journal of the General Practice Airways Group 21 (4):371–376. https://doi.org/10.4104/pcrj.2012.00053
Ansarin K, Sahebi L, Sabur S (2013) Obstructive sleep apnea syndrome: complaints and housing characteristics in a population in the United States. Sao Paulo medical journal = Revista paulista de medicina 131 (4):220–227. https://doi.org/10.1590/1516-3180.2013.1314451
Kang K, Seo JG, Seo SH, Park KS, Lee HW (2014) Prevalence and related factors for high-risk of obstructive sleep apnea in a large korean population: results of a questionnaire-based study. J Clin Neurol 10(1):42–49. https://doi.org/10.3988/jcn.2014.10.1.42
Seyedmehdi SM, Rahnama N, Yazdanparast T, Jamaati H, Attarchi M, Adimi Naghan P, Hassani S (2016) Prevalence of snoring and the risk of sleep apnea in hospital staff. Work 55(4):765–772. https://doi.org/10.3233/wor-162460
Foroughi M, Malekmohammad M, Sharafkhaneh A, Emami H, Adimi P, Khoundabi B (2017) Prevalence of obstructive sleep apnea in a high-risk population using the stop-bang questionnaire in Tehran, Iran. Tanaffos 16(3):217–224
Goyal A, Pakhare AP, Bhatt GC, Choudhary B, Patil R (2018) Association of pediatric obstructive sleep apnea with poor academic performance: A school-based study from India. Lung India 35 (2):132–136. https://doi.org/10.4103/lungindia.lungindia_218_17
Krysta K, Bratek A, Zawada K, Stepańczak R (2017) Cognitive deficits in adults with obstructive sleep apnea compared to children and adolescents. J Neural Transm 124(1):187–201
Cardoso TSG, Pompeia S, Miranda MC (2018) Cognitive and behavioral effects of obstructive sleep apnea syndrome in children: a systematic literature review. Sleep Med 46:46–55
Hunter SJ, Gozal D, Smith DL, Philby MF, Kaylegian J, Kheirandish-Gozal L (2016) Effect of sleep-disordered breathing severity on cognitive performance measures in a large community cohort of young school-aged children. Am J Respir Crit Care Med 194(6):739–747
O'Brien LM, Gozal D (2002) Behavioural and neurocognitive implications of snoring and obstructive sleep apnoea in children: facts and theory. Paediatr Respir Rev 3(1):3–9
Saint Martin M, Sforza E, Roche F, Barthelemy JC, Thomas-Anterion C (2015) Sleep breathing disorders and cognitive function in the elderly: an 8-year follow-up study. The proof-synapse cohort. Sleep 38(2):179
Bucks RS, Olaithe M, Eastwood P (2013) Neurocognitive function in obstructive sleep apnoea: a meta-review. Respirology 18(1):61–70
Rezaeitalab F, Moharrari F, Saberi S, Asadpour H, Rezaeetalab F (2014) The correlation of anxiety and depression with obstructive sleep apnea syndrome. Journal of research in medical sciences: the official journal of Isfahan University of Medical Sciences 19(3):205
Leger D, Stepnowsky C (2020) The economic and societal burden of excessive daytime sleepiness in patients with obstructive sleep apnea. Sleep Med Rev 101275
Ribeiro AI, Amaro J, Lisi C, Fraga S (2018) Neighborhood socioeconomic deprivation and allostatic load: a scoping review. Int J Environ Res Public Health 15(6). https://doi.org/10.3390/ijerph15061092
Johnson SC, Cavallaro FL, Leon DA (2017) A systematic review of allostatic load in relation to socioeconomic position: poor fidelity and major inconsistencies in biomarkers employed. Soc Sci Med (1982 192:66–73. https://doi.org/10.1016/j.socscimed.2017.09.025
Meneton P, Hoertel N, Wiernik E, Lemogne C, Ribet C, Bonenfant S, Menard J, Goldberg M, Zins M (2018) Work environment mediates a large part of social inequalities in the incidence of several common cardiovascular risk factors: findings from the Gazel cohort. Soc Sci Med 216:59–66. https://doi.org/10.1016/j.socscimed.2018.09.042
Smagula SF, Koh WP, Wang R, Yuan JM (2016) Chronic disease and lifestyle factors associated with change in sleep duration among older adults in the Singapore Chinese health study. J Sleep Res 25(1):57–61. https://doi.org/10.1111/jsr.12342
Green MJ, Espie CA, Benzeval M (2014) Social class and gender patterning of insomnia symptoms and psychiatric distress: a 20-year prospective cohort study. BMC psychiatry 14:152. https://doi.org/10.1186/1471-244x-14-152
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Etindele Sosso, F., Matos, E. Socioeconomic disparities in obstructive sleep apnea: a systematic review of empirical research. Sleep Breath 25, 1729–1739 (2021). https://doi.org/10.1007/s11325-020-02274-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02274-z